mastitis
| Classification according to ICD-10 | |
|---|---|
| N61 | Inflammatory diseases of the breast (mammary gland) |
| O91 | Infections of the breast (mammary gland) related to gestation |
| P39.0 | Infectious mastitis in the newborn |
| P83.4 | Non-infectious mastitis in the newborn |
| ICD-10 online (WHO version 2019) | |
The mastitis (syn. Mastadenitis ) or mastitis is usually a bacterial infection of the female, rarely the male mammary gland and mammary gland (from the Greek. Mastos ). Breast inflammation is usually found in breastfeeding mothers ( puerperal mastitis ), often around the second week after birth . Mastitis outside the puerperium is rare (so-called mastitis non puerperalis ). In the case of mastitis, immediate medical help is required so that the cause of the inflammation can be determined and, if necessary, a further development into a mature abscess can be avoided. In the case of mastitis outside the puerperium, it is also important to rule out a malignancy .
Symptoms
- fever
- Pain, usually unilateral (70%) in the nipple area
- Overheating of a chest
- Redness of a breast
- with abscess formation, fluctuating and palpable swelling (breast gland swelling)
- Swelling of the armpit lymph nodes
- altered milk secretion
- Increase in the number of cells in milk
pathology
In bacterial mastitis, a phlegmonous or abscessed inflammation can be found histologically with diffuse granulocytic infiltrates of the mammary gland tissue. In the case of prolonged chronic inflammation, a lymphoplasmic cellular infiltrate predominates . The inflammation usually spreads via lymphatic vessels ( interstitial mastitis ), less often via the milk ducts (intra-canalicular, so-called parenchymatous mastitis ).
A tuberculous mastitis shows typical caseating granulomas .
Puerperal mastitis
Only during the lactation period (breastfeeding period).
etiology
The entry points of pathogens in mastitis in breastfeeding mothers are usually small skin injuries (so-called rhagades ) of the nipple with secondary infection of these injuries by typical skin germs . In addition, an accumulation of secretion (due to a blocked milk duct ( ductus lactifer ) ) is made jointly responsible for the infection .
Pathogen
Typically skin and mouth germs are found in humans:
- Staphylococcus aureus (90%)
- Streptococci
- Pseudomonas et al. a.
therapy
According to the current study situation , weaning , supported by prolactin inhibitors ( dopamine agonists , e.g. bromocriptine ) is only necessary in exceptional cases and, as a rule, tends to delay the course of the disease. Conservative therapy with antibiotics is indicated (e.g. oxacillin). A risk of infection for the breast-fed child is not to be assumed. According to the current state of research, the symptoms subside more effectively with antibiotics than with pure bed rest.
Mature abscesses usually need to be surgically incised and drained, or punctured and flushed with an antibiotic solution. Surgical splitting of the abscess with an incision and a counter-incision is usually performed. In some cases, an ultrasound- guided minimally invasive breast abscess drainage can be performed as an alternative .
Mastitis non puerperalis
etiology
The cause of this mastitis is assumed to be an accumulation of secretions with secondary infection by germs.
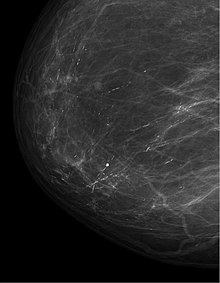
Differential diagnosis and further diagnosis
It is important that in the case of mastitis non puerperalis, a malignancy is excluded after the inflammation has healed ( breast cancer , Paget's cancer , inflammatory breast cancer).
Predisposing factors
- Hyperprolactinemia
- Tranquilizer intake
- Ovulation inhibitor intake
- Mastopathy
- Thyroid disorders
- Nicotine abuse
Pathogen
The following pathogens are found in bacterial mastitis:
- Staphylococci
- Streptococci
- Pseudomonas
- Proteus
- E. coli
- other, rather rare pathogens ( tuberculosis pathogens, anaerobes, etc.)
therapy
The therapy is basically the same as for puerperal mastitis. If an abscess has already formed, it is treated surgically, otherwise the necessary drug therapy is carried out.
For the drug therapy of nonpuerperal mastitis, prolactin inhibitors (such as bromocriptine ), antibiotics and anti-inflammatories can be used.
In addition to the drug treatment of mastitis, the chest must be cooled and a well-fitting bra must be worn.
Nonpuperal mastitis can become chronic.
Periductal mastitis
etiology
Periductal mastitis, also known as plasma cellular or granulomatous mastitis , is an abacterial and chronic mastitis that is triggered by secretion . The secretion behavior leads to ectasia of the milk ducts with the secretion passing into the surrounding tissue with the resulting inflammatory reaction . Middle-aged women are particularly affected. It is important to rule out a malignancy .
Symptoms
There is usually a painful induration in the nipple area with discharge.
pathology
The histology shows lymphoplasmacellular infiltrates and duct ectasia of the milk ducts. There are also granulomas , fat-storing macrophages (so-called lipophages ), epitheloid and giant cells .
Individual evidence
- ↑ S3 guideline: Treatment of inflammatory breast diseases during breastfeeding ( memento of the original from February 26, 2015 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. . P. 31.
- ↑ S. Jahanfar, CJ Ng, CL Teng: Antibiotics for mastitis in breastfeeding women. In: Cochrane Database of Systematic Reviews. 2013, Issue 2. Art. No .: CD005458. doi: 10.1002 / 14651858.CD005458.pub3 Summary (in English).
- ^ A. Strauss, L. Sanders: Minimally Invasive Breast Abscess Treatment: A Paradigm Shift. (PDF; 982 kB) In: Speculum 28th year, 3/2010. Retrieved October 12, 2014 .
- ↑ M. Fahrni, EI Schwarz, S. Stadlemann, G. Singer, M. Hohl, R. Kubik: Ultrasound-guided minimally invasive therapy of breast abscesses. In: Senologie - Journal for Mammadiagnostik und -therapie. Vol. 5, No. 3, 2008, pp. 1611-6453, doi: 10.1055 / s-0028-1095992 .
- ↑ Bradford G. Scott, Eric J. Silberfein, Huang Q. Pham, Mark A. Feanny, Brian K. Lassinger, Francis J. Welsh, Mathew M. Carrick: Rate of malignancies in breast abscesses and argument for ultrasound drainage. In: The American Journal of Surgery . 192, 2006, pp. 869-872, doi: 10.1016 / j.amjsurg.2006.08.060 .
- ↑ A. Strauss, K. Middendorf, S. Müller-Egloff, IM Heer, M. Untch, I. Bauerfeind: Sonographically guided percutaneous needle aspiration of breast abscesses - a minimally invasive alternative to surgical incision. In: Ultrasound in Medicine (Stuttgart, Germany: 1980). Volume 24, Number 6, December 2003, pp. 393-398, ISSN 0172-4614 . doi: 10.1055 / s-2003-45217 . PMID 14658082 .
- ^ A b Xaver Skibbe, Andrea Löseke: Gynecology and obstetrics for nursing professions. Georg Thieme Verlag, 2013, ISBN 978-3-13-152553-6 , p. 138.
- ↑ mastitis. In: onmeda. Retrieved October 11, 2014 .