Shoulder dislocation
| Classification according to ICD-10 | |
|---|---|
| S43.0 | Dislocation of the shoulder joint [glenohumeral joint] |
| M24.41 | Habitual dislocation and subluxation of a joint: shoulder region |
| Q68.8 | Other specified congenital musculoskeletal deformities - Congenital dislocation of the shoulder |
| ICD-10 online (WHO version 2019) | |
A shoulder dislocation or shoulder joint dislocation ( Latin luxatio humeri , luxatio glenohumeralis ) is a dislocation ( dislocation ) of the shoulder joint . The shoulder dislocation is one of the most common dislocations of the large joints. It can be caused by an accident (traumatic dislocation) or due to the patient's condition (habitual dislocation). Symptoms are restricted mobility in the shoulder joint, pain and a changed shoulder shape. After bone fractures have been ruled out by means of X-rays, the therapy is carried out by repositioning . Surgical therapy may be necessary in the event of complications and repeated dislocations.
to form
A traumatic dislocation is caused by a levering force applied to the extended arm, typically from the front with external rotation and abduction , such as, e.g. B. handball players with an outstretched limb or when catching a fall. The first dislocation usually occurs in young adults. After such trauma, recurrent dislocations can occur even with lower forces . The reasons for this are remaining damage to the capsule-ligament apparatus, tearing of the glenoid labrum ( Bankart lesion ), broken bones ( fractures as well as cartilage, muscle and nerve damage).
Predisposing factors are held responsible for the habitual dislocation , although the etiology and pathogenesis are still not fully understood. These can include anomalies of the joint capsule, malformations of the joint socket, weak connective tissue ( Ehlers-Danlos syndrome , Marfan syndrome ) or incorrect innervation of the muscles. The initial dislocation is usually directed forward and occurs predominantly in young patients without adequate trauma.
According to the direction of the dislocation, there are four different types of dislocation. The anterior shoulder dislocation (lat. Luxatio subcoracoidea ) is the most common shoulder dislocation with over 90%. A dislocation back and down is called a luxatio infraspinata . With the luxatio infraglenoidalis or axillary , the humerus head is dislocated downwards (lat. Caudal ). A rare dislocation is the luxatio erecta , in which the humerus head is also dislocated caudally with the arm also held vertically upwards.
Symptoms
The shoulder joint is resiliently fixed, there is spontaneous pain and pain when moving. In the anterior dislocation, the arm is usually in abduction and external rotation and is held with the sound arm. The shoulder contour is more angular because the deltoid muscle is stretched tightly over the acromion when the upper arm is shifted caudally . The joint socket is empty and the humeral head can usually be felt in the soft tissues below the outer clavicle . Damage to axillary vessels or nerves leads to disorders of blood flow, motor skills and sensitivity in the arm.
Diagnosis
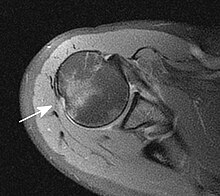
The basis is the anamnesis (accident mechanism) and physical examination (functional impairment). In particular, the damage to blood vessels and nerves must be observed and documented. The diagnosis is confirmed and a fracture ruled out by means of x-rays in different planes. An MRI image can be made to rule out a Bankart lesion (see below).
therapy
Any movement of the arm should be avoided as part of first aid (immobilization). Local cooling can relieve the resulting swelling and pain. In principle, the rescue service should be alerted via an emergency call in order to be able to carry out gentle transport and any necessary treatment on site.
The relocation of the dislocation back from the outside without surgery is called closed reduction and should be done as quickly as possible, since the reduction becomes more difficult as the duration of the dislocation increases due to muscle tension and swelling. If nerves (especially the axillary nerve ) or vessels are pinched by the dislocation , delayed reduction can lead to permanent damage. In principle, the guidelines recommend restraint with immediate emergency repositioning at the scene of the accident, since an X-ray should first be taken in order to rule out an accompanying bone fracture. A blind attempt at repositioning an undetected bone fracture could lead to additional injuries.
It is therefore recommended in guidelines that the decision for or against an immediate attempt at reduction without a prior X-ray should depend on certain criteria in each individual case. A short transport time to the nearest suitable hospital, preserved blood circulation in the arm, preserved nerve functions and little experience of reduction on the part of the helper speak against attempting a reduction. An emergency reduction should be considered in the case of long transport times to the nearest hospital, circulatory disorders, nerve damage with sensory disturbances and an experienced helper on site.
In any case, if the patient is in pain, he or she should be given sufficient pain medication to alleviate the pain during transport or attempted reduction. Painkillers and, if necessary, additionally administered tranquilizers relax the muscles, which makes repositioning easier. In severe cases, even a brief anesthetic with complete muscle relaxation may be necessary to enable reduction.
The following manual techniques are used: With the Hippocratic reduction , the doctor exerts tension on the extended arm while placing his own foot as an abutment in the armpit of the patient. With the reduction according to Arlt , the pull is carried out with a chair back as an abutment, with the repositioning according to Kocher, the arm is reduced by adduction (elbow to the body) - external rotation - and elevation (lifting) with the help of the resulting leverage on the socket. Reduction requires analgesic sedation . The joint is then immobilized in a Gilchrist or Desault bandage for one to three weeks - depending on the severity, the cause of the dislocation and the circumstances . The duration of immobilization must be weighed against the associated risk of shoulder stiffness, which is more likely to be expected in older patients.
Indications for surgical therapy are unsuccessful closed repositioning, complications (vessel / nerve damage, Hill-Sachs lesion , Bankart lesion ) and recurrent dislocations. This can be done arthroscopically or openly , depending on the occasion .
Complications
A Hill-Sachs dent is a bone impression on the humeral head . It can be treated by relining with cancellous bone or a rotary osteotomy (according to Weber, only rarely used). A Bankart lesion is the tearing of the cartilaginous labrum glenoidale inferius from the socket. This can result in anterior shoulder instability. The operative therapy consists of an arthroscopic refixation ( Bankart repair ) or a reconstruction using a bone chip, e.g. B. Latarjet's technology. Both lesions are risk factors for the recurrence of further dislocations.
In a retrospective study at the Balgrist University Hospital in Zurich , the two methods of anterior shoulder stabilization were compared with one another. 93 shoulders were treated with a Latarjet operation, 271 shoulders received an arthroscopic Bankart repair . After just over ten years of follow-up after the operation, significantly fewer patients in the Latarjet group were dissatisfied with the result (3% versus 13%). A renewed shoulder dislocation occurred in 1% versus 13%, a subluxation in 2% versus 19%, and subjective instability complained about 11% versus 42%. Due to instability, 1% versus 21% had to undergo another intervention.
In addition, accompanying injuries to bones, vessels and nerves or the rotator cuff can occur.
literature
- JR Siewert: Surgery. 7th edition. Springer, Berlin 2001, ISBN 3-540-67409-8 .
- A. Ficklscherer: BASICS Orthopedics and Trauma Surgery. Elsevier, 2012, ISBN 978-3-437-42208-9 .
- S1 guideline (PDF; 702 kB) "Shoulder dislocation, recurrent and habitual" of the German Society for Orthopedics and Orthopedic Surgery and the Professional Association of Orthopedic Doctors , last updated in 2009
Web links
Individual evidence
- ↑ M. Holland, T. Pohlemann: shoulder and shoulder girdle . In: H.-P. Scharf, A. Rüter (Ed.): Orthopedics and trauma surgery . Specialist knowledge according to the new training regulations. 1st edition. Urban & Fischer - Elsevier, Munich 2009, ISBN 978-3-437-24400-1 , 24.6, pp. 464 ff .
- ↑ AWMF online: Guidelines of the German Society for Trauma Surgery: First shoulder dislocation. Working Group of Scientific Medical Societies, AWMF Guideline Register No. 012/012, Development Stage 1
- ↑ Stefan M. Zimmermann, Max J. Scheyerer, Mazda Farshad, Sabrina Catanzaro, Stefan Rahm, Christian Gerber : Long-term restoratio of anterior shoulder stability: A retrospective Analysis of artrhoscopic Bankart repair versus open Latarjet procedure . The Journal of Bone & Joint Surgery 2016, Volume 98-A, Issue 23, December 7, 2016, pages 1954-1961; DOI: 10.2106 / JBJS.15.01398