Bruxism
| Classification according to ICD-10 | |
|---|---|
| F45.8 | Other somatoform disorders |
| G47.8 | Other sleep disorders |
| ICD-10 online (WHO version 2019) | |
The bruxism (derived from Greek βρυγμός brygmos , male "gnashing of teeth" with Latin ending) is the unconscious, usually at night, but also during the running teeth grinding or clenching of teeth . As a result, the periodontium wears out due to overload, and the temporomandibular joint , the masticatory muscles and other muscle groups that are tensed to stabilize the head can also be damaged.
This can lead to pain syndromes and ringing in the ears ( tinnitus ). Other common symptoms are dizziness, blurred vision, and nausea. Pain syndromes that affect the temporomandibular joint are referred to in the literature as craniomandibular dysfunction (CMD), for which structural, functional, biochemical and psychological dysregulations of muscle or joint function are responsible.
Sleep - related bruxism (nocturnal teeth grinding) belongs to the sleep - related movement disorders according to the classification system for sleep disorders ICSD-2 and to other sleep disorders (G47.8) or other somatoform disorders (F45.8) according to ICD-10. It also occurs with other sleep disorders such as sleepwalking .
root cause
Scientifically, the clinical picture has been relatively little researched. There are too few studies in the dental literature to be able to speak of reliable findings. It has not yet been clarified to what extent a genetic predisposition plays a role or whether bruxism is always a disease that requires treatment.
Risk factors
As risk factors are and according to studies and surveys. a.
- Sleep disorders ( sleep apnea syndrome , snoring , daytime sleepiness )
- Chronic stress or anxiety
- alcohol
- caffeine
- Smoke
- Certain medications
Effects
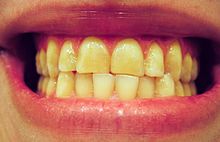
Depending on which structure is the weakest, damage occurs at the weakest point. If the weak point is the tooth support system, bruxism leads to tooth loosening. If the tooth enamel is "soft", it leads to abrasion . If the temporomandibular joint is the weak point, bruxism leads to TMJ problems.
Deviations of the bite position by 0.01 mm from the balanced tooth contact are already perceived. These small deviations can disturb the chewing apparatus to such an extent that bruxism occurs (Kobayashi et al. 1988, double-blind experiment in the sleep laboratory). This tooth contact is perceived as annoying, whereupon an attempt is made to "grind it away". Experimental tooth elevations by 0.1 mm resulted in a series of experiments shortened deep sleep phases , increased adrenaline secretions , and prolonged respiratory arrest times during sleep. After 14 days, the masticatory muscles were so traumatized that there was an increased muscle tone .
The chewing force, which is normally a maximum of 0.4 to 0.45 kN in humans , can increase by a factor of 10, as the pain threshold is increased during night sleep. During the day you would not generate such a high chewing force due to pain.
therapy
The S3 guideline states: "As there is currently no known therapy for curing or eliminating bruxism, the treatment is primarily aimed at protecting the teeth and restorations, reducing bruxism activity and relieving pain." Therapy , instructions for self-observation and an education of the patient about the connections can help. This includes instructions for self- massage of the tense muscles to alleviate the discomfort. However, during sleep there is no control over the reflex activity of the chewing organ. Likewise, physical therapy be displayed. In certain cases this can lead to a reduction in the tone of the masticatory muscles. The success of physiotherapy treatments has only been considered by a few studies, the quality of which has been criticized for various reasons. Further valid studies are necessary here. Psychotherapy may be indicated for stress-related bruxism .
The German Society for Dentistry, Oral and Maxillofacial Medicine (DGZMK) recommends postponing the definitive insertion of dentures if there is a bite problem until this problem has been resolved.
Grinding splint
A splint (bite splint) reduces wear on the teeth. Any interfering contacts that may be present in the event of a bite should be ground in; functional diagnostics can be indicated here . In the case of temporomandibular joint complaints, the construction of the grinding splint should restore the sliding function of the articular disc . Depending on the type of occlusion disorder, different bite corrections or bite aids may be necessary.
The bite splint is not only an abrasion protection, but also relieves the compressed jaw joint and can thus prevent morning pain in the jaw joint.
Biofeedback
There are various attempts at treatment in the field of biofeedback . In one approach, the muscle tension is measured via a probe on the masticatory muscle and acoustically coupled back to the patient, which should make the patient aware of his action. This makes it possible to voluntarily interrupt the chewing impulse. If this is trained, the impulse can possibly be perceived and stopped later even without an acoustic signal via generalization . Dental devices have also been used, namely, capsules which break and release a sharp liquid during bruxism cases. However, no comprehensive, double-blind studies have been carried out to confirm the effectiveness of such biofeedback approaches.
Hypnotherapy
When attempting hypnotherapeutic treatment, a shift of the muscle tension from the jaw to the hand is suggested or an awakening with each grinding of teeth until the habit is changed, or a spontaneous release of tension during sleep. These suggestions are consolidated post-hypnotically and the implementation is checked in a later conversation.
Botulinum toxin
Before using botulinum toxin to treat bruxism, craniomandibular dysfunction (TMJ problems) and to slim down the face, you are warned, as it can lead to massive damage to the jawbone . Botulinum toxin is injected into the masseter muscle to reduce muscle tension. A period of three months between injections, which is usually observed, is not enough to regenerate the lost bone. In some cases, the results show that the jawbone no longer regenerates even in the long term. The bone loss can lead to tooth loosening - up to and including loss of teeth - and increases the risk of fracture of the jawbone.
Bruxism in children
In children, grinding teeth is usually physiological. Before, during and after the change of teeth, children have to bite and grind the occlusion , i.e. the fine-tuning of the clench between the upper and lower row of teeth, which is often accompanied by violent grinding noises, but is not a cause for concern. There are studies in the American literature that see a connection between “idiopathic” scoliosis in adolescents and dysfunctional chewing organ. However, bruxism in children can also be a sign of tension, anxiety, stress, or being overwhelmed.
Definition of the German Society for Dentistry, Oral and Maxillofacial Medicine
The German Society for Dentistry, Oral and Maxillofacial Medicine defines bruxism as a parafunction (grinding, pressing) with non-physiological effects on teeth , periodontium, masticatory muscles and / or the jaw joints .
history
The first publications on this topic go back to the year 1934, the actually fundamental work on this was published by Harold Gelb in 1991 as clinical management of head, neck and TMJ- Pain and dysfunction .
The attempts at dental therapy in the 1970s with extensive " gnathological rehabilitation" were generally unsuccessful.
literature
- WH Miltner: Bruxism. In: W. Miltner, N. Birbaumer, DW Gerber (ed.): Behavioral medicine. Springer-Verlag , Berlin 1986, ISBN 3-540-15438-8 .
See also
Web links
- S3 guideline for the diagnosis and treatment of bruxism. Status: May 2019
- Study on the correlation between stress and bruxism by the University of Düsseldorf published in Head and Face Medicine
- Interview with psychologist Hans-Peter Kuhl about the possible cause of bruxism ( Memento from December 15, 2013 in the Internet Archive )
Individual evidence
- ↑ S3 guideline for non-restful sleep / sleep disorders of the German Society for Sleep Research and Sleep Medicine (DGSM). In: AWMF online (as of 2009)
- ↑ a b c d e f g Maurice M. Ohayon, Kasey K. Li, Christian Guilleminault: Risk Factors for Sleep Bruxism in the General Population. Stanford University School of Medicine, Sleep Disorders Center, Stanford, CA; ( online article )
- ↑ Y. Kobayashi, M. Yokoyoma, H. Shiga, N. Namba: 1198 Sleep Bruxism Condition and in Bruxist. ( Abstract ( Memento from October 16, 2007 in the Internet Archive )), Nippon Dental University, Tokyo, Japan
- ^ A. Oksenberg, E. Arons: Sleep bruxism related to obstructive sleep apnea: the effect of continuous positive airway pressure. ( Abstract ); Sleep Disorders Unit, Loewenstein Hospital-Rehabilitation Center, PO Box 3, Raanana, Israel
- ↑ DK Ng, KL Kwok, G. Poon, KW Chau: Habitual snoring and sleep bruxism in a pediatric outpatient population in Hong Kong. Department of Pediatrics, Kwong Wah Hospital, Waterloo Road, Hong Kong, SAR China. ( Abstract )
- ↑ E. Winocur, A. Gavish, M. Voikovitch, A. Emodi-Perlman, I. Eli: Drugs and bruxism: a critical review. Department of Occlusion and Behavioral Sciences, Maurice and Gabriela Goldschleger, School of Dental Medicine, Tel Aviv University, Tel Aviv, Israel. ( Abstract )
- ^ I. Wilde: Self- observation sheet . (PDF) 2016, accessed on July 3, 2016 .
- ↑ Axel Bumann, Ulrich Lotzmann: Color Atlases of Dentistry, Volume 12, Functional Diagnostics and Therapy Principles . 1st edition. Thieme, Stuttgart 2000, ISBN 3-13-787501-3 .
- ^ S. Shetty, V. Pitti, CL Satish Babu, GP Surendra Kumar, BC Deepthi: Bruxism: a literature review . In: Journal of Indian Prosthodontic Society . tape 10 , no. 3 , September 2010, p. 141-148 , doi : 10.1007 / s13191-011-0041-5 .
- ↑ M. Nissani: A Taste-Based Approach to the Prevention of Bruxism . In: Applied Psychophysiology and Biofeedback . tape 25 , no. 1 , 2000, pp. 43-54 , doi : 10.1023 / A: 1009585422533 (English).
- ↑ KG Raphael, A. Tadinada include: Osteopenic Consequences of botulinum toxin injections in the masticatory muscles: a pilot study. In: Journal of Oral Rehabilitation. Volume 41, 2014, p. 555, doi: 10.1111 / joor.12180 .
- ↑ Is Botox Safe and Effective for TMD? The TMJ Association, Retrieved June 13, 2016.
- ↑ CK Miller: Updates on pediatric feeding and swallowing problems ( Memento of the original from December 15, 2013 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. . (PDF; 82 kB). In: Current opinion in otolaryngology & head and neck surgery. Volume 17, Number 3, June 2009, pp. 194-199, ISSN 1531-6998 . doi: 10.1097 / MOO.0b013e32832b3117 . PMID 19454892 . (Review).
- ↑ Scoliosis: The crooked spine also affects the stomatognathic system , ZR issue 03/2015, February 23, 2015. Retrieved July 11, 2019.
- ↑ L. Höfel: Bruxism in children - the psychological perspective (PDF; 132 kB). Oemus, ZWP, 05/2009.