Intrauterine device
Intrauterine devices ( Latin intra , inside; uterus , uterus), also known colloquially as coils , are medical devices for contraception for women that are inserted into the uterus . Today there are two different types that differ according to the principle of action: The copper or copper-gold coil discussed here and the hormone coil , which is also known as the intrauterine system (IUS). In the past, rings made of wound metal wire ( e.g. Graefenberg ring ) and models made solely of plastic (e.g. Lippes -Loop) were used.
history
The use of intrauterine devices is the most widespread method of reversible contraception around the world today. At the beginning of the 20th century, the first products made of silk or silver wire were designed. a. by the German gynecologist Ernst Graefenberg and the Japanese Tenrei Ota . With the development of thermoplastic materials in the late 1950s, numerous shapes and models came onto the market. The Lippes Loop and the Margulies Spiral, for example , after which the intrauterine devices are now colloquially named, date from this time . In the 1970s, the Dalkon Shield developed severe inflammation due to specific design deficiencies, which, however, earned all intrauterine devices the reputation of being at high risk. Intrauterine devices have contained copper since the 1970s , after the contraceptive effect of copper became known. There are no longer any intrauterine devices in Germany that are made exclusively of plastic; the last one (Goldlily sensitive) was taken off the market because the Pearl Index is far above that of the copper-containing intrauterine devices.
construction
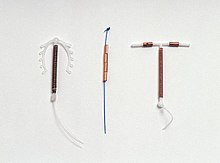
The copper spiral consists of a plastic structure of 2.5 to 3.5 centimeters in size wrapped with fine copper wire or a copper-gold alloy . There are also copper spirals with small gold clips, which however have no effect of their own (e.g. Femena Gold). However, the gold clips are intended to improve the visibility of the coil in the ultrasound. Another variant of the so-called gold spiral is offered by a gold core inside the copper wire (e.g. with the Gold-T or Goldlily). The precious metal gold inside the copper wire helps the copper to break down less easily and thus ensures a longer shelf life. Gold is very resistant to corrosion and inert and can therefore be classified as hypoallergenic. Many of the copper spirals used today are shaped like a T. But other variants, such as loops or the shape of the number 7, are also possible. The purpose of these different shapes is to ensure that the spiral is held as securely as possible in the uterine cavity and yet can be removed easily. The copper chain is anchored in the uterine muscles so that an additional frame is not required for fixation ( frameless IUD ). At the lower end of the intrauterine device there is an eyelet to which retrieval threads are attached that protrude about 1 to 2 cm from the cervix . So-called inert intrauterine devices, which have neither a copper component nor a hormone reservoir, are currently not sold in Germany.
effect
The working principle has not been clarified in every detail. Several different mechanisms are discussed:
- Copper ions have a toxic and inhibitory effect on sperm , which leads to a reduction in mobility and lifespan. The effect of copper is locally limited to the uterus, fallopian tubes and cervix. Elevated serum concentrations of copper ions are not found.
- In addition, the spiral caused as a foreign body, a sterile inflammatory response of the endometrium so that their changing nature and produced by their cytotoxic enzymes a nidation prevent (implantation), and therefore it is sometimes referred to as "Notfallkontrazeptivum" used.
- Inflammatory cells , such as macrophages , can also break down sperm directly ( phagocytosis )
- An influencing of the fallopian tube function leads to an impairment of the egg and sperm transport.
- The use of a gold-copper alloy in the so-called gold spirals or copper-gold spirals is intended to reduce the risk of infections and inflammation through a bacteria and fungus-inhibiting effect by means of the gold and copper ions dissolved in traces.
- A microgalvanic effect in the gold-copper alloys is also intended to reduce the orientation and mobility of the sperm, so that the principle of action is not the inhibition of nidation, but the prevention of egg fertilization.
The copper IUD is a very effective means of contraception. In particular, the fact that no interaction is required on the part of the woman or her partner avoids application errors, which are the main cause of failure of most contraceptives.
According to Pro Familia, the pearl index of the copper spiral is around 0.3 to 0.8, that of a gold-copper spiral ( gold lily or gold-T ) around 0.5–1.0. The variant of the copper chain , whose operating principles correspond to those of the copper spiral, has - depending on the study - the same or an even better Pearl index of 0.1-0.3.
application
The insertion of the IUD is performed by a gynecologist and is usually done during menstruation , as the cervix is naturally somewhat open at this time. A stretching of the cervical canal, for example with Hegar pins , is rarely necessary. The correct fit of the spiral is then checked using ultrasound .
The IUD can also be used immediately after an abortion or a miscarriage .
Young women who have not yet given birth can also use the IUD. However, ejection rates of up to 10% are described here. Since the uterus is usually smaller in these women, correspondingly smaller IUD models can then be used.
Spiral afterwards
A deposit no later than five days after unprotected intercourse than spiral afterwards is possible and especially worth considering if the 72-hour time period for the morning-after pill has been exceeded, the unprotected sexual intercourse has taken place at the time of ovulation or for medical reasons no hormonal Nachverhütung is possible. All copper-containing IUDs (copper spiral, copper chain ) approved for this purpose can then be used as a spiral . In the case of emergency contraception, the IUD can then prevent unwanted pregnancy up to five days after unprotected sexual intercourse with up to 99% certainty. The professional association of gynecologists recommends it as the safest emergency contraceptive method, since compared to the two preparations of the morning-after pill, the effectiveness of the copper IUD does not decrease with every past hour and it still works retrospectively if the unprotected sexual intercourse took place at the time of ovulation Has. Likewise, the user's BMI and user safety play no role in the preventive effect.
Duration of the spirals
The length of time the IUDs remain in place is based on the information provided by the manufacturer of the respective intrauterine device, although most copper IUDs are recommended to be used for a maximum of three or five years. However, these can also be removed before the end of the lay period. Removal can cause slight pain, but it usually subsides immediately after the procedure. After removing an intrauterine device, a new specimen can be inserted directly. After removing the copper coil, the woman is usually fertile again in the next cycle.
Risks
- Women who wear an IUD have an 8-fold higher risk of infection in the first month than women without an IUD. In the first four months after the deposit, the risk is increased by a factor of 4. Thereafter, there is no increased risk of infection for a period of up to eight years. In the event of an infection, the IUD should always be removed. In this case, however, an infection is not caused by the coil itself, but by an existing infection of the vagina, usually with Chlamydia trachomatis . This infection occurs more frequently in young women between the ages of 15 and 19 and should be ruled out before inserting an IUD in order to prevent an ascending infection.
- According to a large study, the risk of cervical cancer is not increased, but decreased.
- The increase in the likelihood of ectopic pregnancies known from outdated copper-free IUDs is significantly lower with the copper IUD, as the principle of action also prevents extrauterine pregnancies relatively safely.
- Bleeding disorders, usually in the form of increased menstruation, and increased menstrual cramps are common side effects. This occurs just as often with frameless IUDs as with conventional IUDs .
- In the first two to three months, the risk of ejection of the intrauterine device is increased.
- In rare cases, the uterine wall can be pierced when the coil is inserted. The risk is increased with an insert shortly after giving birth.
- The retrieval sutures can turn up into the uterus, so that removal usually requires a surgical procedure ( hysteroscopy ).
Contraindications
Under no circumstances should a coil be inserted if:
- a pregnancy is suspected or on a pregnancy
- Undiagnosed bleeding disorders are present
- There is inflammation in the genital area
- there is a suspicion of a malignant disease of the uterus .
In case of:
- Diabetes mellitus
- Kidney disease
- Treatments with immunosuppressants
- Treatment with anticoagulants
- Uterus myomatosus
A IUD should only be inserted in individual cases after weighing up all the risks.
Costs and assumption of costs
The copper coil usually costs 120 to 200 euros for an application period of three to five years. A hormone-containing IUD approx. 300 to 400 euros, for a period of use of up to five years. This price includes advice, examination and lodging. The costs for women with statutory health insurance in Germany according to Section 24a of the Social Code Book V up to the age of 20 are covered by the health insurance company, and for women entitled to social assistance who are not insured ( Section 52 ), according to Section 49 of the SGB XII (help for family planning) by the responsible social assistance provider accepted.
distribution
In Germany, according to the Federal Center for Health Education, 10% of women use IUDs, in Switzerland 6%, in Austria 12% and in China 46% (as of 2004).
Ethical issues
In some cultures it is not possible for women to decide independently about contraception. If the retrieval threads are shortened accordingly, wearing a spiral is not obvious, which is why “contraceptive anonymity” is guaranteed.
Some population groups reject the use of intrauterine devices because of their anti-nidation effect for ideological reasons.
see main article Life Rights Movement .
See also
Web links
- ProFamilia
- The hormone spiral on Familienplanung.de - Information portal of the Federal Center for Health Education (BZgA)
- Museum for Contraception and Abortion Vienna
Individual evidence
- ↑ C. d'Arcangues: Worldwide use of intrauterine devices for contraception. In: Contraception , Volume 75, 2007, pp. S2-S7.
- ↑ The development of the intrauterine device . Der Standard , December 14, 2006; Retrieved April 21, 2015.
- ^ M. Thiery: Pioneers of the intrauterine device. In: European Journal of Contraception and Reproductive Health Care Volume 2, 1997, pp. 15-23.
- ↑ D. Cheng: The Intrauterine Device: Still misunderstood after all these years. In: Southern Medical Journal , Vol. 93, No. 9, 2000, pp. 859-864.
- ^ E. Espey, T. Ogburn: Perpetuating negative attitudes about the intrauterine device: textbooks lag behind the evidence. In: Contraception , Volume 65, 2002, pp. 389-395.
- ↑ Zipper u. a .: Metallic Copper as an intrauterine contraceptive adjunction to the "T" device. In: American Journal of Obstetrics and Gynecology , Volume 109, 1969, pp. 1274-1278.
- ↑ a b c d A Feige, A Rempen, W Würfel, J Jawny, A. Rohde: Frauenheilkunde . in the Google book search, Elsevier, Urban & Fischer Verlag, 2006, ISBN 3-437-21871-9 , chap. 5: Contraception - Intrauterine Device , pp. 257-259
- ^ JW Dudenhausen: gynecology and obstetrics . Walter de Gruyter, 2001, ISBN 3-11-016562-7 ( limited preview in the Google book search).
- ^ KJ Bühling, W. Friedmann: Intensive course in gynecology and obstetrics . in the Google book search Elsevier, Urban and Fischer Verlag, 2004, ISBN 3-437-42400-9 , 2.2 Pregnancy contraception , p. 85.
- ↑ a b c d I. Gerhard: Obstetrics integrative . in Google Book Search. Elsevier, Urban and Fischer Verlag, 2005, ISBN 3-437-56510-9 , chap. 18.1.2 Intrauterine Device (IUD) , pp. 349-350.
- ↑ a b Pro Familia : The Spiral - page 9 (PDF; 100 kB)
- ↑ bvf.de (PDF)
- ↑ Thomas Rabe, Christian Albring: Emergency Contraception - an Update Joint statement of the German Society for Gynecological Endocrinology and Reproductive Medicine (DGGEF) e. V. and the professional association of gynecologists (BVF) e. V. Ed .: Seminar in Gynecological Endocrinology. 2013, ISBN 978-3-00-039077-7 , pp. 368-394 .
- ↑ Amna I. Dermish, David K. Turok: The copper intrauterine device for emergency contraception: an opportunity to provide the optimal emergency contraception method and transition to highly effective contraception . In: Expert Review of Medical Devices . tape 10 , no. 4 , July 1, 2013, ISSN 1743-4440 , p. 477-488 , doi : 10.1586 / 17434440.2013.811865 .
- ↑ Werner Mendling: Chlamydia smear before spiral insert . No. 21 . gyn, S. 466-467 .
- ↑ Xavier Castellsagué, Mireia Díaz, Salvatore Vaccarella, Silvia de Sanjosé, Nubia Muñoz, Rolando Herrero, Silvia Franceschi, Chris JLM Meijer, F Xavier Bosch: Intrauterine device use, cervical infection with human papillomavirus, and risk of cervical cancer: a pooled analysis of 26 epidemiological studies. The Lancet Oncology 12 (2011), pp. 1023-1031, doi: 10.1016 / S1470-2045 (11) 70223-6
- ^ P O'Brien, CC. Marfleet: Frameless versus classical intrauterine device for contraception. Cochrane Database of Systematic Reviews 2005, Issue 1. Art. No .: CD003282 doi: 10.1002 / 14651858.CD003282.pub2
- ↑ R. Gros: Gynecology for women. Thieme Verlag, Stuttgart, 1989. Page 67.
- ↑ The copper spiral . Pro Familia .
- ↑ Youth sexuality - results of the current representative survey 2010 . Federal Center for Health Education , Cologne 2010, ISBN 978-3-937707-79-2 , p. 160 ff. Forschung.sexualaufklaerung.de ( Memento of the original from February 9, 2015 in the Internet Archive ; PDF) Info: The archive link was automatically used and not yet tested. Please check the original and archive link according to the instructions and then remove this notice. .
- ↑ Contraception methods 1996. ( Memento of the original from June 26, 2008 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice. Swiss Federal Statistical Office.
- ↑ Contraception with the IUD . Der Standard , April 21, 2015
- ^ Chinese women and their contraceptive choices . China Daily , Jan. 8, 2005; Retrieved April 21, 2015.