Hippel-Lindau disease
| Classification according to ICD-10 | |
|---|---|
| Q85.8 | Other phacomatoses |
| ICD-10 online (WHO version 2019) | |
The von Hippel-Lindau syndrome ( VHL syndrome ), sometimes also referred to as retino-cerebellar angiomatosis , is a rare, hereditary tumor disease from the so-called phakomatoses . The patients develop benign, tumor-like tissue changes ( angiomas ) primarily in the area of the retina of the eye and the cerebellum . The latter was also known as Lindau tumor or Lindau syndrome . In the central nervous system , the brain stem and spinal cord , and rarely the cerebrum, can also be affected. It is characteristic of VHL syndrome that preforms of the connective tissue develop into tumors consisting of blood vessels. Many patients also have tissue changes in the kidney (renal cell carcinoma), adrenal gland ( pheochromocytoma ), and pancreas. In men, the epididymis can be affected. These tissue changes can be harmless, but they can also develop into malignant tumors. The cause of the disease is a gene mutation in the Von Hippel Lindau tumor suppressor gene. Since VHL syndrome is a genetic disorder, no cure is possible. The treatment of the patient depends on the location and the severity of the tissue changes. The retinal tumors on the eye are destroyed using laser beams. Malignant growths occur primarily in the kidney area and are treated according to the guidelines for treating this disease. The tissue changes in the central nervous system are operated on if their location and size can cause dangerous consequences for the patient. Since the disease can be detected early, regular check-ups are recommended.
history
The disease is named after the Göttingen ophthalmologist Eugen von Hippel (1867–1939) and the Swedish pathologist Arvid Lindau (1892–1958). Von Hippel first described angiomas of the eye in 1904 , Lindau in 1926 the angiomas in the spinal cord.
Incidence, inheritance, epidemiology
A family connection of the disease was initially suspected when examining siblings in 1894. 1929 has been found that the VHL syndrome of autosomal - dominant obey inheritance. The risk of developing tumors increases with age. The maximum genetic penetrance is reached at the age of 65. The incidence is given between 1: 36,000 - 1: 45,000. The possible manifestations of the disease can vary greatly in sick people. Depending on the study, the spontaneous mutation rate is up to 50%. Men and women are equally affected.
Pathogenesis, molecular biology and pathophysiological relationships
The gene for Hippel-Lindau disease was localized in the region of chromosome 3, band p25 / 26. It is involved in the cell cycle and the formation of new blood vessels. The HL gene has three exons and codes for a nuclear protein that binds to proteins of the elongin group. A large number of mutations have been discovered in patients with HL disease, all of which are largely evenly distributed across the gene. Various studies have found that 35% of mutations are missense mutations and around 75% of patients have a germline mutation.
pathology
The angiomas of HL syndrome are predominantly capillary hemangiomas and hemangioblastomas . A hemangioma is the term used to describe benign, tumor-like neoplasms with a conformation of blood vessels. They usually appear as hamartomas , so they are not tumors in the strict sense. The hemangiomas do not arise, as the name suggests, from blood vessels, but from connective tissue precursors and they develop into structures that can most simply be referred to as blood vessel clusters or blood sponges. The blood sponges found in the cerebellum, brain stem, and spinal cord of VHL patients are hemangioblastomas. This term is used to describe real neoplasms that consist of overgrown capillary shoots.
- The retinal hemangiomas can be more angiomatous or more fibrosing. This is very important for the prognosis of the disease in relation to the eye. With more angiomatous hemangiomas, the vascular portion of the tissue change predominates, which can often lead to massive bleeding into the eye with sudden complete blindness. Fibrosing hemangiomas tend to change the traction of the retina. If the hemangiomas are on the periphery of the retina, they often do not cause any discomfort. If, on the other hand, they are central, visual acuity may soon be reduced. If the blood vessels form short circuits between veins and arteries, tissue fluid can leak into the eye with corresponding consequences (pressure increase).
- Hemangioblastomas manifest themselves primarily in the cerebellum and become symptomatic when the growth rate is slow due to disruption of the CSF outflow. Since they also produce erythropoietin , polycythemia is observed in some cases . Under the microscope, the capillary hemangioblastoma appears as an extremely well vascularized tumor with CD31 / CD34-positive vascular endothelium and NSE expression of the stroma.
Clinical picture
The core, or cardinal, symptoms of VHL syndrome are the appearance of retinal hemangiomas and cerebellar hemangioblastomas.
The clinical spectrum of the disease includes affections of the eyes and the cerebellum and the occurrence of hemangioblastomas in the area of the brain stem and the spinal cord . Renal cell carcinomas (the risk of disease is 25-45%, mostly from the age of 50), pancreatic cysts, pheochromocytomas, epididymal cysts and polycythemia are then observed.
The hemangioblastomas of the CNS present in about 60% of the cases in the cerebellum, in 13% of the cases in the spinal cord and in 4% of the cases in the brain stem . Rarely <1% in the cerebrum. The lesions in the cerebellum become clinically evident on average in patients aged 29 years and in the case of spinal cord lesions at 34 years of age.
The diagnostic criterion is the detection of bilateral or multiple retinal hemangiomas or the detection of multiple hemangioblastomas of the posterior fossa.
On the basis of clinical courses and differences in the phenotype - genotype correlation, a distinction is made between two forms of VHL syndrome. Patients without pheochromocytoma are assigned to VHL type I, patients with a pheochromocytoma to VHL type II.
Very different statements are made about the course of the disease. The retinal angiomas are revealed on average in the patients by the age of 25. The retinal changes can be treated well if they are discovered in good time. The intracerebral and spinal hemangioblastomas can lead to dangerous bleeding, especially in the area of the brain stem.
Genotype-Phenotype Correlation
In HL type I, microdeletions and nonsense mutations were discovered in over 50% of the cases examined . In HL type II, missense mutations were found in almost 100% of the patients examined .
diagnosis
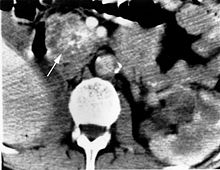
The diagnosis of VHL syndrome is made in the presence of capillary hemangioblastomas (vascular tumors) in the CNS or the retina of the eye. Other tumors belonging to the VHL complex ( pheochromocytoma , renal cell carcinoma ) or a corresponding family history appear. In magnetic resonance imaging , the hemangioblastomas appear as contrast-enhancing nodules.
therapy
The choice of therapy depends on the size, location and clinical picture. Only early diagnosis and effective therapy can maintain visual acuity . In a few rare individual cases, spontaneous regressions without treatment for retinal angiomas have been described.
Laser coagulation
The laser photocoagulation is used currently for smaller retinal hemangioma. Argon, krypton, dye and diode lasers, previously also xenon coagulators, are used. The advantage of the procedure is the targeted destruction with precise dosage, whereby the healthy tissue is spared. Frequent use of the method shows success in retinal hemangiomas up to a size of 4.5 mm, but the therapy is most effective with sizes up to 1.5 mm (corresponds to a papilla diameter) or smaller. Angiomas that are larger than the diameter of a papilla show only unsatisfactory results with laser coagulation and should therefore be treated with other methods. Laser coagulation can take place directly on the angioma, on the vessels supplying the angioma, or both at the same time. The response rate for direct photocoagulation when using the argon laser is 91 - 100%. Hemangiomas the size of the diameter of a papilla need an average of three applications to complete obliteration, whereas one session is usually sufficient for microangiomas. Some authors recommend combining laser coagulation with other methods to treat angiomas that could not be adequately treated by laser coagulation alone.
The use of the yellow laser with the krypton laser offers a theoretical advantage over the other laser methods, since the oxidized and reduced hemoglobin absorbs more yellow wavelengths than green or blue as with the argon laser. As a result, the supplying vessels should be irradiated more intensely.
The most common side effects of laser coagulation are vitreous hemorrhages or exudative retinal detachments , especially due to lipid deposits in the macula with permanent visual loss. This degenerative process can occur within a day of treatment. The complications are particularly common when the angioma has already caused structural changes. With indirect laser coagulation, a few months after the treatment, reperfusion of the vessels supplying the angioma can occur. Which may make follow-up treatments necessary. The occlusion of a supplying artery can lead to an infarction in the retina it supplies. The consequence is visual field losses.
Despite treatment with direct or indirect laser coagulation, new hemangiomas can develop later. Recurrences of the treated angioma can also occur. In histological examinations, treatment with laser beams showed only superficial destruction of tumor cells in large hemangiomas. In the depth, unchanged tumor tissue could be found. In contrast, complete destruction could be demonstrated in small hemangiomas.
Cryotherapy
In the cryotherapy be angiomas, which are greater than two disc diameter and far peripherally treated. Angiomas with subretinal exudates can also be treated in this way. This method was first used and studied by Lincoff in 1967. The retinal angioma is frozen at temperatures of −60 ° C to −80 ° C. In a long-term study, the best results were seen with angiomas smaller than 3.75 mm. For larger angiomas, cryotherapy was not more successful than laser coagulation, but it showed fewer complications than treatment with laser beams.
Follow-up treatments are also often necessary for cryotherapy, but there should be a minimum interval of two months between treatments. Exudative retinal detachments and proliferative vitreoretinopathy can occur as complications .
Brachytherapy
For angiomas of a size of 4 mm, ruthenium-106 applicators can be used as episcally sewn steel supports. After the irradiation, the angiomas regress more slowly than treatment with laser beams. The average regression time is 5 to 14 months. After irradiation, chorioretinal scars that were larger than the tumor almost always develop. The greatest danger is injury to the optic nerve from radioactive rays.
With brachytherapy , too , exudative retinal detachment and vitreous hemorrhage can occur, but these occurred less often than with conventional treatment methods. Epiretinal membrane formations, which require surgical repair, can rarely occur. However, if the retinal detachment existed before the treatment, the risk of complications after brachytherapy is greatly increased.
Transpupillary thermotherapy
The Transpupillary thermotherapy can in the treatment of choroidal melanoma, retinoblastoma and choroidal hemangiomas are attempted. Local heating of the tumor is generated by means of an infrared diode laser. Histological examinations showed clear necrosis of the tumor in choroidal melanoma after treatment. In the treatment of retinal hemangiomas, on the one hand, there were successes, on the other hand, other studies showed little effectiveness of the method.
Photodynamic Therapy
For larger angiomas, the effectiveness of photodynamic therapy with verteporfin is currently being investigated in clinical studies. Improvements in vision by an average of 0.5 after two years were found. Macular edema can occur as a side effect , which in turn can lead to a deterioration in vision . This method can also be combined with photocoagulation.
radiotherapy
Radiation treatment was attempted as the very first therapeutic method for retinal angiomas by Houwer in 1919. However, he could not determine any effectiveness, which has been confirmed by other authors. The therapy showed success in individual cases at a dose of 12 Gray. In a long-term study of 11 years, radiation therapy was only successful in one case at an average dose of 38 Gray. A more recent study from 2004 showed an improvement in visual acuity from 0.28 to 0.44, with an average tumor reduction of around 40%, although not all tumors were reduced in size to the same extent. The greatest reduction was seen in smaller angiomas. The patients were fractionally irradiated with a total dose of 21.6 Gray over twelve days. One patient developed cataract as a side effect.
Proton therapy
This therapeutic method has the advantage of a high level of precision in tissue destruction, whereby non-diseased tissue parts are spared. Therefore, this method is used when angiomas grow near sensitive areas of tissue. Here, protons applied, which can penetrate several centimeters into the tissue with great energy.
Medication
The treatment of angiomas with VEGF inhibitors such as pegaptanib or SU 5416 has been investigated in clinical studies . No changes in tumor size were found. However, visual improvements occurred due to the reduction in macular edema. Anaphylaxis can occur as a serious side effect . At the moment, drug therapy is being discussed as an adjunct therapy alongside conventional therapy methods.
Enucleation
The indication for enucleation is rarely made. Mostly when there is pain in the blind eye, caused by secondary glaucoma.
Others
Therapy is the surgical removal of the tumors.
Individual evidence
- ^ J. van der Hoeve: The Doyne Memorial Lecturs: Eye symptoms in phakomatoses. In: Tr Ophth Soc UK. 1932. 52, p. 380.
- ^ ET Collins: Two cases, brother and sister, with peculiar vascular new growth, probably primarily retinal, affecting both eyes. In: Trans Opthalmol Soc. UK 1894, 14, pp. 141-149.
- ↑ HU Moller: Familial angiomatosis retinae et cerebelli. In: Acta Ophthalmol. 1929, 7, pp. 244-260.
- ↑ PL Choyke, GM Glenn, MM Walther et al .: von Hippel-Lindau disease: genetic, clinical, and imaging features. In: Radiology. 1995, 194, pp. 629-642.
- ↑ ER Maher, L. Iselius, JR Yates et al.: Von Hippel-Lindau disease: a genetic study. In: J Med Genet . 1991 28, pp. 443-447.
- ^ HP Neumann, OD Wiestler: Clustering of features of von Hippel – Lindau syndrome: evidence for a complex genetic locus. In: The Lancet . 1991, 337, pp. 1052-1054.
- ^ A b M. Ridley, J. Green and G. Johnson: Retinal angiomatosis: the ocular manifestations of von Hippel-Lindau disease. In: Can J Ophthalmol. 1986. 21 (7), pp. 276-283.
- ^ JT Whitson, RB Welch, WR Green: Von Hippel-Lindau disease: case report of a patient with spontaneous regression of a retinal angioma. In: Retina. 1986. 6 (4), pp. 253-259.
- ^ D. Schmidt, HPH Neumann: Atypical retinal changes in v. Hippel-Lindau syndrome. In: Fortschr Ophthalmol. 1987, 84 (2), pp. 187-189.
- ↑ M. Bonnet, G. Garmier, S. Tlouzeau, C. Burtin: [Treatment of retinal capillary angiomas of von Hippels disease]. In: J Fr Ophtalmol. 1984, 7, pp. 545-555.
- ^ A b M. F. Goldberg, S. Koenig: Argon laser treatment of von Hippel – Lindau retinal angiomas. I. Clinical and angiographic findings. In: Arch Ophthalmol. 1974 92, pp. 121-125.
- ↑ I. Kremer, E. Gilad, I. Ben-Sira: Juxtapapillary exophytic retinal capillary hemangioma treated by yellow krypton (568 nm) laser photocoagulation. In: Ophthalmic Surg. 1988, 19, pp. 743-747.
- ↑ a b G. Meyer-Schwickerath: Light coagulation in angiomatosis retinae. In: Lichtkoagulation, ophthalmologist's library. 1959; 33, pp. 62-70.
- ↑ a b J. DM Gass: Treatment of retinal vascular anomalies. In: Trans Am Acad Ophthalmol Otolaryngol. 1977, 83, pp. 432-442.
- ^ A b C. M. Lane, G. Turner, ZJ Gregor, AC Bird: Laser treatment of retinal angiomatosis. In: Eye. 1989 3, pp. 33-38.
- ↑ RH Rosa Jr, MF Goldberg, WR Green: Clinicopathologic correlation of argon laser photocoagulation of retinal angiomas in a patient with von Hippel – Lindau disease followed for more than 20 years. In: Retina. 1996, 16, pp. 145-156.
- ↑ a b c d D. Schmidt, E. Natt, HPH Neumann: Long-term results of laser treatment for retinal angiomatosis in von Hippel-Lindau disease. In: Eur J Med Res. 2000; 5, pp. 47-58.
- ↑ CF Blodi, SR Russell, JS Pulido, JC Folk: Direct and feeder vessel photocoagulation of retinal angiomas with dye yellow laser. In: Ophthalmology. 1990, 97, pp. 791-795; discussion 796-797.
- ^ A b W. J. Annesley, BC Leonard, JA Shields, WS Tasman: Fifteen year review of treated cases of retinal angiomatosis. In: Trans Am Acad Ophthalmol Otolaryngol. 1977, 83, pp. 446-453.
- ↑ A. Lommatzsch, A. Wessing: Angiomatosis retinae. Long-term observations. In: Ophthalmologist. 1996; 93, pp. 158-162.
- ↑ GA Peyman, M. Raichand, RC Zeimer: Ocular effects of various laser Wavelengths. In: Surv Ophthalmol. 1984, 28, pp. 391-404.
- ^ RB Welch: von Hippel-Lindau disease: the recognition and treatment of early angiomatosis retinae and the use of cryosurgery as an adjunct to therapy. In: Trans Am Ophthalmol Soc. 1970, 68, pp. 367-424.
- ^ A. Wessing: 10 years of light coagulation in angiomatosis retinae. In: Klin Monatsbl Augenheilk. 1967. 150, pp. 57-71.
- ^ A b D. J. Apple, MF Goldberg, GJ Wyhinny: Argon laser treatment of von Hippel-Lindau retinal angiomas. II. Histopathology of treated lesions. In: Arch Ophthalmol. 1974. 92 (2), pp. 126-130.
- ^ I. Baras, S. Harris, MA Galin: Photocoagulation treatment of angiomatosis retinae. In: Am J Ophthalmol. 1964; 58, pp. 296-299.
- ^ MF Goldberg, JR Duke: Von Hippel-Lindau disease. Histopathological findings in a treated and an untreated eye. In: Am J Ophthalmol. 1968; 66, pp. 693-705.
- ↑ MB Gorin: von Hippel-Lindau disease: clinical considerations and the use of fluorescein-potentiated argon laser therapy for treatment of retinal angiomas. In: Semin Ophthalmol. 1992, 7, pp. 182-191.
- ↑ H. Lincoff, J. McLean, R. Long: The cryosurgical treatment of intraocular tumors. Am J Ophthalmol 1967; 63, pp. 389-399.
- ↑ RC Watzke: Cryotherapy for retinal angiomatosis. A clinicopathologic report. In: Arch Ophthalmol. 1974; 92, pp. 399-401.
- ^ JA Shields: Response of retinal capillary hemangioma to cryotherapy. In: Arch Ophthalmol. 1993; 111, p. 551.
- ↑ a b N. Bornfeld, KM Kreusel. Capillary hemangiomas of the retina in Von Hippel Lindau syndrome. In: Ophthalmologist. 2007; 104, pp. 114-118.
- ↑ KM Kreusel, N. Bornfeld, A. Lommatzsch et al. Ruthenium-106 brachytherapy for peripheral retinal capillary hemangioma. In: Ophthalmology. 1998; 105, pp. 1386-1392.
- ↑ K. Rohrschneider, ROW Burk, N. Bornfeld et al . Capillary hemangioma of the retina. Laser scanning tomographic follow-up observations after radiation therapy. In: Fortschr Ophthalmol. 1991; 88, pp. 623-628.
- ↑ JA Oosterhuis, HG Journee-de Korver, HM Kakebeeke-Kemme, JC Bleeker: Transpupillary thermotherapy in choroidal melanomas. In: Arch Ophthalmol. 1995; 113, pp. 315-321.
- ^ CL Shields, MC Santos, W. Diniz et al: Thermotherapy for retinoblastoma. In: Arch Ophthalmol. 1999; 117, pp. 885-893.
- ↑ IS Othmane, CL Shields, JA Shields et al .: Circumscribed choroidal hemangioma managed by transpupillary thermotherapy. In: Arch Ophthalmol. 1999, 117, pp. 136-137.
- ↑ CL Shields, JA Shields, J. Cater et al .: Transpupillary thermotherapy for choroidal melanoma: tumor control and visual results in 100 consecutive cases. In: Ophthalmology. 1998, 105, pp. 581-590.
- ↑ JG Journeé-De-Korver, JA Oosterhuis, HM Kakebeeke-Kemme and others: Thranspupillary thermotherapy (TTT) by infrared irradiation of choroidal melanoma. In: Doc Ophthalmol. 1992; 82, pp. 185-191.
- ↑ DN Parmar, K. Mireskandari, D. McHugh: Transpupillary thermotherapy for retinal capillary hemangioma in von Hippel-Lindau disease. In: Ophthalm Surg Lasers. 2000; 31, pp. 334-336.
- ↑ J. Garcia-Arum, LH Sararols, L. Cavero et al .: Therapeutic options for capillary papillary hemangiomas. In: Ophthalmology. 2000; 107, pp. 48-54.
- ^ H. Rodriguez-Coleman, RF Spaide, LA Yannuzzi: Treatment of angiomatous lesions of the retina with photodynamic therapy. In: Retina. 2002; 22, pp. 228-232.
- ↑ TM Aaberg, TM Aaberg, DF Martin et al .: Three cases of large retinal capillary henangiomas treated with verteporfin and photodynamic therapy. In: Arch Ophthalmol. 2005; 123, pp. 328-332.
- ↑ A. Szabo, Z. Géhl, A. Seres: Photodynamic (verteporfin) therapy for retinal capillary haemangioma, with monitoring of feeder and draining blood vessel diameters. In: Acta Ophthalmol Scand. 2005; 83, pp. 512-513.
- ^ SJ Bakri, JE Sears, AD Singh. Transient closure of a retinal capillary hemangioma with verteporfin photodynamic therapy. In: Retina. 2005; 25, pp. 1103-1104.
- ↑ AWM Houwer: von Hippels disease: retinal angiomatosis. In: Am J Ophthalmol 1919; 2, p. 820.
- ^ AJ Ballantyne: Angiomatosis retinae. Account of a case including histologic results. In: Proc R Soc Med 1941; 35, pp. 345-358.
- ↑ C. Cordes, MJ Hogan: Angiomatosis retinae (Hippels disease): report of a case in which roentgen therapy was used in an early stage. In: Arch Ophthalmol 1940; 23, pp. 253-269.
- ^ FH McGovern: Angiomatosis retinae. In: Am J Ophthalmol 1943; 26, pp. 184-187.
- ↑ Cordes FC, Dickson OC: Angiomatosis retinae (von Hippels disease). Results following irradiation of three eyes. In: Am J Ophthalmol. 1943; 26, pp. 454-463.
- ^ FC Cordes, A. Schwartz: Angiomatosis retinae (von Hippels disease) eleven years after irradiation. In: Trans Am Ophthalmol Soc. 1943; 50, pp. 227-235.
- ^ D. Raja, MS Benz, Murray TG et al. Salvage external beam radiotherapy of retinal capillary hemangiomas secondary to von Hippel-Lindau disease. In: Ophthalmology. 2004; 111, pp. 150-153.
- ↑ JD Palmer, ES Gragoudas: Advances in treatment of retinal angiomas. In: Int Ophthalmol Clin. 1997; 37, pp. 150-170.
- ↑ N. Bornfeld, P. Chauvel, MH Foerster et al. Proton therapy of intraocular tumors. In: Klin Mbl Augenheilk. 1994; 204, p. 195.
- ↑ SS Dahr, M. Cusick, H. Rodriguez-Coleman et al. Intravitreal anti-vascular endothelial growth factor therapy with pegaptanib for advanced von Hippel-Lindau disease of the retina. In: Retina. 2007; 27, pp. 150-158.
- ↑ JF Girmens, A. Erginay, P. Massin et al. Treatment of von Hippel-Lindau retinal hemangioblastoma by the vascular endothelial growth factor receptor inhibitor SU5416 is more effective for associated macular edema than for hemangioblastomas. In: Am J Ophthalmol. 2003; 136, pp. 194-196.
- ↑ a b L. P. Aiello, DJ George, MT Cahill et al. Rapid and durable recovery of visual function in a patient with von Hippel-Lindau syndrome after systemic therapy with vascular endothelial growth factor receptor inhibitor SU5416. In: Ophthalmology. 2002; 109, pp. 1745-1751.
- ↑ S. Madhusudan, G. Deplanque, JP Braybrooke et al. Antiangiogenic therapy for von Hippel-Lindau disease. In: JAMA. 2004; 291, pp. 943-944.
- ^ MI Rosenblatt, DT Azar. Anti-angiogenic therapy: prospects for the treatment of ocular tumors. In: Seminars Ophthalmol. 2006; 21, pp. 151-160.
- ^ AR Webster, ER Maher, AT Moore: Clinical characteristics of ocular angiomatosis in von Hippel – Lindau disease and correlation with germline mutation. In: Arch Ophthalmol. 1999; 117, pp. 371-378.
literature
Books
- Olaf Rieß, Ludger Schöls (Ed.): Neurogenetics. Molecular genetic diagnosis of neurological diseases. Jumper. Berlin 1998, ISBN 3-540-63874-1 .
- P. Lewis. Rowland (Ed.): Merrits Textbook of Neurology. Williams and Wilkins. Baltimore 1995, ISBN 0-683-07400-8 .
- S. Mark. Greenberg: Handbook of Neurosurgery. Lakeland 1997, ISBN 0-9626384-5-5 .
- O. Bruce. Berg (Ed.): Principles of Child Neurology. McGraw-Hill. New York 1996, ISBN 0-07-005193-3 .
- D. Raymond. Adams (Ed.): Principles of Neurology. McGraw-Hill. New York 1997, ISBN 0-07-067439-6 .
Technical article
- JP Constans et al .: Posterior fossa hemangioblastomas. In: Surgical Neurology . 1986, 25, pp. 269-275. PMID 3945908
- DM Hough et al: Pancreatic lesions in von Hippel-Lindau diseas: Prevalence, clinical significance and CT findings. In: Am J Radiol. 1994, 162, pp. 1091-1094. PMID 8165988
- ER Maher et al: Familial renal cell carcinoma. Clinical and molecular genetic aspects. In: Br J Cancer . 1991; 63, pp. 176-179. PMID 1997093
- ER Maher et al.: Von Hippel-Lindau disease: a genetic study. In: J Med Genet. 1991, 28, pp. 443-447. PMID 1895313
- KL Melmon et al: Lindaus disease: Review of the literature and study of a large kindred. In: Am J Med. 1964, 36, pp. 595-617. PMID 14142412
- HPH Neumann et al: Clustering of features of Hippel-Lindau syndrome. In: The Lancet . 1991; 337, pp. 1062-1054. PMID 1673491
- HPH Neumann among others: Von Hippel Lindau Syndrome. In: Brain Pathol . 1995; 5, pp. 181-193. PMID 7670659
- JM Whaley et al .: Germ-line mutations in the von Hippel-Lindau tumor-suppressor genes are similar to somatic von Hippel-Lindau aberrations in sporadic renal cell carcinoma. In: Am J Hum Genet. 1994 Dec; 55 (6), pp. 1092-1102. PMID 7977367