Rotator cuff rupture
| Classification according to ICD-10 | |
|---|---|
| M75 | Shoulder lesions |
| M75.1 | Rotator cuff lesions |
| S46 | Injury to muscles and tendons at shoulder and upper arm level |
| S46.0 | Injury to the muscles and tendons of the rotator cuff |
| ICD-10 online (WHO version 2019) | |
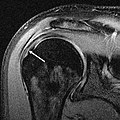
MRI of a complete rupture
As a rotator cuff tear , the rupture (rupture) of one or more muscles or tendons of the rotator cuff , a group of muscles in the shoulder region , respectively. The lesion (damage) can have traumatic (accident-related) or degenerative (wear- related ) causes. Depending on its extent, the rotator cuff rupture leads to a more or less pronounced functional disorder up to and including loss of function of the affected shoulder joint .
Anatomy of the shoulder joint
The human shoulder joint is the only joint that is mainly muscle-stabilized, since the ligaments of the shoulder joint are of little importance for its stability. The upper end of the humerus, the humerus head, consists of an almost exact 3/4 ball. This ball is held in the joint socket of the shoulder by a total of four muscles , which is formed by the joint part of the shoulder blade and the outer part of the collarbone , and at the same time its mobility is guided. These four muscles and their tendons are called the rotator cuff; these are the supraspinatus , subscapularis , infraspinatus and teres minor muscles . The glenoid lip ( labrum glenoidale ) of the joint socket is also important for stabilizing the shoulder joint.
As a functional ball joint , the shoulder joint has all three possibilities of movement ( degrees of freedom ). These are elevation / retroversion (lifting / backward movement), abduction / adduction (spreading / bending) and rotation (turning). There is no direct bony connection to the trunk skeleton: the connecting links to the trunk are formed by the shoulder blade and the clavicle , apart from the sternoclavicular joint , the connections between these bones and the trunk skeleton consist only of muscles and connective tissue ligament structures.
Disease mechanism
In the etiology of the rotator cuff rupture, a distinction is made between “extrinsic” (externally acting) and “ intrinsic ” (resulting from structural changes) factors in their development. While the acute ruptures in younger ages (under 40 years of age) are usually based on accidental injuries, i.e. purely extrinsic factors, the ruptures with advancing age are increasingly due to a "multifactorial" event: Both degenerative and traumatic processes are involved in the development . A special case are antibiotics from the group of fluoroquinolones , which can cause degenerative damage to the rotator cuff due to their tendotoxic properties. In this context, ruptures and tendopathies of the supraspinatus tendon have primarily been reported; the subscapularis tendon is more rarely affected. The Food and Drug Administration (FDA) drew attention to the first cases of fluoroquinolone-induced rotator cuff ruptures as early as 1995.
Acute rupture
In the event of a fall on the arm stretched backwards or the action of levering force on the fixed upper arm, shoulder dislocation (dislocation of the humerus head from the shoulder joint) can occur. This dislocation does not necessarily mean that the stabilizing structures are destroyed or cracked. The muscles belonging to the rotator cuff, in particular, can often withstand overstretching without damage due to their elasticity. Correctly performed reduction of the shoulder joint can thus enable undisturbed healing. However, the dislocation of the shoulder often leads to further injuries: In the course of the dislocation , the anterior lower joint capsule and its ligaments can be torn, the acetabular lip in the lower area tears off ( Bankart lesion ), and rarely the edge of the acetabulum also breaks off there (bony Bankart lesion) and / or pressure damage to the joint head ( Hill-Sachs lesion ) occurs. Depending on the severity of the trauma, the rotator cuff muscles or their tendons can also tear or tear off. Depending on the affected muscle, certain movements in the shoulder joint cannot be carried out or only to a limited extent. A complete rotator cuff rupture is the result of a traumatic initial dislocation in around a quarter of the cases in younger patients.
Also SLAP lesions , that violations of the pan lip at the top of the socket, often occur in combination with a rotator cuff tear and can lead to instability of the shoulder joint. Such a SLAP lesion can be caused by a sudden and unexpected pull or pressure on the already pre-tensioned long biceps tendon (lifting of heavy objects, strong winds while windsurfing, corresponding fall on the arm).
Compared to the far more frequent rotator cuff ruptures, which arise due to chronic damage to the shoulder joint, the number of acute traumatic ruptures is of minor importance.
Only those ruptures that are based on an adequate accident mechanism are referred to as traumatic rotator cuff ruptures. Such is the case:
- Passively forced external or internal rotation with the arm lying flat or spread apart
- passive traction in caudal , ventral or medial direction
- axial compression cranioventrally or ventromedially
Degenerative rupture
After injuries to the shoulder joint or possibly only due to advancing age, the cartilage substance and the strength of the tendons of the rotators can be lost. This is often shown by calcification of the subscapularis tendon, which can be seen in the X-ray image by calcified shadows . The supraspinatus muscle, which is most frequently involved in rotator cuff rupture, even if it is isolated, can be literally "crushed". In such a case, the X-ray image shows a reduced distance between the shoulder joint and the humerus head as an indication of an impingement syndrome. Other muscles and especially tendons can also be involved in this degenerative process. This can particularly affect the long biceps tendon , which is pinched in the joint space and “rubbed open” ( pulley lesion ).
If the structures of the rotator cuff are damaged by these aging and wear processes, “inadequate” trauma (i.e. injuries whose intensity could not cause significant damage to healthy young people) can lead to a rupture of the rotator cuff. In extreme cases, wide tears in the supraspinatus, infraspinatus and subscapularis muscles occur. The teres minor is rarely involved in the rupture.
Inadequate traumas are
- Craniodorsal or medial compression
- direct impact trauma
- active physical exertion
frequency
There are a large number of studies on the frequency of rotator cuff ruptures in the population (“ prevalence ”), some of which have significantly different results. Statistics compiled on the basis of autopsies give figures from 5 to 39 percent. The information on the frequency of rotator cuff ruptures in relation to age is just as varied, with most studies showing an increase in the disease with increasing age; however, there is no definite correlation between these findings and the clinical symptoms. However, the view that was widespread until a few decades ago that the rotator cuff rupture is a fateful old age disease, the surgical treatment of which is not necessary, is refuted by numerous studies.
Diagnosis
Physical examination
Acute accidental injuries, whether associated with a dislocation or not, usually result in pain of varying intensity, soft tissue swelling and restricted mobility: the range of motion of the shoulder can no longer be accessed painlessly even passively ( painful arc ). If the rotator cuff is torn, the abduction (lateral lifting of the arm) in particular, and in addition usually the elevation (lifting of the arm forwards) can no longer be performed - or no longer painlessly.
The main characteristic of degenerative ruptures is the pain symptoms associated with a loss of strength, especially with greater stress and overhead work. Long-term pain can occur later, which is often felt to be unbearable mostly at night, and lying on the affected side is then no longer possible. In addition, with certain movements, for example the lateral spreading of the upper arm, suddenly shooting stabbing pain occurs, which makes it impossible to continue the movement. With a decrease in muscle mass and muscle strength, there is increasing stiffening in the shoulder joint up to the clinical picture of the frozen shoulder .
However, the clinical examinations only provide a rough overview of the damage present. However, the findings described give cause for further diagnostics.
Differential diagnoses
Shoulder pain can be manifestations of various other diseases: if the pain spreads to the fingers with sensory disturbances in the hand area, then the cause may be found in wear damage to the cervical spine . Typical night pain also occurs with carpal tunnel syndrome , here the pain occasionally radiates from the hand to the shoulder of the affected side. Inflammatory nerve diseases such as acute neuritis of the brachial plexus can also lead to movement-dependent neck, shoulder and arm pain.
roentgen
The devastating damage to the rotator cuff can only rarely be seen so clearly in a simple X-ray image (see picture). The impingement shown here speaks for a largely complete degeneration of the rotator cuff, the subacromial bursa is completely destroyed. The joint contours of the humerus head, but also the X-ray structure of the joint socket, already show the characteristics of a progressive osteoarthritis .
Sonography
The ultrasound is considered as a method for initial examination, since it is an inexpensive and widely available technology. A meta-analysis showed a sensitivity (hit rate) of 67% and a specificity of 94% for the detection (detection) of partial cracks ; for complete cracks there was a sensitivity of 92% and a specificity of 94%.
Ultrasound can show the tear directly as a hypoechoic region or lack of tendon fibers as well as indirect signs that indicate a tendon tear: The latter include a flattening of the tendon, irregular surface of the bony protrusions ( tuberculi ) on the humerus, and an echogenic line along the cartilage ( cartilage interface sign ). A effusion in the shoulder joint , the bursa subacromial -subdeltoidea below the Grätenecks the scapula and the deltoid muscle and the tendon sheath of the biceps suggest the suspicion of a rotator cuff tear.
Magnetic resonance arthrography
The magnetic resonance imaging , possibly with intraarticular (directly administered into the joint) administration of contrast medium ( "MR arthrography "), shows very accurately destroyed structures and is now one of the standard tests in the shoulder joint lesions.
Classification and division
Various classification systems have been proposed to facilitate the planning of a possible operative approach, but also for scientific investigations . Among other things , the classification according to Bateman , published as early as 1920, which classifies the rupture into four different degrees according to the defect width in centimeters, is used to classify complete ruptures . According to Ellman , incomplete ruptures ( "partial ruptures " ) are classified according to the relative size of the tear in relation to the total tendon diameter. A systematic, comparative overview of the various classification systems was published by CH Krieter in 2008 as part of a dissertation.
treatment
There are basically several options available for treating a rotator cuff rupture:
The rare, purely traumatic rupture of the rotator cuff is usually treated surgically as soon as possible through primary tendon sutures. But older traumatic or degenerative ruptures can also be treated with the help of modern surgical techniques. The decisive factors for the indication for an operative intervention are the age, the functional deficit and the subjective suffering of the patient concerned.
Surgical treatment
Arthroscopy
The arthroscopy of the shoulder joint is usually the surgical treatment of rotator cuff tears start. Despite the generally reliable diagnosis with the help of the above-mentioned imaging methods , more extensive arthroscopic findings can often be made. On the one hand, this concerns the extent of the lesion and, on the other hand, the assessment of joint damage that goes beyond the rotator cuff rupture or is independent of it ( omarthrosis , Bankart lesion, Hill-Sachs defect, pulley lesion, rupture of the long biceps tendon, subacromial impingement, etc.) .). These accompanying damage can in some cases be treated more effectively with an arthroscopic approach than with open surgery. The arthroscopic stabilization of a Bankart lesion, the removal of the stump of a rupture of the long biceps tendon, the smoothing of cartilage fractures and the decompression of the subacromial bursa come into question here .
The arthroscopic assessment also serves to confirm the indication for a reconstruction of the rotator cuff. For example, high-grade osteoarthritis of the shoulder joint with extensive loss of the cartilage substance on the joint head and socket makes an expensive restoration of the rotator cuff seem pointless. In such cases, functional improvement through surgical intervention is not to be expected.
The rotator cuff defect is immediately visible through arthroscopy. Advances in arthroscopic surgical technology make arthroscopic or arthroscopically assisted reconstruction of older and / or extensive ruptures possible. Various procedures and instruments have been developed for this purpose. So-called “suture anchors” made of metal or absorbable plastic material can be inserted into the attachment area of the tendons on the humerus head, to which the muscle / tendon stumps can be fixed under arthroscopic view. As with the open surgical transosseous suturing method (see below), the success of the operation is primarily dependent on how far the stumps have already been retracted and changed in a fatty degenerative way. In addition, the surgeon's personal experience and technical skills, and not least the equipment, are decisive for successful arthroscopic reconstruction.
Direct seam
The rotator cuff tear is usually in the transition area between the muscle and the tendon. The natural basic tension of the muscles and their tendons means that direct seams in the muscle area can tear out even if the joint is effectively immobilized. In older ruptures, the affected muscle is usually "shrunk", i.e. shortened, which means that a direct suture is always under significant tension. This regularly leads to " insufficiency " (weakening) of such seams; they cut through the tissue and become ineffective before solid scarring in the tear area can stabilize the rotator cuff. Therefore, performing a simple, direct tendon / muscle suture is only recommended for fresh, usually traumatic ruptures: here the tear can be adapted with little tension and - as long as it has not yet been retracted and degenerated - it can be bridged very quickly with stable scar tissue.
Open surgical reconstruction
For the reconstruction of older ruptures, if arthroscopic restoration does not appear possible or sensible for the reasons mentioned above, procedures are used that fix the affected tendon / muscle stumps in the bone of the humerus head, more precisely in the area of the greater tuberosity, using an open surgical technique. This technique is called “transosseous” (“leading through the bone” - Latin trans , “over, through”, os “the bone”) suturing technique. For this purpose, several - usually two to three - special metal screws are inserted into the head of the humerus, to which the tendon stumps are anchored via further small bone holes using strong sutures. The contact of the tendon stumps with the additionally “roughened” bone leads to the formation of a significantly more stable scar than can be achieved with direct suturing.
This procedure is used when the muscles have already shrunk in the case of long-standing tears and the stumps consist of scar tissue that is not very stable and no longer capable of regeneration, or when muscles and tendons rupture that were "worn out" before the injury.
In the case of very extensive, combined defects of the supra- and infraspinatus tendons in younger, physically active patients, complex plastic-surgical reconstruction procedures in the sense of a "muscle transfer operation" (relocation of the latissimus dorsi muscle ) are also used. In the event of an irreparable rupture of the subscapularis muscle with repeated forward dislocation of the shoulder, an improvement can be achieved by transferring the pectoralis tendon .
Aftercare
The aim of the follow-up treatment is to restore the continuity of injured tendons and muscles. Since stable and resilient scar tissue can only be expected to develop six weeks after the operation at the earliest, immobilization in a suitable abduction bandage takes place during this time . This consists of a soft wedge with an angle of about 45 °, which is carried under the armpit of the affected shoulder and held in position with Velcro fasteners. Passive movement and pendulum exercises can and should begin during this rest period. These are even essential to prevent stiffening of the shoulder. After six weeks at the earliest, the patient begins active movement exercises, initially in the sense of pendulum exercises with the hanging arm, later increasing abduction, elevation and rotation exercises. The physiotherapy and physiotherapy treatment is complex and must be continued for months, in some cases years, in order to restore or maintain physical performance.
Conservative treatment
Non -steroidal anti-inflammatory drugs and cortisone injections can be used for drug treatment of ruptures . In some cases it is possible to treat ruptures with platelet-rich plasma .
Physical therapy is also used: fresh, traumatic ruptures are immobilized in the abduction bandage for the first six weeks, the physiotherapy exercise treatment is limited to passive movement and stress-free pendulum exercises. Old, degenerative lesions are subjected to individually adapted active and passive exercise treatment from the outset, if necessary with regional pain elimination .
forecast
Surgical restoration of degeneratively damaged rotator cuffs is accompanied by a considerable number of possible complications. Since the rotator cuff rupture is only one of several manifestations of degenerative shoulder diseases, even a technically flawless reconstruction can lead to a clinically unsatisfactory result.
The early complications during or shortly after the operation correspond to those of open joint surgery in all other areas. In addition to bruises (around 10%), wound infections (1.7%) and joint infections (around 1%) are rare. A special feature is the tear of the deltoid muscle , the occurrence of which is given as 8%.
In the late phase, the persistence of pain (17%) and muscle strength reduction predominate (25%). Clinically significant ruptures occur in 8%, sonographically detectable residual defects without clinical significance in 28% of the cases. Heterotopic ossifications (ossification of muscles and soft tissues) occur quite frequently at 26%, but their clinical significance cannot be derived from this figure. Arthrofibrosis (3%) and CRPS (less than 1%) are quantitatively insignificant . Arthrosis occurs in around 6% of cases, although it is not stated here whether this existed before the rotator cuff rupture occurred.
Assessment under social security law
The recognition under insurance law of a rotator cuff rupture as an occupational disease or classification as an occupational accident often turns out to be extremely problematic due to the often difficult assessment of combined traumatic and degenerative events. The disease is not explicitly listed as such in the Occupational Disease Ordinance (BKV), but in legal disputes it is often assigned to BK number 2101 BKV ("Diseases of the tendon sheaths or the tendon sliding tissue and the tendon and muscle attachments"). According to Section 9, Paragraph 2 of Book VII of the Social Code, a disease is "recognized as an occupational disease if, according to new findings in medical science, the other requirements of Paragraph 1 are met, but a corresponding disease has not yet been included in the list of occupational diseases", however such new medical-scientific findings have not yet been made.
Web links
- R. Sistermann: rotator cuff tears. Orthopädie Klinikum Dortmund , accessed on March 31, 2013 .
Individual evidence
- ↑ Jourdan M. Cancienne, Stephen F. Brockmeier, Scott A. Rodeo, Chris Young, Brian C. Werner: Early postoperative fluoroquinolone use is associated with an increased revision rate after arthroscopic rotator cuff repair . In: Knee Surgery, Sports Traumatology, Arthroscopy . tape 25 , no. 7 , July 1, 2017, ISSN 0942-2056 , p. 2189-2195 , doi : 10.1007 / s00167-016-4354-0 .
- ↑ Alice JS Fox, Michael O. Schär, Florian Wanivenhaus, Tony Chen, Erik Attia: Fluoroquinolones impair tendon healing in a rat rotator cuff repair model: a preliminary study . In: The American Journal of Sports Medicine . tape 42 , no. December 12 , 2014, ISSN 1552-3365 , p. 2851-2859 , doi : 10.1177 / 0363546514545858 , PMID 25143490 .
- ↑ Leonie Strobbe, Roger JM Brüggemann, Peter J. Donnelly, Nicole MA Blijlevens: A rare case of supraspinatus tendon rupture . In: Annals of Hematology . tape 91 , no. 1 , January 1, 2012, ISSN 0939-5555 , p. 131-132 , doi : 10.1007 / s00277-011-1220-5 .
- ↑ Walter de Araujo Eyer-Silva, Henrique de Barros Pinto Netto, Jorge Francisco da Cunha Pinto, Fernando Raphael de Almeida Ferry, Rogério Neves-Motta: Severe shoulder tendinopathy associated with levofloxacin . In: The Brazilian Journal of Infectious Diseases . tape 16 , no. 4 , 2012, p. 393-395 , doi : 10.1016 / j.bjid.2012.06.015 .
- ↑ BK Baddredine u. a .: Rupture de la coiffe des rotateurs secondaire à la prise des fluoroquinolones chez les patients hémodialysés. à propos de 2 cas. (PDF) La Tunisie Médicale, January 10, 2015, accessed on March 14, 2018 (French, English).
- ↑ JM Casparian, M. Luchi, RE Moffat, D. Hinthorn: Quinolones and tendon ruptures . In: Southern Medical Journal . tape 93 , no. 5 , May 2000, ISSN 0038-4348 , p. 488-491 , PMID 10832946 .
- ↑ More on Fluoroquinolone Antibiotics and Tendon Rupture . In: New England Journal of Medicine . tape 332 , no. 3 , January 19, 1995, ISSN 0028-4793 , p. 193-193 , doi : 10.1056 / nejm199501193320319 , PMID 7800022 .
- ↑ P. Habermeyer, S. Lichtenberg, P. Magosch: rotator cuff rupture and shoulder instability . In: Arthroscopy . Vol. 20, No. 3 , 2007, ISSN 0933-7946 , p. 217-222 , doi : 10.1007 / s00142-007-0405-3 .
- ↑ a b M. Loew u. a .: Recommendations for diagnosis and assessment of the traumatic rotator cuff lesion . In: The trauma surgeon . Volume 103, No. 5 , May 2000, ISSN 0177-5537 , p. 417-426 , doi : 10.1007 / s001130050560 .
- ↑ a b c d e f L. Lehmann, H.-P. Sharp: rotator cuff injuries . In: H.-P. Scharf, A. Rüter u. a. (Ed.): Orthopedics and trauma surgery . Specialist knowledge according to the new training regulations. 1st edition. Elsevier Urban & Fischer, Munich 2009, ISBN 978-3-437-24400-1 , 24.3, pp. 449-456 .
- ↑ B. Daenen, G. Houben, E. Bauduin, KV Lu, JL Meulemans: Ultrasound of the Shoulder. In: JBR-BTR. 2007, 90, pp. 325-337. PMID 18085186 , p. 325.
- ^ JO de Jesus, L. Parker, AJ Frangos, LN Nazarian: Accuracy of MRI, MR Arthrography, and Ultrasound in the Diagnosis of Rotator Cuff Tears: A Meta-Analysis. In: AJR. 2009; 192, pp. 1701-1707 PMID 19457838 , p. 1705.
- ↑ B. Daenen, G. Houben, E. Bauduin, KV Lu, JL Meulemans: Ultrasound of the Shoulder. In: JBR-BTR. 2007, 90, pp. 325-337. PMID 18085186 , p. 329.
- ^ EA Zimmer, A. Köhler: Limits of the normal and beginnings of the pathological in the radiology of the child and adult skeleton . 14. fully revised, restructured. and extended edition. Georg Thieme, Stuttgart 2000, ISBN 3-13-362214-5 , chap. Shoulder impingement and rotator cuff rupture , p. 294 ff .
- ^ J. Bateman: The Shoulder and Neck . In: WB Saunders (Ed.): The Shoulder and Neck . Philadelphia 1972, p. 213-235 .
- ^ H. Ellman: Arthroscopic Shoulder Surgey and Related Procedures . Ed .: LA Febiger. Philadelphia 1993, p. 8-99 .
- ^ CH Krieter: The arthroscopic classification of the articular-side rotator cuff partial ruptures . Inaugural dissertation to obtain the medical doctoral degree from the Ludwig Maximilians University in Munich. Munich 2008 ( here online (PDF; 4.1 MB) [accessed on March 31, 2013]).
- ↑ M. Loew: rotator cuff rupture . In: V. Ewerbeck u. a. (Ed.): Standard procedures in surgical orthopedics and trauma surgery . 3rd, completely revised edition. Georg Thieme Verlag, Stuttgart 2007, ISBN 3-13-100533-5 , chapter 6.6, p. 339 ff .
- ↑ Transosseous suturing techniques are also regularly used for other tendon tears close to the bone, for example a tear in the biceps tendon in the elbow area or quadriceps tendon ruptures .
- ^ RG Marx u. a .: Indications for Surgery in Clinical Outcome Studies of Rotator Cuff Surgery. In: Clin Orthop Relat Res. V.467 (2); Feb 2009 PMC 2628527 (free full text).
- ^ P. Maniscalco: The "Cascade" membrane: a new PRP device for tendon ruptures. Description and case report on rotator cuff tendon. ( Memento of the original from December 4, 2013 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF) In: Acta Biomed , 2008; 79, pp. 223-226.
- ↑ CJ Wirth: Complications of open joint surgery . Open surgery on the shoulder joint. In: Carl Joachim Wirth u. a. (Ed.): Avoid - recognize - treat complications in orthopedics and trauma surgery . 1st edition. Georg Thieme, Stuttgart 2009, ISBN 978-3-13-148751-3 , p. 332 ff .
- ↑ GG Mollowitz (ed.); G. Mehrtens, M. Reichenbach, D. Höffler: The accident man: Assessments of the consequences of accidents at work, private accidents and occupational diseases. 12th edition. Springer Verlag, 1998, ISBN 3-540-63538-6 , p. 183 ff.
- ↑ Judgment of the Landessozialgericht Bayern L 2 U 390/04 from June 21, 2006 in the process to clarify whether a rotator cuff rupture should be recognized as an occupational disease (BK) according to No. 2101 of the Annex to the Occupational Disease Ordinance (BKV) or as a BKV compensate is