Carpal tunnel syndrome
| Classification according to ICD-10 | |
|---|---|
| G56.0 | Carpal tunnel syndrome |
| ICD-10 online (WHO version 2019) | |
The carpal tunnel syndrome ( CTS , synonyms include: carpal tunnel syndrome , CTS , Medianuskompressionssyndrom , Brachialgia paraesthetica nocturnal ) is a term from the medicine and designates a compression syndrome of the median nerve in the wrist .
anatomy

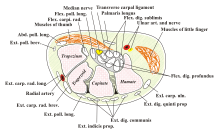
The carpal tunnel is a tunnel-like, tightly enclosed tube from the forearm to the hand on the palmar side (palm side ) of the wrist . The "floor" and the side walls of the tunnel are formed by the carpal bones (part of the bony hand skeleton ), while the "roof" is formed by a broad ligament , the retinaculum flexorum , which spans across the carpal bones. The median nerve runs through the tunnel - together with nine flexor tendons (four each of the superficial and deep finger flexors and four of the long thumb flexor ) , which, among other things, controls the movements of the fingers and the thumb, reports sensations and fulfills vegetative functions in the hand.
Usually at the distal exit of the carpal tunnel, the median nerve gives off a small motor ramus palmaris towards the ball of the thumb . However, there are numerous variants with a more proximal exit, or directly through the retinaculum. The median nerve can also sometimes be divided into two parts or even run through separate retinaculum septa.
causes
Narrowing the carpal tunnel damages the nerve. Carpal tunnel syndrome usually arises when the patient is relatively anatomically tight, when tissue swelling due to mechanical overload, inflammation or general diseases is added.
To carpal tunnel syndrome dispose
- constitutional narrowness of the carpal canal
- Working hand usually more affected (but bilateral occurrence is common)
- manual work
- pregnancy
- Kidney damage
- Wrist or distal forearm fractures and scarring
- Diabetes mellitus
- Tendonitis of the finger flexors
- elongated muscle profile of the long finger flexors
- Underactive thyroid ( hypothyroidism )
- chronic polyarthritis
- Acromegaly
- Infections in the hand area
- increased venous pressure, for example on the shunt arm in dialysis patients
- Alcohol abuse
- Amyloidosis
- Scleroderma
- Fluoroquinolones
Women are about three times more likely to be affected than men.
Carpal tunnel syndrome is practically unknown in children, but with mucopolysaccharidoses of types I, II and VI it often occurs in childhood. Typically, there is no pain, and carpal tunnel syndrome is often associated with a trigger finger .
In rare cases, wrist malformations such as Madelung deformity can trigger a carpal tunnel syndrome in childhood.
Symptoms
Typical initial symptoms are pain or abnormal sensations that can radiate from the hand into the thumb, index finger and middle finger and often occur at night. Later, the symptoms also appear increasingly during the day, in the advanced stage there may be muscle wasting , especially in the area of the ball of the thumb , weakness when grasping and a reduction in the sense of touch ( numbness ). It is not uncommon for vegetative disorders, for example trophic and vascular disorders, to occur.
As the nerve damage progresses, there is an increase in the weakness of typical hand muscles and a decrease in the sense of touch in a localized area of the skin. A disability occurs, in particular, as a result of the reduced function of the thumb. On the other hand, the pain subsides at this stage, as the pain fibers are also destroyed.
If the fine motor skills and sensitivity are reduced, this usually affects the thumb, index finger and middle finger corresponding to the supply area of the median nerve with hyp and paresthesia of the three fingertips and atrophy of the ball of the thumb muscles in an advanced stage.
The carpal canal ( Canalis carpi ) is often sensitive to pressure and light tapping ( Hoffmann-Tinel sign ). If the wrist is overstretched (or flexed strongly), the typical abnormal sensations occur in the sensitive supply area of the median nerve ( Phalen's sign ). The median compression test is positive after about one minute.
Diagnosis
Even if the medical history and physical examination findings are often characteristic of carpal tunnel syndrome, only the measurement of the nerve conduction velocities can confirm the diagnosis. The motor conduction time (“distal motor latency”) of the median nerve between the stimulation site on the wrist and the ball of the thumb muscles innervated by this nerve is measured. Values <4.2 milliseconds are considered normal . The standard values depend on the technique chosen and are not necessarily the same from examiner to examiner. Therefore, both hands should always be measured side by side and the values determined should also be compared with the corresponding values of the ulnar nerve. In the presence of a carpal tunnel syndrome, the sensory conduction velocity of the median nerve between the index finger or middle finger joint and wrist is typically slower than the sensory conduction velocity of the ulnar nerve of the same hand measured for comparison (it is around 48 m / s for both nerves in healthy individuals). Often it turns out that on a symptom-free opposite hand, electrophysiologically abnormal values can already be found (albeit less). An answer to the question of whether it is a (temporary) blockage of the nerve conduction ( neurapraxia ) or even a current destruction of nerve fibers ( axonotmesis ) can only be provided by electromyography .
In the event of a discrepancy between the examination findings and the measured values found, the measurement of the sensible nerve conduction velocity by stimulation on the finger and derivation can take place both in the palm of the hand and beyond the carpal tunnel in order to measure the conduction velocity selectively in the area of the carpal tunnel. The comparison of the responses of the median and ulnar nerves after ring finger stimulation can then be useful for making a diagnosis.
If no comparative measurements are made, the hands should be sufficiently warm when measuring the nerve conduction velocities, as the velocity is about 2 m / s slower per ° C. The ideal measuring temperature is 34 ° C.
Because of the compression by the retinaculum, there is a tightly localized swelling (pseudoneuroma) of the median nerve at the entrance to the carpal tunnel. This can be assessed with an ultrasound examination. The cross-sectional area of the nerves is measured at several points. In most cases, specialized hand surgery centers can make a reliable diagnosis in this way, so that in connection with the corresponding clinical symptoms, the (often painful) measurement of the nerve conduction velocity can be dispensed with. In addition, other pathological changes that are important in this context can be detected during the ultrasound examination, such as tendinitis, excessively long muscle tummies or central arteries.
Damage to the cervical spine , which leads to irritation of the spinal cord or spinal nerve roots ( cervicobrachial syndrome , especially nerve root C6), comes into consideration in the differential diagnosis . With these diseases, too, pain and abnormal sensations can radiate through the arm to the wrist. In addition, the median nerve can be more proximally compressed than pronator teres syndrome. In individual cases, illnesses or a compression syndrome of the arterial vessels can trigger corresponding symptoms. It should therefore not in the investigation to a keyboard of the radial artery pulses and a comparative measurement of blood pressure to dispense on both arms.
Conservative therapy
In the early stages of carpal tunnel syndrome, conservative treatment can be attempted.
At least in the early stages, the symptoms can be improved or eliminated by "shaking out" and rubbing, pumping the fingers, changing position, holding under cold water, etc.
If there is a medical history of severe mechanical, repetitive overload, then doing without the activity that caused the complaint can bring an improvement. Wearing special night splints or putting on shaped support bandages, which are also offered by medical supply stores during the day, can eliminate or alleviate the complaints at least for a while. The night splint prevents the hand from bending at night by immobilizing the wrist.
As supportive or alternative therapy, analgesic and anti-inflammatory drugs can be used, such as non-steroidal anti-inflammatory drugs or a local infiltration of corticosteroids into the carpal tunnel. Cold therapy to reduce inflammatory activity or heat therapy to promote blood circulation are also used.
In the context of pregnancy, symptoms can be expected to subside after the birth.
Operative therapy
A surgical procedure is used in the event of persistent symptoms despite conservative treatment in order to avoid permanent damage. This can usually be done on an outpatient basis.
anesthesia
The procedure is usually carried out under regional anesthesia. Anesthesia of the whole arm is necessary so that the evacuation required for the operation can be better endured. It can be performed as an axillary block or intravenous regional anesthesia. To make the blood empty, the blood is "wrapped" out of the arm with a tight bandage, the backflow of the blood is prevented by a blood seal . In intravenous regional anesthesia, the veins are filled with a local anesthetic to relieve pain in the entire arm. With subaxillary regional anesthesia, the nerves in the armpit that pull the arm are numbed.
Also, a general anesthesia is concerned.
Open surgical technique
The surgeon works from the outside with a direct view of the operating field, sometimes with optical magnification. The skin incision can be curved in the ulnar extension of the middle finger, parallel to or on the thenar fold. The flexion of the wrist should not be exceeded in order to protect the ramus palmaris nervi mediani and the nervus ulnaris. Furthermore, opening the Guyon box on the ulnar side should also be avoided.
An alternative is the “short incision technique” with a skin incision immediately distal to the flexor crease or a “mini incision” further away from the body or a double incision.
The principle of the operation is the complete severing of the retinaculum flexorum , the ligament that spans the carpal bones and delimits the carpal tunnel towards the palm. As a result, the nerve recovers, if the damage caused by the carpal tunnel syndrome has not existed for too long, through the pressure relief achieved. Contrary to previous practice, measures directly on the nerve are only indicated in rare, well-founded exceptional cases. A routine opening of the connective tissue covering around the nerves (epineurotomy) is usually not necessary for initial interventions; surgical splitting of the individual nerve bundles (interfascicular neurolysis) leads to poorer results and is usually not indicated. The illustration of the motor thenar branch, which controls the movement of the ball of the thumb, is usually not necessary, but caution is advised in the case of atypical departure or normal variants. A removal of the mucous membrane ( synovialectomy ) is also usually not necessary, but only in the case of noticeable pathological changes such as increased mucous membrane formation or inflammatory rheumatic inflammation of the mucous membranes ( synovialitis ) and amyloidosis in dialysis patients . The palmaris longus tendon should only be removed with a subsequent autologous transplant. Atypical muscles or tendons within the carpal canal can be removed in individual cases. A reconstruction of the retinaculum (e.g. with a Z- plasty) to improve the coarse strength after surgery has been suggested, but only carried out by individual surgeons in the event of contradicting statements.
The procedure is one of the most common hand surgery operations, takes a few minutes and is very safe. H. afflicted with minimal complication rate. Typical problems are occasional scarring, which require hardening treatment, and a decrease in strength of the rough strength over a few months.
Endoscopic surgical technique
The surgeon works endoscopically , i.e. from the inside, with an instrumental view of the operating field.
Results and Complications
The success of the therapy depends largely on the duration and extent of the previous nerve damage. In uncomplicated cases, splitting the carpal tunnel immediately eliminates all complaints and eliminates pain and nightly abnormal sensations. If there have already been sensory disturbances, abnormal sensations and / or muscle weakness, it cannot be assumed in every case that it will disappear immediately or completely.
The general dangers of surgical interventions (e.g., bleeding , infection , swelling, or damage to nerves and blood vessels ) have become rare. In exceptional cases, irrespective of the surgical technique chosen, lengthy and sometimes very painful bone decalcification and / or soft tissue swelling can result, which can also result in joint stiffening ( Sudeck's disease ).
Comparison of the open and endoscopic technique
In an American review article, data from over 58,000 interventions between 2007 and 2014 were evaluated, and 86% were open to 14% endoscopic interventions. 60% of the patients were women, the largest age cohort was between 65 and 69 years.
Compared to open techniques, the endoscopic procedures have neither clear advantages nor disadvantages. Overall, the results of the operation are comparable to those of the open operation, also when compared to the mini-incision. The higher patient satisfaction with an uncomplicated course and the lower scar pain with endoscopic procedures contrast with a higher complication rate and poorer long-term results than with open surgery. In particular, incomplete splitting of the retinaculum and injury to the motor thenar branch are possible. The endoscopic intervention is associated with a higher cost of materials, higher technical difficulty and longer operation time. The revision rate , i.e. H. the need to operate again is also higher. The operating costs and hospital costs are also higher, but the costs for subsequent physiotherapy are lower.
With open surgery as well as with endoscopic procedures, the retinaculum may be incompletely split or the median nerve and its branches, as well as the ulnar nerve, damaged.
In a follow-up examination after an average of 13 years of 113 patients who had "open" surgery in Massachusetts / USA, 74% were completely symptom-free (80% of them were women and only 59% of men) and 88% were satisfied to very satisfied. Only two operations (1.8%) had to be performed again. All patients without comorbidities were completely symptom-free, while the result was worse the more comorbidities were present. Especially with diabetes, polyneuropathy, rheumatism and osteoarthritis, postoperative function and satisfaction were seldom good to very good.
Aftercare
For the first few days, a cotton bandage or a bandage with slight compression in the wound area without constriction is required. Sometimes the wrist is immobilized briefly using a wrist orthosis or a plaster splint. Pain relieving medication can be used if necessary. Post-operative cold packs can relieve pain. Special "scar ointments" are not required; if necessary, a fatty ointment can be recommended for scar treatment.
An early functional treatment with independent movement exercises of the fingers with little or no strain on the first postoperative day prevents hand edema and finger stiffness and enables the hand to be used earlier in everyday life and at work.
The scar usually heals almost invisibly after 6 months. The duration of the inability to work is a few days to a few weeks, depending on the field of activity.
See also
literature
- S3- guideline carpal tunnel syndrome, diagnosis and therapy of the German Society for Hand Surgery (DGH). In: AWMF online (as of 2012)
- Hans Assmus, G. Antoniadis: Nerve compression syndrome. Steinkopff, Berlin 2008, ISBN 978-3-7985-1818-6 , p. 46f limited preview in the Google book search
- K. Giersiepen, M. Spallek: Carpal tunnel syndrome as an occupational disease. In: Deutsches Ärzteblatt . Volume 108, No. 14, 2011, pp. 238-242. (aerzteblatt.de)
- Riccardo Luchetti, P. Amadio (Ed.): Carpal Tunnel Syndrome. Springer-Verlag, Berlin 2007, ISBN 978-3-540-22387-0 .
Individual evidence
- ↑ Jasmine Z. Cheng, Mohit Sodhi, Mahyar Etminan, Bruce C. Carleton: Fluoroquinolone Use and Risk of Carpal Tunnel Syndrome: A Pharmacoepidemiologic Study . In: Clinical Infectious Diseases . tape 65 , no. 4 , August 15, 2017, ISSN 1058-4838 , p. 684–686 , doi : 10.1093 / cid / cix362 ( oup.com [accessed March 10, 2018]).
- ↑ N. Williams, D. Calloumas, D. Ketteridge, PJ Cundy. DM Eastwood: The mucopolysaccharidoses. In: The Bone & Joint Journal . Volume 99-B, 2017, pp. 1132–1139, doi: 10.1302 / 0301-620X.99B9.BJJ-2017-0487
- ↑ J. Carls, P. Mailänder: Child's bilateral carpal tunnel syndrome with Madelung deformity . In: Springer Verlag (Ed.): Monthly Pediatric Medicine . tape 147 , no. 3 . Springer, March 1999, p. 269-274 .
- ↑ Carpal tunnel syndrome - diagnosis and therapy (long version). (PDF) AWMF, July 2012, accessed on October 14, 2019 . P. 6.
- ↑ Diagnosis and treatment of carpal tunnel syndrome. ( Memento from September 3, 2013 in the Internet Archive ) (PDF) German Society for Hand Surgery
- ↑ A. Żyluk: Carpal tunnel syndrome in pregnancy: a review. In: Pol Orthop Traumatol. Volume 78, Oct 7, 2013, pp. 223-227. PMID 24104526 .
- ↑ S. Ariyan, HK Watson: The palmar approach for the visualization and release of the carpal tunnel. An analysis of 429 cases. In: Plast Reconstr Surg. Volume 60, 1977, pp. 539-547. PMID 909963 .
- ↑ H. Nigst: The carpal tunnel syndrome. Operative technique for surgical decompression. In: Orthop and Traumat. Volume 1, 1992, pp. 122-129.
- ↑ RH Gelberman, ER North: Carpal tunnel release. Open release of transverse carpal ligament. In: RH Gelberman (Ed.): Operative nerve repair and reconstruction. JB Lippincott, Philadelphia 1991, pp. 899-912.
- ^ WB Connolly: Treatment for carpal tunnel syndrome. Wolfe, London 1984.
- ^ JH Huang, EL Zager: Mini-open carpal tunnel decompression. In: Neurosurgery. Vol. 54, No. 2, Feb 2004, pp. 397-399; discussion 399-400. PMID 14744287
- ^ GS Bromley: Minimal-incision open carpal tunnel decompression. In: J Hand Surg Am. Volume 19, No. 1, Jan 1994, pp. 119-120. PMID 8169355 .
- ^ W. Schmidt, AA Gruber, R. Hammer: [Results of different incisions in treatment of carpal tunnel syndrome]. In: hand surgery, microsurgery, plastic surgery. Volume 32, Number 1, January 2000, pp. 67-69, doi: 10.1055 / s-2000-19242 . PMID 10763132 .
- ↑ KM Wilson: Double incision open technique for carpal tunnel release: an alternative to endoscopic release. In: J Hand Surg Am. Volume 19, No. 6, Nov 1994, pp. 907-912. PMID 7876487
- ↑ Borisch and Haussmann 2003.
- ↑ a b Scholten 2004.
- ↑ Chapell et al. a. 2003.
- ↑ Lanz 1977.
- ↑ Shum et al. a. 2002.
- ↑ Karlsson et al. a. 1997.
- ↑ Netscher u. a. 1997.
- ↑ Rosenbaum u. Ochoa 2002.
- ↑ a b Steven Zhang, Molly Vora, Alex HS Harris, Laurence Baker, Catherine Curtin, Robin N. Kamal: cost-minimization analysis of open and endoscopoc carpal tunnel release. In: The Journal of Bone & Joint Surgery . Volume 98-A, Issue 23, December 7, 2016, pp. 1970–1977. doi: 10.2106 / JBJS.16.00121
- ↑ Scholten 2004.
- ↑ Antoniadis et al. a. 1997.
- ↑ Ferdinand u. MacLean 2002.
- ↑ a b Thoma u. a. 2004.
- ↑ Hallock et al. Lutz 1995.
- ↑ Wong et al. a. 2003.
- ↑ Trumble et al. a. 2001.
- ↑ Brown et al. a. 1993.
- ↑ unicorn u. Leddy 1996.
- ↑ Shinya et al. a. 1995.
- ^ Concannon et al. a. 2000.
- ↑ MacDermid et al. a. 2003.
- ↑ Hunt et al. Osterman 1994.
- ↑ Assmus u. a. 2006.
- ↑ Dexter L. Louie, Brandon E. Earp, Jamie E. Collins, Elena Losina, Jeffrey N. Katz, Eric M. Black, Barry P. Simmons, Philip E. Blazar: Outcomes of open carpal tunnel release at a minimum of ten years. In: The Journal of Bone & Joint Surgery . Volume 95-Am, Issue 12, June 19, 2013, pp. 1067-1073. doi: 10.2106 / JBJS.L.00903 .
- ↑ Cook et al. a. 1995.