Parkinsonism: Difference between revisions
Added Christine_2004 ref for "PD is most common cause of parkinsonism." |
RileyOberg (talk | contribs) Corrected term →Neurological |
||
| (466 intermediate revisions by more than 100 users not shown) | |||
| Line 1: | Line 1: | ||
{{cs1 config|name-list-style=vanc|display-authors=6}} |
|||
{{Infobox_Disease |
|||
{{Redirect-distinguish|Parkinson's syndrome|Parkinson's disease}} |
|||
| Name = {{PAGENAME}} |
|||
{{Infobox medical condition (new) |
|||
| Image = |
|||
| name = Parkinsonism |
|||
| synonym = |
|||
| image = Person with Parkinson disease.jpg |
|||
| image_size = |
|||
| alt = |
|||
| caption = |
|||
| pronounce = |
|||
| specialty = |
|||
| symptoms = |
|||
| complications = |
|||
| onset = |
|||
| duration = |
|||
| types = |
|||
| causes = * [[Parkinson's disease]] |
|||
* [[Dementia with Lewy bodies]] |
|||
* [[Parkinson's disease dementia]] |
|||
* [[Neurodegenerative|Other neurodegenerative disorders]], including [[multiple system atrophy]], [[progressive supranuclear palsy]], and [[corticobasal degeneration]] |
|||
* [[Drugs]] |
|||
* [[Toxins]] |
|||
* [[Metabolic disease]] |
|||
* [[Dural arteriovenous fistula]] |
|||
* Dural [[arteriovenous malformation]] |
|||
| risks = |
|||
| diagnosis = |
|||
| differential = |
|||
| prevention = |
|||
| treatment = |
|||
| medication = |
|||
| prognosis = |
|||
| frequency = |
|||
| deaths = |
|||
}} |
}} |
||
'''Parkinsonism''' |
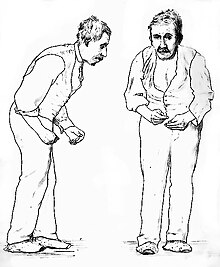
'''Parkinsonism''' is a clinical [[syndrome]] characterized by [[tremor]], [[bradykinesia]] (slowed movements), [[Rigidity (neurology)|rigidity]], and [[balance disorder|postural instability]].<ref name="Aminoff_2005">{{cite book |vauthors=Aminoff MJ, Greenberg DA, Simon RP | title = Clinical Neurology | publisher = Lange: McGraw-Hill Medical | edition = 6th | pages = 241–45 |year = 2005 | isbn = 978-0-07-142360-1 |chapter= Chapter 7: Movement disorders}}</ref><ref name="Role of neuroimaging on differentia">{{cite journal |vauthors=Ogawa T, Fujii S, Kuya K, Kitao SI, Shinohara Y, Ishibashi M, Tanabe Y |title=Role of neuroimaging on differentiation of Parkinson's disease and its related diseases |journal=Yonago Acta Med |volume=61 |issue=3 |pages=145–55 |date=September 2018 |pmid=30275744 |pmc=6158357 |doi=10.33160/yam.2018.09.001|type= Review|quote= Parkinsonian syndromes are a group of movement disorders characterized by classical motor symptoms such as tremors, bradykinesia, and rigidity. They are most frequently due to primary neurodegenerative disease, resulting in the loss of dopaminergic nerve terminals along the nigrostriatal pathway, similar to idiopathic PD, MSA, PSP, CBD, and DLB.}}</ref> Both hypokinetic (bradykinesia and akinesia) as well as hyperkinetic (cogwheel rigidity and tremors at rest) features are displayed by Parkinsonism.<ref name=Ganog/>These are the four [[Parkinson's disease#Motor|motor symptoms]] found in [[Parkinson's disease]] (PD){{snd}}after which it is named{{snd}}[[dementia with Lewy bodies]] (DLB), [[Parkinson's disease dementia]] (PDD), and many other conditions. This set of symptoms occurs in a wide range of conditions and may have many causes, including [[neurodegenerative]] conditions, drugs, [[toxin]]s, [[metabolic disease]]s, and neurological conditions other than PD.<ref>{{cite journal | vauthors = Christine CW, Aminoff MJ | title = Clinical differentiation of parkinsonian syndromes: prognostic and therapeutic relevance | journal = The American Journal of Medicine | volume = 117 | issue = 6 | pages = 412–9 | date = September 2004 | pmid = 15380498 | doi = 10.1016/j.amjmed.2004.03.032 }}</ref> |
||
== Signs and symptoms == |
|||
The underlying causes of parkinsonism are numerous and diagnosis can be complex.<ref name=Tuite_2007>{{cite journal | author = Tuite PJ, Krawczewski K | title = Parkinsonism: a review-of-systems approach to diagnosis | journal = Seminars in neurology | volume = 27 | issue = 2 | pages = 113-22 | year = 2007 | pmid = 17390256 | doi = 10.1055/s-2007-971174}}</ref> If PD has been excluded, the [[differential diagnosis]] or list of potential causes for this disease includes: |
|||
Parkinsonism is a clinical [[syndrome]] characterized by the four [[Parkinson's disease#Motor|motor symptoms]] found in [[Parkinson's disease]]: [[tremor]], [[bradykinesia]] (slowed movements), [[Rigidity (neurology)|rigidity]], and [[balance disorder|postural instability]].<ref name="Aminoff_2005"/><ref name="Role of neuroimaging on differentia"/> |
|||
* [[AIDS]] can sometimes lead to the symptoms of Parkinson's disease, due to commonly causing dopaminergic dysfunction.<ref name=Tse_2004>{{cite journal | author = Tse W, Cersosimo MG, Gracies JM, Morgello S, Olanow CW, Koller W | title = Movement disorders and AIDS: a review | journal = Parkinsonism Relat. Disord. | volume = 10 | issue = 6 | pages = 323-34 | year = 2004 | pmid = 15261874 | doi = 10.1016/j.parkreldis.2004.03.001}}</ref> |
|||
* [[Corticobasal degeneration]] |
|||
* [[Creutzfeldt-Jakob disease]]<ref name=Maltête_2006>{{cite journal | author = Maltête D, Guyant-Maréchal L, Mihout B, Hannequin D | title = Movement disorders and Creutzfeldt-Jakob disease: a review | journal = Parkinsonism Relat. Disord. | volume = 12 | issue = 2 | pages = 65-71 | year = 2006 | pmid = 16364674 | doi = 10.1016/j.parkreldis.2005.10.004}}</ref> |
|||
* [[Diffuse Lewy body disease]] |
|||
* Drug-induced parkinsonism (due to drugs such as [[antipsychotics]], [[metoclopramide]], [[MPTP]]<ref name=Watanabe_2005>{{cite journal | author = Watanabe Y, Himeda T, Araki T | title = Mechanisms of MPTP toxicity and their implications for therapy of Parkinson's disease | journal = Med. Sci. Monit. | volume = 11 | issue = 1 | pages = RA17-23 | year = 2005 | pmid = 15614202 | doi = }}</ref>)<ref name=Aminoff_2005/> |
|||
* [[Encephalitis]] lethargica<ref name=Aminoff_2005/> |
|||
* [[Hallervorden-Spatz syndrome]] |
|||
* [[Multiple system atrophy]] |
|||
* [[Progressive supranuclear palsy]] |
|||
* Toxicity (due to substances such as [[Manganism|manganese]], [[toluene]], [[paraquat]], [[rotenone]], [[hexane]], [[carbon monoxide]], and [[carbon disulfide]]){{cn}} |
|||
* Vascular parkinsonism<ref name=Thanvi_2005>{{cite journal | author = Thanvi B, Lo N, Robinson T | title = Vascular parkinsonism--an important cause of parkinsonism in older people | journal = Age and ageing | volume = 34 | issue = 2 | pages = 114-9 | year = 2005 | pmid = 15713855 | doi = 10.1093/ageing/afi025}}</ref> |
|||
* [[Wilson's disease]]. Wilson's disease is a genetic disorder in which there is an abnormal accumulation of copper. The excess copper can lead to the formation of a copper-dopamine complex, which leads to the oxidation of dopamine to aminochrome. |
|||
Parkinsonism [[gait]] problems can lead to falls and serious physical injuries. Other common symptoms include: |
|||
==References== |
|||
* [[Tremor]]s, as rest tremor (when resting, mostly in the hands) and/or postular tremor |
|||
<!-- --------------------------------------------------------------- |
|||
* Short, [[shuffling gait]] |
|||
See http://en.wikipedia.org/wiki/Wikipedia:Footnotes for a |
|||
* Slow movements ([[bradykinesia]]) |
|||
discussion of different citation methods and how to generate |
|||
* Loss of [[perception#Sound|sound perception]] leading to soft speech, [[hypophonia]]<ref>{{cite journal |last1=Kwan |first1=Lorinda C. |last2=Whitehill |first2=Tara L. |date=2011 |title=Perception of Speech by Individuals with Parkinson's Disease: A Review |journal=Parkinson's Disease |volume=2011 |pages=389767 |doi=10.4061/2011/389767 |issn=2090-8083 |pmc=3179876 |pmid=21961077 |doi-access=free }}</ref> |
|||
footnotes using the <ref> & </ref> tags and the {{Reflist}} template |
|||
* [[Difficulty sleeping]] |
|||
-------------------------------------------------------------------- --> |
|||
* [[Dry skin]] |
|||
{{Reflist|2}} |
|||
* [[Apathy]] |
|||
* [[Hypomimia|Lack of facial expressions]] |
|||
* [[Balance problems]] |
|||
* Frequent [[Falling (accident)|falls]] |
|||
* [[Micrographia (handwriting)|Very small handwriting]] |
|||
* [[Hypertonia|Rigid, stiff muscles]] |
|||
* [[Cogwheeling]] (jerky feeling in arm or leg) |
|||
* Upgaze impairment |
|||
* Plastic, dead feeling resistance known as "[[lead-pipe rigidity]]".<ref name="Ganog">{{cite book |last1=Barrett |first1=Kim E. |last2=Barman |first2=Susan M. |last3=Brooks |first3=Heddwen L. |last4=Yuan |first4=Jason |title=Ganong's Review of Medical Physiology |date=21 January 2019 |publisher=McGraw Hill |isbn=978-1-260-12241-1 |edition=26 |url=https://books.google.com/books?id=JuN8DwAAQBAJ |access-date=1 April 2024}}</ref> |
|||
== Conditions== |
|||
[[Category:Neurology]] |
|||
Parkinsonism occurs in many conditions. |
|||
=== Neurological === |
|||
[[Neurodegenerative]] conditions and [[Parkinson plus syndrome|Parkinson-plus syndrome]]s that can cause parkinsonism include:<ref name="Bradley2004">{{cite book|title= Neurology in Clinical Practice: Principles of diagnosis and management |volume= 1 |editor= Bradley, Walter George |publisher= Taylor & Francis |year= 2004 |chapter= Diagnosis and Assessment |vauthors= Jankovic J, Lang AE |pages= [https://books.google.com/books?id=vOQqyNhTDl0C&q=parkinsonism&pg=PA294 295–96] | isbn= 978-99976-25-88-5}}</ref> |
|||
* [[Corticobasal degeneration]]<ref name="Bradley2004" /> |
|||
* [[Dementia with Lewy bodies]]<ref name="Bradley2004" /> |
|||
* The relationship (if any) with [[essential tremor]] is not clear.<ref>{{cite journal | vauthors = Algarni M, Fasano A | title = The overlap between Essential tremor and Parkinson disease | journal = Parkinsonism & Related Disorders | volume = 46 | pages = S101–S104 | date = January 2018 | issue = Suppl 1 | pmid = 28729090 | doi = 10.1016/j.parkreldis.2017.07.006 | url = https://www.prd-journal.com/article/S1353-8020(17)30239-0/abstract?code=prd-site }}</ref> |
|||
* [[Frontotemporal dementia]] ([[Pick's disease]])<ref name="Finger2016">{{cite journal | vauthors = Finger EC | title = Frontotemporal Dementias | journal = Continuum | volume = 22 | issue = 2 Dementia | pages = 464–89 | date = April 2016 | pmid = 27042904 | pmc = 5390934 | doi = 10.1212/CON.0000000000000300 | type = Review }}</ref> |
|||
* [[Gerstmann–Sträussler–Scheinker syndrome]]<ref name="Bradley2004" /> |
|||
* [[Huntington's disease]]<ref name="Bradley2004" /> |
|||
* [[Lytico-bodig disease]] ([[ALS]] complex of Guam)<ref name="Bradley2004" /> |
|||
* [[Multiple system atrophy]] ([[Shy–Drager syndrome]])<ref name="Bradley2004" /> |
|||
* [[Neuroacanthocytosis]]<ref name="Bradley2004" /> |
|||
* [[Neuronal ceroid lipofuscinosis]]<ref name="Bradley2004" /> |
|||
* [[Olivopontocerebellar atrophy]]<ref name="Bradley2004" /> |
|||
* [[Pantothenate kinase-associated neurodegeneration]], also known as [[neurodegeneration with brain iron accumulation]]<ref name="Bradley2004" /> |
|||
* [[Parkin mutation]] causing [[hereditary juvenile dystonia]]<ref name="Bradley2004" /> |
|||
* [[Parkinson's disease]]<ref name="Bradley2004" /> |
|||
* [[Parkinson's disease dementia]]<ref name="McKeithConsensus2017">{{cite journal | vauthors = McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, Aarsland D, Galvin J, Attems J, Ballard CG, Bayston A, Beach TG, Blanc F, Bohnen N, Bonanni L, Bras J, Brundin P, Burn D, Chen-Plotkin A, Duda JE, El-Agnaf O, Feldman H, Ferman TJ, Ffytche D, Fujishiro H, Galasko D, Goldman JG, Gomperts SN, Graff-Radford NR, Honig LS, Iranzo A, Kantarci K, Kaufer D, Kukull W, Lee VM, Leverenz JB, Lewis S, Lippa C, Lunde A, Masellis M, Masliah E, McLean P, Mollenhauer B, Montine TJ, Moreno E, Mori E, Murray M, O'Brien JT, Orimo S, Postuma RB, Ramaswamy S, Ross OA, Salmon DP, Singleton A, Taylor A, Thomas A, Tiraboschi P, Toledo JB, Trojanowski JQ, Tsuang D, Walker Z, Yamada M, Kosaka K | title = Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium | journal = Neurology | volume = 89 | issue = 1 | pages = 88–100 | date = July 2017 | pmid = 28592453 | pmc = 5496518 | doi = 10.1212/WNL.0000000000004058 | type = Review }}</ref> |
|||
* [[Progressive supranuclear palsy]]<ref name="Bradley2004" /> |
|||
* [[Wilson's disease]]<ref name="Bradley2004" /> |
|||
* [[X-linked dystonia parkinsonism]] ([[Lubag Syndrome|Lubag syndrome]])<ref name="Bradley2004" /> |
|||
=== Infectious === |
|||
* [[Creutzfeldt–Jakob disease]]<ref name="Bradley2004" /><ref>{{cite journal | vauthors = Maltête D, Guyant-Maréchal L, Mihout B, Hannequin D | title = Movement disorders and Creutzfeldt-Jakob disease: a review | journal = Parkinsonism & Related Disorders | volume = 12 | issue = 2 | pages = 65–71 | date = March 2006 | pmid = 16364674 | doi = 10.1016/j.parkreldis.2005.10.004 }}</ref> |
|||
* [[Encephalitis lethargica]]<ref name="Aminoff_2005" /> |
|||
* [[HIV]] infection<ref name="Bradley2004" /> and [[AIDS]]<ref name="Bradley2004" /><ref>{{cite journal | vauthors = Tse W, Cersosimo MG, Gracies JM, Morgello S, Olanow CW, Koller W | title = Movement disorders and AIDS: a review | journal = Parkinsonism & Related Disorders | volume = 10 | issue = 6 | pages = 323–34 | date = August 2004 | pmid = 15261874 | doi = 10.1016/j.parkreldis.2004.03.001 }}</ref> |
|||
=== Toxins === |
|||
Evidence exists to show a link between exposure to [[pesticides]] and [[herbicides]] and PD; a two-fold increase in risk was seen with [[paraquat]] or [[maneb]]/[[mancozeb]] exposure.<ref name="Pezzoli2013">{{cite journal | vauthors = Pezzoli G, Cereda E | title = Exposure to pesticides or solvents and risk of Parkinson disease | journal = Neurology | volume = 80 | issue = 22 | pages = 2035–41 | date = May 2013 | pmid = 23713084 | doi = 10.1212/WNL.0b013e318294b3c8 | s2cid = 13628268 | type = Meta-analysis }}</ref> |
|||
Chronic [[manganese]] (Mn) exposure has been shown to produce a parkinsonism-like illness characterized by movement abnormalities.<ref name="Guilarte2015">{{cite journal | vauthors = Guilarte TR, Gonzales KK | title = Manganese-Induced Parkinsonism Is Not Idiopathic Parkinson's Disease: Environmental and Genetic Evidence | journal = Toxicological Sciences | volume = 146 | issue = 2 | pages = 204–12 | date = August 2015 | pmid = 26220508 | pmc = 4607750 | doi = 10.1093/toxsci/kfv099 | type = Review }}</ref> This condition is not responsive to [[Management of Parkinson's disease|typical therapies used in the treatment of PD]], suggesting an alternative pathway than the typical [[dopamine]]rgic loss within the [[substantia nigra]].<ref name="Guilarte2015" /> Manganese may accumulate in the [[basal ganglia]], leading to the abnormal movements that characterize parkinsonism.<ref name="Kwakye2015">{{cite journal | vauthors = Kwakye GF, Paoliello MM, Mukhopadhyay S, Bowman AB, Aschner M | title = Manganese-Induced Parkinsonism and Parkinson's Disease: Shared and Distinguishable Features | journal = International Journal of Environmental Research and Public Health | volume = 12 | issue = 7 | pages = 7519–40 | date = July 2015 | pmid = 26154659 | pmc = 4515672 | doi = 10.3390/ijerph120707519 | type = Review | doi-access = free }}</ref> A mutation of the [[SLC30A10]] gene, a manganese efflux transporter necessary for decreasing intracellular Mn, has been linked with the development of this parkinsonism-like disease.<ref name="Peres2016">{{cite journal | vauthors = Peres TV, Schettinger MR, Chen P, Carvalho F, Avila DS, Bowman AB, Aschner M | title = Manganese-induced neurotoxicity: a review of its behavioral consequences and neuroprotective strategies | journal = BMC Pharmacology & Toxicology | volume = 17 | issue = 1 | pages = 57 | date = November 2016 | pmid = 27814772 | pmc = 5097420 | doi = 10.1186/s40360-016-0099-0 | type = Review | doi-access = free }}</ref> The [[Lewy body|Lewy bodies]] typical to PD are not seen in Mn-induced parkinsonism.<ref name="Kwakye2015" /> |
|||
[[Agent Orange]] may be a cause of parkinsonism, although evidence is inconclusive and further research is needed.<ref name=McKnight2020>{{cite journal |vauthors=McKnight S, Hack N |title=Toxin-Induced Parkinsonism |journal=Neurol Clin |volume=38 |issue=4 |pages=853–865 |date=November 2020 |pmid=33040865 |doi=10.1016/j.ncl.2020.08.003 |s2cid=222299758 |type= Review|doi-access=free }}</ref> |
|||
Other toxins that have been associated with parkinsonism are: |
|||
* [[Annonaceae]]<ref>{{cite journal | vauthors = Carod-Artal FJ | title = [Neurological syndromes linked with the intake of plants and fungi containing a toxic component (I). Neurotoxic syndromes caused by the ingestion of plants, seeds and fruits] | language = es | journal = Revista de Neurología | volume = 36 | issue = 9 | pages = 860–71 | date = 2003 | pmid = 12717675 | type = Review }}</ref> |
|||
* [[Carbon monoxide]]<ref name="Bradley2004" /> |
|||
* [[Carbon disulfide]]<ref name="Bradley2004" /> |
|||
* [[Cyanide]]<ref name="Bradley2004" /> |
|||
* [[Ethanol]]<ref name="Bradley2004" /> |
|||
* [[Hexane]]<ref name="Kim2010">{{cite journal | vauthors = Kim EA, Kang SK | title = Occupational neurological disorders in Korea | journal = Journal of Korean Medical Science | volume = 25 | issue = Suppl | pages = S26-35 | date = December 2010 | pmid = 21258587 | pmc = 3023358 | doi = 10.3346/jkms.2010.25.S.S26 | type = Review }}</ref> |
|||
* [[Mercury (element)|Mercury]]<ref name="Bradley2004" /> |
|||
* [[Methanol]]<ref name="Bradley2004" /> |
|||
* [[MPTP]]<ref name="Bradley2004" /><ref name="Watanabe_2005">{{cite journal | vauthors = Watanabe Y, Himeda T, Araki T | title = Mechanisms of MPTP toxicity and their implications for therapy of Parkinson's disease | journal = Medical Science Monitor | volume = 11 | issue = 1 | pages = RA17-23 | date = January 2005 | pmid = 15614202 | url = http://www.medscimonit.com/pub/vol_11/no_1/5333.pdf }}</ref> |
|||
* [[Rotenone]]<ref name="Nandipati">{{cite journal | vauthors = Nandipati S, Litvan I | title = Environmental Exposures and Parkinson's Disease | journal = International Journal of Environmental Research and Public Health | volume = 13 | issue = 9 | pages = 881 | date = September 2016 | pmid = 27598189 | pmc = 5036714 | doi = 10.3390/ijerph13090881 | type = Review | doi-access = free }}</ref> |
|||
* [[Toluene]]<ref>Weiss J. Chapter 151. Toluene and Xylene. In: Olson KR, ed. Poisoning & Drug Overdose. 6th ed. New York: McGraw-Hill; 2012. http://www.accessmedicine.com/content.aspx?aID=55982958. Accessed April 21, 2013.</ref> ([[inhalant abuse]]: "huffing")<ref>{{cite journal | vauthors = Uitti RJ, Snow BJ, Shinotoh H, Vingerhoets FJ, Hayward M, Hashimoto S, Richmond J, Markey SP, Markey CJ, Calne DB | title = Parkinsonism induced by solvent abuse | journal = Annals of Neurology | volume = 35 | issue = 5 | pages = 616–9 | date = May 1994 | pmid = 8179306 | doi = 10.1002/ana.410350516 | s2cid = 23657208 }}</ref> |
|||
=== Vascular === |
|||
* [[Binswanger's disease]] (subcortical [[leukoencephalopathy]])<ref name="Bradley2004" /> |
|||
* [[Vascular dementia]] (multi-infarct)<ref name="Bradley2004" /> |
|||
* [[Dural arteriovenous fistula]] / dAVF (reversible parkinsonism through fistula treatment) <ref>{{cite journal |last1=Lai |first1=Joshua |last2=Heran |first2=Manraj K.S. |last3=Stoessl |first3=A. Jon |last4=Gooderham |first4=Peter A. |date=2017-03-27 |title=Reversible Parkinsonism and Rapidly Progressive Dementia Due to Dural Arteriovenous Fistula: Case Series and Literature Review |journal=Movement Disorders Clinical Practice |volume=4 |issue=4 |pages=607–611 |doi=10.1002/mdc3.12480 |issn=2330-1619 |pmc=6174482 |pmid=30363443}}</ref><ref>{{cite journal |last1=Matsuda |first1=S. |last2=Waragai |first2=M. |last3=Shinotoh |first3=H. |last4=Takahashi |first4=N. |last5=Takagi |first5=K. |last6=Hattori |first6=T. |date=1999-05-01 |title=Intracranial dural arteriovenous fistula (DAVF) presenting progressive dementia and parkinsonism |url=https://pubmed.ncbi.nlm.nih.gov/10426146/ |journal=Journal of the Neurological Sciences |volume=165 |issue=1 |pages=43–47 |doi=10.1016/s0022-510x(99)00075-1 |issn=0022-510X |pmid=10426146|s2cid=31594108 }}</ref><ref>{{cite journal |last1=Kim |first1=Hang Rai |last2=Lee |first2=Jee-Young |last3=Kim |first3=Yu Kyeong |last4=Park |first4=Hyeyoung |last5=Kim |first5=Han-Joon |last6=Son |first6=Young-Je |last7=Jeon |first7=Beom Seok |date=September 2015 |title=Dural Arteriovenous Fistula-Associated Reversible Parkinsonism with Presynaptic Dopaminergic Loss |journal=Journal of Movement Disorders |volume=8 |issue=3 |pages=141–143 |doi=10.14802/jmd.15021 |issn=2005-940X |pmc=4572665 |pmid=26413242}}</ref> |
|||
* Dural arteriovenous malformation / dAVM (reversible through dAVM treatment) <ref>{{cite journal |last1=Goldstein |first1=S. |last2=Friedman |first2=J. H. |last3=Innis |first3=R. |last4=Seibyl |first4=J. |last5=Marek |first5=K. |date=March 2001 |title=Hemi-parkinsonism due to a midbrain arteriovenous malformation: dopamine transporter imaging |url=https://pubmed.ncbi.nlm.nih.gov/11295793/ |journal=Movement Disorders|volume=16 |issue=2 |pages=350–353 |doi=10.1002/mds.1047 |issn=0885-3185 |pmid=11295793|s2cid=22701874 }}</ref><ref>{{cite journal |last1=Armenteros |first1=Patricia Rodrigo |last2=Kapetanovic |first2=Solange |last3=Lopez |first3=Sonia Gonzalez |last4=Vazquez-Lorenzo |first4=Enrique |last5=Mendez |first5=Lander Anton |last6=Muga |first6=Juan Jose Gomez |last7=Deza |first7=Edison Santos Morales |last8=Iriarte |first8=Markel Erburu |last9=Garcia-Monco |first9=Juan Carlos |date=2022-03-29 |title=Pearls & Oy-sters: Arteriovenous Malformation With Sinus Thrombosis and Thalamic Hemorrhage: Unusual Cause of Parkinsonism and Dementia |url=https://n.neurology.org/content/98/13/550 |journal=Neurology |language=en |volume=98 |issue=13 |pages=550–553 |doi=10.1212/WNL.0000000000200016 |issn=0028-3878 |pmid=35121672|s2cid=246556634 |doi-access=free }}</ref> |
|||
=== Other === |
|||
* [[Chronic traumatic encephalopathy]] (boxer's dementia or pugilistic encephalopathy)<ref name="Bradley2004" /> |
|||
* Damage to the [[brain stem]] (especially dopaminergic nuclei of the [[substantia nigra]]),<ref>{{cite journal | vauthors = Jubault T, Brambati SM, Degroot C, Kullmann B, Strafella AP, Lafontaine AL, Chouinard S, Monchi O | title = Regional brain stem atrophy in idiopathic Parkinson's disease detected by anatomical MRI | journal = PLOS ONE | volume = 4 | issue = 12 | pages = e8247 | date = December 2009 | pmid = 20011063 | pmc = 2784293 | doi = 10.1371/journal.pone.0008247|editor1-link=Howard E. Gendelman | editor-first = Howard E. | editor-last = Gendelman | bibcode = 2009PLoSO...4.8247J | doi-access = free }}</ref>[[basal ganglia]] (especially [[globus pallidus]])<ref>{{cite journal | vauthors = Kuoppamäki M, Rothwell JC, Brown RG, Quinn N, Bhatia KP, Jahanshahi M | title = Parkinsonism following bilateral lesions of the globus pallidus: performance on a variety of motor tasks shows similarities with Parkinson's disease | journal = Journal of Neurology, Neurosurgery, and Psychiatry | volume = 76 | issue = 4 | pages = 482–90 | date = April 2005 | pmid = 15774432 | pmc = 1739601 | doi = 10.1136/jnnp.2003.020800 }}</ref> and the [[thalamus]].<ref>{{cite journal|last=Halliday|first=Glenda M.|date=2009-12-15|title=Thalamic changes in Parkinson's disease|journal=Parkinsonism & Related Disorders|language=en|volume=15|pages=S152–S155|doi=10.1016/S1353-8020(09)70804-1|pmid=20082979}}</ref> |
|||
* [[Hypothyroidism]]<ref name="Bradley2004" /> |
|||
* [[Orthostatic tremor]]<ref>{{cite journal | vauthors = Apartis E, Tison F, Arné P, Jedynak CP, Vidailhet M | title = Fast orthostatic tremor in Parkinson's disease mimicking primary orthostatic tremor | journal = Movement Disorders | volume = 16 | issue = 6 | pages = 1133–6 | date = November 2001 | pmid = 11748748 | doi = 10.1002/mds.1218 | s2cid = 36301428 }}</ref> |
|||
* [[Paraneoplastic syndrome]]: neurological symptoms caused by antibodies associated with cancers<ref>{{cite journal | vauthors = Panzer J, Dalmau J | title = Movement disorders in paraneoplastic and autoimmune disease | journal = Current Opinion in Neurology | volume = 24 | issue = 4 | pages = 346–53 | date = August 2011 | pmid = 21577108 | pmc = 3705177 | doi = 10.1097/WCO.0b013e328347b307 }}</ref> |
|||
* Rapid onset dystonia parkinsonism<ref>{{cite journal | vauthors = Liu Y, Lu Y, Zhang X, Xie S, Wang T, Wu T, Wang C | title = A case of rapid-onset dystonia-parkinsonism accompanied by pyramidal tract impairment | journal = BMC Neurology | volume = 16 | issue = 1 | pages = 218 | date = November 2016 | pmid = 27835968 | pmc = 5105251 | doi = 10.1186/s12883-016-0743-8 | doi-access = free }}</ref> |
|||
* Autosomal recessive juvenile parkinsonism<ref>{{cite journal | vauthors = Saito M, Maruyama M, Ikeuchi K, Kondo H, Ishikawa A, Yuasa T, Tsuji S | title = Autosomal recessive juvenile parkinsonism | journal = Brain & Development | volume = 22 | pages = S115-7 | date = September 2000 | issue = Suppl 1 | doi = 10.1016/s0387-7604(00)00137-6 | pmid = 10984671 | s2cid = 22733500 }}</ref> |
|||
==Differential diagnosis == |
|||
Secondary parkinsonism, including vascular parkinsonism and drug-induced parkinsonism.<ref>{{cite journal |vauthors=Del Toro-Pérez C, Guevara-Sánchez E, Martínez-Sánchez P |title=Treatment of Vascular Parkinsonism: A Systematic Review |journal=Brain Sci |volume=13 |issue=3 |date=March 2023 |page=489 |pmid=36979299 |pmc=10046744 |doi=10.3390/brainsci13030489 |url= |doi-access=free }}</ref><ref>{{cite journal |vauthors=Shin HW, Hong SW, Youn YC |title=Clinical Aspects of the Differential Diagnosis of Parkinson's Disease and Parkinsonism |journal=J Clin Neurol |volume=18 |issue=3 |pages=259–270 |date=May 2022 |pmid=35589315 |pmc=9163948 |doi=10.3988/jcn.2022.18.3.259 |url=}}</ref> |
|||
=== Drug-induced ("pseudoparkinsonism") === |
|||
About 7% of people with parkinsonism developed symptoms as a result of side effects of medications, mainly neuroleptic [[antipsychotic]]s especially the [[phenothiazine]]s (such as [[perphenazine]] and [[chlorpromazine]]), [[thioxanthene]]s (such as [[Flupentixol|flupenthixol]] and [[zuclopenthixol]]) and [[butyrophenone]]s (such as [[haloperidol]]), and rarely, antidepressants. Yet another drug that can induce parkinsonism is the [[antihistaminic]] medication [[cinnarizine]], usually prescribed for motion sickness; this is because besides antagonizing [[histamine receptors]] this drug antagonizes the [[dopamine D2 receptor]]s.<ref name="Marti-Masso" /> The incidence of drug-induced parkinsonism increases with age. Drug-induced parkinsonism tends to remain at its presenting level and does not worsen like Parkinson's disease.<ref>{{cite web | url = http://www.parkinsons.org.uk/PDF/FS38_druginducedparkinsonism.pdf | title = Information Sheet: Drug-induced Parkinsonism | publisher = Parkinson's Disease and Society |access-date = 2013-04-15 | url-status = dead | archive-url = https://web.archive.org/web/20130626024034/http://www.parkinsons.org.uk/PDF/FS38_druginducedparkinsonism.pdf | archive-date = 2013-06-26 }}</ref> |
|||
Implicated medications include: |
|||
* [[Antipsychotics]]<ref name="Bradley2004" /> |
|||
* [[Lithium (medication)|Lithium]]<ref name="Bradley2004" /> |
|||
* [[Metoclopramide]]<ref>{{cite journal | vauthors = Shuaib UA, Rajput AH, Robinson CA, Rajput A | title = Neuroleptic-induced Parkinsonism: Clinicopathological study | journal = Movement Disorders | volume = 31 | issue = 3 | pages = 360–5 | date = March 2016 | pmid = 26660063 | pmc = 5064745 | doi = 10.1002/mds.26467 }}</ref> |
|||
* [[MDMA]] (addiction and frequent use)<ref>{{cite journal | vauthors = Louis ED, Ottman R | title = Is there a one-way street from essential tremor to Parkinson's disease? Possible biological ramifications | journal = European Journal of Neurology | volume = 20 | issue = 11 | pages = 1440–4 | date = November 2013 | pmid = 24033795 | pmc = 3801177 | doi = 10.1111/ene.12256 | type = Review }}</ref><ref>{{cite journal |author=Fabrizi, Monaco, Dalla Libera |title=Parkinsonian syndrome following MDMA (Ecstasy) addiction |journal=Movement Disorders |volume=19 |pages=S73–S74 |year=2004}}</ref> |
|||
* [[Tetrabenazine]]<ref name="Bradley2004" /> |
|||
* [[Cinnarizine]]<ref name="Marti-Masso">{{cite journal |first1=José F. |first2=Juan J. |url=https://movementdisorders.onlinelibrary.wiley.com/doi/10.1002/mds.870130313 |journal=Movement Disorders |publisher=International Parkinson and Movement Disorder Society/Wiley |issn=1531-8257 |editor1-first=A. Jon |editor1-last=Stoessl |editor2-first=Christine |editor2-last=Klein |editor3-first=David G. |editor3-last=Standaert |publication-place=[[Vancouver]], [[British Columbia]], [[Canada]] |title=Cinnarizine-induced parkinsonism: ten years later |last1=Martí-Massó |last2=Poza |doi=10.1002/mds.870130313 |pmid=9613736 |date=1 May 1998 |volume=13 |issue=3 |pages=453–456 |
|||
|s2cid=31516105 }}</ref> |
|||
== Society and culture == |
|||
In the United States, the 2021 [[National Defense Authorization Act]] (NDAA) added parkinsonism to the list of presumptive conditions associated with [[Agent Orange]] exposure, enabling affected service members to receive [[United States Department of Veterans Affairs|Veterans Affairs]] disability benefits.<ref name= VAParkinsonism>{{cite web |url= https://www.publichealth.va.gov/exposures/publications/agent-orange/agent-orange-2021/presumptions.asp |title= VA adds three new Agent Orange presumptions |publisher= U. S. Department of Veteran Affairs |date= September 10, 2021 |access-date= March 2, 2022}}</ref> |
|||
== References == |
|||
{{Reflist|32em}} |
|||
== External links == |
|||
* [https://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=perry GeneReviews/NIH/NCBI/UW entry on Perry syndrome] |
|||
* [https://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=xdp GeneReviews/NCBI/NIH/UW entry on X-Linked Dystonia-Parkinsonism] |
|||
{{CNS diseases of the nervous system}} |
|||
{{Antiparkinson agents}} |
|||
{{Medical resources |
|||
| DiseasesDB = 24212 |
|||
| ICD11 = {{ICD11|8A00}} |
|||
| ICD10 = {{ICD10|G20}}, {{ICD10|G21}}, {{ICD10|G22}} |
|||
| ICD9 = {{ICD9|332}} |
|||
| ICDO = |
|||
| OMIM = |
|||
| MedlinePlus = 000759 |
|||
| eMedicineSubj = |
|||
| eMedicineTopic = |
|||
| MeshID = D020734 |
|||
}} |
|||
{{Authority control}} |
|||
[[Category:Extrapyramidal and movement disorders]] |
|||
[[Category:Geriatrics]] |
[[Category:Geriatrics]] |
||
[[Category:Parkinson's disease]] |
|||
Latest revision as of 12:24, 17 April 2024
| Parkinsonism | |
|---|---|
 | |
| Specialty | Neurology |
| Causes | |
Parkinsonism is a clinical syndrome characterized by tremor, bradykinesia (slowed movements), rigidity, and postural instability.[1][2] Both hypokinetic (bradykinesia and akinesia) as well as hyperkinetic (cogwheel rigidity and tremors at rest) features are displayed by Parkinsonism.[3]These are the four motor symptoms found in Parkinson's disease (PD) – after which it is named – dementia with Lewy bodies (DLB), Parkinson's disease dementia (PDD), and many other conditions. This set of symptoms occurs in a wide range of conditions and may have many causes, including neurodegenerative conditions, drugs, toxins, metabolic diseases, and neurological conditions other than PD.[4]
Signs and symptoms[edit]
Parkinsonism is a clinical syndrome characterized by the four motor symptoms found in Parkinson's disease: tremor, bradykinesia (slowed movements), rigidity, and postural instability.[1][2]
Parkinsonism gait problems can lead to falls and serious physical injuries. Other common symptoms include:
- Tremors, as rest tremor (when resting, mostly in the hands) and/or postular tremor
- Short, shuffling gait
- Slow movements (bradykinesia)
- Loss of sound perception leading to soft speech, hypophonia[5]
- Difficulty sleeping
- Dry skin
- Apathy
- Lack of facial expressions
- Balance problems
- Frequent falls
- Very small handwriting
- Rigid, stiff muscles
- Cogwheeling (jerky feeling in arm or leg)
- Upgaze impairment
- Plastic, dead feeling resistance known as "lead-pipe rigidity".[3]
Conditions[edit]
Parkinsonism occurs in many conditions.
Neurological[edit]
Neurodegenerative conditions and Parkinson-plus syndromes that can cause parkinsonism include:[6]
- Corticobasal degeneration[6]
- Dementia with Lewy bodies[6]
- The relationship (if any) with essential tremor is not clear.[7]
- Frontotemporal dementia (Pick's disease)[8]
- Gerstmann–Sträussler–Scheinker syndrome[6]
- Huntington's disease[6]
- Lytico-bodig disease (ALS complex of Guam)[6]
- Multiple system atrophy (Shy–Drager syndrome)[6]
- Neuroacanthocytosis[6]
- Neuronal ceroid lipofuscinosis[6]
- Olivopontocerebellar atrophy[6]
- Pantothenate kinase-associated neurodegeneration, also known as neurodegeneration with brain iron accumulation[6]
- Parkin mutation causing hereditary juvenile dystonia[6]
- Parkinson's disease[6]
- Parkinson's disease dementia[9]
- Progressive supranuclear palsy[6]
- Wilson's disease[6]
- X-linked dystonia parkinsonism (Lubag syndrome)[6]
Infectious[edit]
Toxins[edit]
Evidence exists to show a link between exposure to pesticides and herbicides and PD; a two-fold increase in risk was seen with paraquat or maneb/mancozeb exposure.[12]
Chronic manganese (Mn) exposure has been shown to produce a parkinsonism-like illness characterized by movement abnormalities.[13] This condition is not responsive to typical therapies used in the treatment of PD, suggesting an alternative pathway than the typical dopaminergic loss within the substantia nigra.[13] Manganese may accumulate in the basal ganglia, leading to the abnormal movements that characterize parkinsonism.[14] A mutation of the SLC30A10 gene, a manganese efflux transporter necessary for decreasing intracellular Mn, has been linked with the development of this parkinsonism-like disease.[15] The Lewy bodies typical to PD are not seen in Mn-induced parkinsonism.[14]
Agent Orange may be a cause of parkinsonism, although evidence is inconclusive and further research is needed.[16]
Other toxins that have been associated with parkinsonism are:
- Annonaceae[17]
- Carbon monoxide[6]
- Carbon disulfide[6]
- Cyanide[6]
- Ethanol[6]
- Hexane[18]
- Mercury[6]
- Methanol[6]
- MPTP[6][19]
- Rotenone[20]
- Toluene[21] (inhalant abuse: "huffing")[22]
Vascular[edit]
- Binswanger's disease (subcortical leukoencephalopathy)[6]
- Vascular dementia (multi-infarct)[6]
- Dural arteriovenous fistula / dAVF (reversible parkinsonism through fistula treatment) [23][24][25]
- Dural arteriovenous malformation / dAVM (reversible through dAVM treatment) [26][27]
Other[edit]
- Chronic traumatic encephalopathy (boxer's dementia or pugilistic encephalopathy)[6]
- Damage to the brain stem (especially dopaminergic nuclei of the substantia nigra),[28]basal ganglia (especially globus pallidus)[29] and the thalamus.[30]
- Hypothyroidism[6]
- Orthostatic tremor[31]
- Paraneoplastic syndrome: neurological symptoms caused by antibodies associated with cancers[32]
- Rapid onset dystonia parkinsonism[33]
- Autosomal recessive juvenile parkinsonism[34]
Differential diagnosis[edit]
Secondary parkinsonism, including vascular parkinsonism and drug-induced parkinsonism.[35][36]
Drug-induced ("pseudoparkinsonism")[edit]
About 7% of people with parkinsonism developed symptoms as a result of side effects of medications, mainly neuroleptic antipsychotics especially the phenothiazines (such as perphenazine and chlorpromazine), thioxanthenes (such as flupenthixol and zuclopenthixol) and butyrophenones (such as haloperidol), and rarely, antidepressants. Yet another drug that can induce parkinsonism is the antihistaminic medication cinnarizine, usually prescribed for motion sickness; this is because besides antagonizing histamine receptors this drug antagonizes the dopamine D2 receptors.[37] The incidence of drug-induced parkinsonism increases with age. Drug-induced parkinsonism tends to remain at its presenting level and does not worsen like Parkinson's disease.[38]
Implicated medications include:
- Antipsychotics[6]
- Lithium[6]
- Metoclopramide[39]
- MDMA (addiction and frequent use)[40][41]
- Tetrabenazine[6]
- Cinnarizine[37]
Society and culture[edit]
In the United States, the 2021 National Defense Authorization Act (NDAA) added parkinsonism to the list of presumptive conditions associated with Agent Orange exposure, enabling affected service members to receive Veterans Affairs disability benefits.[42]
References[edit]
- ^ a b c Aminoff MJ, Greenberg DA, Simon RP (2005). "Chapter 7: Movement disorders". Clinical Neurology (6th ed.). Lange: McGraw-Hill Medical. pp. 241–45. ISBN 978-0-07-142360-1.
- ^ a b Ogawa T, Fujii S, Kuya K, Kitao SI, Shinohara Y, Ishibashi M, et al. (September 2018). "Role of neuroimaging on differentiation of Parkinson's disease and its related diseases". Yonago Acta Med (Review). 61 (3): 145–55. doi:10.33160/yam.2018.09.001. PMC 6158357. PMID 30275744.
Parkinsonian syndromes are a group of movement disorders characterized by classical motor symptoms such as tremors, bradykinesia, and rigidity. They are most frequently due to primary neurodegenerative disease, resulting in the loss of dopaminergic nerve terminals along the nigrostriatal pathway, similar to idiopathic PD, MSA, PSP, CBD, and DLB.
- ^ a b Barrett KE, Barman SM, Brooks HL, Yuan J (21 January 2019). Ganong's Review of Medical Physiology (26 ed.). McGraw Hill. ISBN 978-1-260-12241-1. Retrieved 1 April 2024.
- ^ Christine CW, Aminoff MJ (September 2004). "Clinical differentiation of parkinsonian syndromes: prognostic and therapeutic relevance". The American Journal of Medicine. 117 (6): 412–9. doi:10.1016/j.amjmed.2004.03.032. PMID 15380498.
- ^ Kwan LC, Whitehill TL (2011). "Perception of Speech by Individuals with Parkinson's Disease: A Review". Parkinson's Disease. 2011: 389767. doi:10.4061/2011/389767. ISSN 2090-8083. PMC 3179876. PMID 21961077.
- ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag Jankovic J, Lang AE (2004). "Diagnosis and Assessment". In Bradley, Walter George (ed.). Neurology in Clinical Practice: Principles of diagnosis and management. Vol. 1. Taylor & Francis. pp. 295–96. ISBN 978-99976-25-88-5.
- ^ Algarni M, Fasano A (January 2018). "The overlap between Essential tremor and Parkinson disease". Parkinsonism & Related Disorders. 46 (Suppl 1): S101–S104. doi:10.1016/j.parkreldis.2017.07.006. PMID 28729090.
- ^ Finger EC (April 2016). "Frontotemporal Dementias". Continuum (Review). 22 (2 Dementia): 464–89. doi:10.1212/CON.0000000000000300. PMC 5390934. PMID 27042904.
- ^ McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor JP, Weintraub D, et al. (July 2017). "Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium". Neurology (Review). 89 (1): 88–100. doi:10.1212/WNL.0000000000004058. PMC 5496518. PMID 28592453.
- ^ Maltête D, Guyant-Maréchal L, Mihout B, Hannequin D (March 2006). "Movement disorders and Creutzfeldt-Jakob disease: a review". Parkinsonism & Related Disorders. 12 (2): 65–71. doi:10.1016/j.parkreldis.2005.10.004. PMID 16364674.
- ^ Tse W, Cersosimo MG, Gracies JM, Morgello S, Olanow CW, Koller W (August 2004). "Movement disorders and AIDS: a review". Parkinsonism & Related Disorders. 10 (6): 323–34. doi:10.1016/j.parkreldis.2004.03.001. PMID 15261874.
- ^ Pezzoli G, Cereda E (May 2013). "Exposure to pesticides or solvents and risk of Parkinson disease". Neurology (Meta-analysis). 80 (22): 2035–41. doi:10.1212/WNL.0b013e318294b3c8. PMID 23713084. S2CID 13628268.
- ^ a b Guilarte TR, Gonzales KK (August 2015). "Manganese-Induced Parkinsonism Is Not Idiopathic Parkinson's Disease: Environmental and Genetic Evidence". Toxicological Sciences (Review). 146 (2): 204–12. doi:10.1093/toxsci/kfv099. PMC 4607750. PMID 26220508.
- ^ a b Kwakye GF, Paoliello MM, Mukhopadhyay S, Bowman AB, Aschner M (July 2015). "Manganese-Induced Parkinsonism and Parkinson's Disease: Shared and Distinguishable Features". International Journal of Environmental Research and Public Health (Review). 12 (7): 7519–40. doi:10.3390/ijerph120707519. PMC 4515672. PMID 26154659.
- ^ Peres TV, Schettinger MR, Chen P, Carvalho F, Avila DS, Bowman AB, et al. (November 2016). "Manganese-induced neurotoxicity: a review of its behavioral consequences and neuroprotective strategies". BMC Pharmacology & Toxicology (Review). 17 (1): 57. doi:10.1186/s40360-016-0099-0. PMC 5097420. PMID 27814772.
- ^ McKnight S, Hack N (November 2020). "Toxin-Induced Parkinsonism". Neurol Clin (Review). 38 (4): 853–865. doi:10.1016/j.ncl.2020.08.003. PMID 33040865. S2CID 222299758.
- ^ Carod-Artal FJ (2003). "[Neurological syndromes linked with the intake of plants and fungi containing a toxic component (I). Neurotoxic syndromes caused by the ingestion of plants, seeds and fruits]". Revista de Neurología (Review) (in Spanish). 36 (9): 860–71. PMID 12717675.
- ^ Kim EA, Kang SK (December 2010). "Occupational neurological disorders in Korea". Journal of Korean Medical Science (Review). 25 (Suppl): S26-35. doi:10.3346/jkms.2010.25.S.S26. PMC 3023358. PMID 21258587.
- ^ Watanabe Y, Himeda T, Araki T (January 2005). "Mechanisms of MPTP toxicity and their implications for therapy of Parkinson's disease" (PDF). Medical Science Monitor. 11 (1): RA17-23. PMID 15614202.
- ^ Nandipati S, Litvan I (September 2016). "Environmental Exposures and Parkinson's Disease". International Journal of Environmental Research and Public Health (Review). 13 (9): 881. doi:10.3390/ijerph13090881. PMC 5036714. PMID 27598189.
- ^ Weiss J. Chapter 151. Toluene and Xylene. In: Olson KR, ed. Poisoning & Drug Overdose. 6th ed. New York: McGraw-Hill; 2012. http://www.accessmedicine.com/content.aspx?aID=55982958. Accessed April 21, 2013.
- ^ Uitti RJ, Snow BJ, Shinotoh H, Vingerhoets FJ, Hayward M, Hashimoto S, et al. (May 1994). "Parkinsonism induced by solvent abuse". Annals of Neurology. 35 (5): 616–9. doi:10.1002/ana.410350516. PMID 8179306. S2CID 23657208.
- ^ Lai J, Heran MK, Stoessl AJ, Gooderham PA (2017-03-27). "Reversible Parkinsonism and Rapidly Progressive Dementia Due to Dural Arteriovenous Fistula: Case Series and Literature Review". Movement Disorders Clinical Practice. 4 (4): 607–611. doi:10.1002/mdc3.12480. ISSN 2330-1619. PMC 6174482. PMID 30363443.
- ^ Matsuda S, Waragai M, Shinotoh H, Takahashi N, Takagi K, Hattori T (1999-05-01). "Intracranial dural arteriovenous fistula (DAVF) presenting progressive dementia and parkinsonism". Journal of the Neurological Sciences. 165 (1): 43–47. doi:10.1016/s0022-510x(99)00075-1. ISSN 0022-510X. PMID 10426146. S2CID 31594108.
- ^ Kim HR, Lee JY, Kim YK, Park H, Kim HJ, Son YJ, et al. (September 2015). "Dural Arteriovenous Fistula-Associated Reversible Parkinsonism with Presynaptic Dopaminergic Loss". Journal of Movement Disorders. 8 (3): 141–143. doi:10.14802/jmd.15021. ISSN 2005-940X. PMC 4572665. PMID 26413242.
- ^ Goldstein S, Friedman JH, Innis R, Seibyl J, Marek K (March 2001). "Hemi-parkinsonism due to a midbrain arteriovenous malformation: dopamine transporter imaging". Movement Disorders. 16 (2): 350–353. doi:10.1002/mds.1047. ISSN 0885-3185. PMID 11295793. S2CID 22701874.
- ^ Armenteros PR, Kapetanovic S, Lopez SG, Vazquez-Lorenzo E, Mendez LA, Muga JJ, et al. (2022-03-29). "Pearls & Oy-sters: Arteriovenous Malformation With Sinus Thrombosis and Thalamic Hemorrhage: Unusual Cause of Parkinsonism and Dementia". Neurology. 98 (13): 550–553. doi:10.1212/WNL.0000000000200016. ISSN 0028-3878. PMID 35121672. S2CID 246556634.
- ^ Jubault T, Brambati SM, Degroot C, Kullmann B, Strafella AP, Lafontaine AL, et al. (December 2009). Gendelman HE (ed.). "Regional brain stem atrophy in idiopathic Parkinson's disease detected by anatomical MRI". PLOS ONE. 4 (12): e8247. Bibcode:2009PLoSO...4.8247J. doi:10.1371/journal.pone.0008247. PMC 2784293. PMID 20011063.
- ^ Kuoppamäki M, Rothwell JC, Brown RG, Quinn N, Bhatia KP, Jahanshahi M (April 2005). "Parkinsonism following bilateral lesions of the globus pallidus: performance on a variety of motor tasks shows similarities with Parkinson's disease". Journal of Neurology, Neurosurgery, and Psychiatry. 76 (4): 482–90. doi:10.1136/jnnp.2003.020800. PMC 1739601. PMID 15774432.
- ^ Halliday GM (2009-12-15). "Thalamic changes in Parkinson's disease". Parkinsonism & Related Disorders. 15: S152–S155. doi:10.1016/S1353-8020(09)70804-1. PMID 20082979.
- ^ Apartis E, Tison F, Arné P, Jedynak CP, Vidailhet M (November 2001). "Fast orthostatic tremor in Parkinson's disease mimicking primary orthostatic tremor". Movement Disorders. 16 (6): 1133–6. doi:10.1002/mds.1218. PMID 11748748. S2CID 36301428.
- ^ Panzer J, Dalmau J (August 2011). "Movement disorders in paraneoplastic and autoimmune disease". Current Opinion in Neurology. 24 (4): 346–53. doi:10.1097/WCO.0b013e328347b307. PMC 3705177. PMID 21577108.
- ^ Liu Y, Lu Y, Zhang X, Xie S, Wang T, Wu T, et al. (November 2016). "A case of rapid-onset dystonia-parkinsonism accompanied by pyramidal tract impairment". BMC Neurology. 16 (1): 218. doi:10.1186/s12883-016-0743-8. PMC 5105251. PMID 27835968.
- ^ Saito M, Maruyama M, Ikeuchi K, Kondo H, Ishikawa A, Yuasa T, et al. (September 2000). "Autosomal recessive juvenile parkinsonism". Brain & Development. 22 (Suppl 1): S115-7. doi:10.1016/s0387-7604(00)00137-6. PMID 10984671. S2CID 22733500.
- ^ Del Toro-Pérez C, Guevara-Sánchez E, Martínez-Sánchez P (March 2023). "Treatment of Vascular Parkinsonism: A Systematic Review". Brain Sci. 13 (3): 489. doi:10.3390/brainsci13030489. PMC 10046744. PMID 36979299.
- ^ Shin HW, Hong SW, Youn YC (May 2022). "Clinical Aspects of the Differential Diagnosis of Parkinson's Disease and Parkinsonism". J Clin Neurol. 18 (3): 259–270. doi:10.3988/jcn.2022.18.3.259. PMC 9163948. PMID 35589315.
- ^ a b Martí-Massó JF, Poza JJ (1 May 1998). Stoessl AJ, Klein C, Standaert DG (eds.). "Cinnarizine-induced parkinsonism: ten years later". Movement Disorders. 13 (3). Vancouver, British Columbia, Canada: International Parkinson and Movement Disorder Society/Wiley: 453–456. doi:10.1002/mds.870130313. ISSN 1531-8257. PMID 9613736. S2CID 31516105.
- ^ "Information Sheet: Drug-induced Parkinsonism" (PDF). Parkinson's Disease and Society. Archived from the original (PDF) on 2013-06-26. Retrieved 2013-04-15.
- ^ Shuaib UA, Rajput AH, Robinson CA, Rajput A (March 2016). "Neuroleptic-induced Parkinsonism: Clinicopathological study". Movement Disorders. 31 (3): 360–5. doi:10.1002/mds.26467. PMC 5064745. PMID 26660063.
- ^ Louis ED, Ottman R (November 2013). "Is there a one-way street from essential tremor to Parkinson's disease? Possible biological ramifications". European Journal of Neurology (Review). 20 (11): 1440–4. doi:10.1111/ene.12256. PMC 3801177. PMID 24033795.
- ^ Fabrizi, Monaco, Dalla Libera (2004). "Parkinsonian syndrome following MDMA (Ecstasy) addiction". Movement Disorders. 19: S73–S74.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ "VA adds three new Agent Orange presumptions". U. S. Department of Veteran Affairs. September 10, 2021. Retrieved March 2, 2022.
