Osteochondrosis dissecans
| Classification according to ICD-10 | |
|---|---|
| M93.2 | Osteochondrosis dissecans |
| ICD-10 online (WHO version 2019) | |

The osteochondritis dissecans (short OCD or OD , Anglo-American also osteochondritis dissecans ) is a localized bone lesion below the articular cartilage associated with the rejection of the affected bone area with the overlying cartilage as loose bodies ( joint mouse can end). A joint surface defect (mouse bed) then remains. OCD can affect most joints in the human body, but it mainly occurs in the knee , upper ankle, and elbow joints . Due to concentrated mechanical action, however, the OD occurs almost exclusively in convex parts of the joint such as the femoral condyle , the talus roll , the radial condyle of the humerus and on the femoral head . This article is mainly based on the knee localization. In veterinary medicine , it occurs particularly in large breeds of dogs (shoulder, elbow, knee, ankle, etc.) and in fattening pigs .
Etiology (cause)
Mechanical factors (repetitive impulse loads) seem to be the most likely main cause of various theories of origin that have been controversially discussed in the past. Therefore, active to highly active children and adolescents are most often affected. Without intensive sporting activities, osteochondrotic changes in the knee do not occur. This also applies to Osgood-Schlatter disease . Possibly in the (typical) OCD on the medial femoral condyle a disturbance of the movement sequence during running and jumping plays a decisive role. Quite often, patients with OD on the knee can be asked about long and intensive use of the trampoline . This sporty peculiarity is not surprising: It is a highly stressed repetitive strain. In the rarer osteochondrosis dissecans of the lateral femoral condyle, meniscus pathology (e.g. a disc meniscus ) and possibly childhood rheumatism also play a role. The also common OCD of the medial talus shoulder in the upper ankle joint may be a real OCD with repetitive overload caused by exercise. The cartilage bone lesion of the lateral (outer) talus shoulder is exclusively the result of repeated ankle injuries, i.e. traumatic osteochondral flakes, cartilage bone scales with a completely different therapeutic approach. In the case of OCD on the elbow , throwing sports that put a strain on the arm ( handball , volleyball ) are often causally involved. However, the mechanical genesis of all OCD forms on the elbow cannot be documented as clearly as on the knee. The role of bone structure and quality in the development of OCD is the subject of further studies in osteology . Almost all those affected have an insufficient supply or a partially pronounced vitamin D3 deficiency with corresponding disorders of the calcium metabolism. The bone structure disorder associated with vitamin D3 deficiency can contribute to the picture of OCD with a typical fracture healing disorder ( pseudarthrosis ). It is not, as long assumed, osteonecrosis, the bone is not dead (necrotic), but only structurally changed. The part of the joint (mouse) affected by the OCD cannot heal due to the repetitive mechanical stress, but gradually loosens. Vitamin D3 deficiency plays a decisive role in this healing disorder.
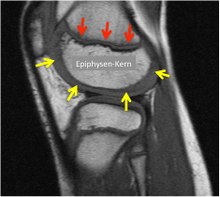
According to current investigations from veterinary medicine, circulatory disorders of the epiphyseal growth plate play a central role in causing the disease OCD: It is of great importance to understand that the cartilaginous growth plate (red) is not only important for length growth in the thigh shaft, but also as a closed layer on the bony epiphyseal nucleus for the growth in thickness of the femoral condyles (Fig. yellow arrows). The vascular-free articular cartilage lies on this cartilaginous epiphyseal growth plate. The growth plate is supplied with blood from the bone side (the epiphyseal nucleus) and the vessels are at risk from mechanical impacts (shear loads). Studies in foals and piglets show that cartilage necrosis occurs in the growth zone under the joint cartilage. These necrosis zones, like the surrounding growth cartilage, reach the epiphyseal bone zone in the course of normal growth and are marked there as a bony osteochondrosis zone. This means that for the first time they are visible with low contrast in the X-ray image. Only some time (months to years) after the onset of cartilage necrosis and the development of a bony OCD focus does the typical stress-dependent pain appear, which in turn enables the diagnosis to be made.
Pathogenesis (course of disease)
The disease may arise from a bony structural disorder below the articular cartilage (subchondral vascularization disorder). This takes place in the border area between articular cartilage and growth cartilage around the epiphyseal nucleus. (Lit. Olstad et al.) At the beginning there is chondronecrosis in this area, later on to a connective tissue demarcation (rejection) from the vital surrounding bone. Then a healing disorder in the sense of a pseudarthrosis seems to be the decisive process. The once dissolved dissecate does not heal again under the mechanical stress. The overlying the Osteochondroseherd articular cartilage shows no changes initially, it is vital and mechanically stable because its (normal) diet by synovial fluid synovial ensures unchanged. Later, due to the increasingly unstable bony base and an increase in volume due to loose, water-rich tissue in the border area between the dissecate and the bearing bone, secondary cartilage changes in the form of overstretching and tears at the edges of the affected zone occur. These changes in contour (bulging or bulging) of the effective joint surface can now lead to joint blockages for the first time due to trapping ( impingement ). Continuous stress then results in a loosening of the cartilage-bearing bone from the vital environment and, after a rupture of the elastic cartilage cover in the late phase, the entire piece of cartilage-bone dissolves and thus the joint mouse ( dissecat ). The dissecate may vary depending on joint circuit remain in the mouse long bed (often at the anklebone (talus) and at the head of the femur) or acute deploy (often on the femoral condyle ), d. H. moved from the mouse bed to other parts of the joint cavity by moving the joint. This stage of dissection gives the disease its name (dissecans): In the past, before the introduction of X-ray and nuclear spin examinations, the disease was only recognized when the "mouse" was detached and the resulting blockage. In the last stage of the disease (dissection), the cartilage-bone fragment can also break down and disintegrate into hardly detectable parts. In any case, a relevant articular surface defect (mouse bed) corresponding to the size of the mouse remains after the dissection.
Clinic (complaints)
The first symptoms appear in children and adolescents from around the age of 8 to around 15 years as unspecific, load-dependent pain at the affected joint. These are often misinterpreted by doctors, parents and trainers as the consequences of injuries, growing pains or rheumatism. The time from the first symptoms to the definitive diagnosis is still around a year. Morning complaints never occur, they only occur during and / or after exercise. Typically, the sport often has to be stopped due to the pain (the children sit on the bench after half time). Consistent sports breaks or relief will reduce the symptoms. A joint effusion (thick knee) or a soft tissue swelling (doughy swelling) is not one of the signs of OCD, it is initially not a joint disease, but a disease of the bone core of the femoral condyle. The pain point cannot be precisely localized either, i.e. pointed at it with a finger. The pain is indicated rather dull and pulling deep in the bone. After a joint mouse has been detached , OD is a joint disease. The dissection of the joint surface can pinch and it comes to the joint lock (blockage) and sudden onset of severe pain like a large meniscus tear . Mechanical symptoms (blockages, inhibition of stretching) in addition to pain are always a warning signal and an indication of an already existing change in the articular surface, instability or an incipient dissection (rejection) of the cartilage-bone fragment. In rare cases there are pronounced OD findings without any symptoms. An accumulation of this particular painless course can be found in cortisone therapy z. B. for bronchial asthma or as part of chemotherapy in children z. B. because of an ALL .
diagnosis
The disease can be discovered by chance on an X-ray that is taken after an accident of the knee region , the ankle or the elbow . In the case of typical complaints of active children and adolescents, a clear diagnosis can be made with such a simple X-ray, because the changed bone below the joint surface can be identified at a typical location in the thigh roll on the knee. Sometimes a so-called tunnel image with a bent knee can show the damaged area even better. Magnetic resonance imaging (MRI) should be performed for a more detailed analysis . The position and size of the finding, the depth and, above all, the involvement of the overlying cartilage can be precisely measured on the images generated. Statements about the stability of the finding are also to be made. This then results in decisive clues for therapeutic consequences. MRI is best for assessing the progression of the disease, but a simple X-ray examination may also be used. Due to the high cost of MR in the USA, the courses there are largely only documented with X-rays, which leads to our own recommendations for course assessment. In general, however, MR examinations are the method of choice. They allow a differentiated assessment of the different criteria for healing, instability and impending dissection. Examinations with sonography can provide reliable, but only indicative findings on the femoral condyle. It is thus possible, for example, to rule out the infestation on the opposite side more quickly, cheaply and reliably.

therapy
General
The therapy of osteochondrosis dissecans on the knee joint is initially dependent on the relative size of the lesion compared to the condyle. There is OCD on the medial and on the lateral thigh roller (condyle). The change also rarely occurs on the sliding bearing opposite the kneecap and on the kneecap itself. Another important decision criterion is the stage (stable / unstable) of the lesion. Cyst formation, a protrusion of the cartilage-bone dissection, a fracture of the subchondral bone lamella and the formation of cracks in the cartilage are clearly evident on the MRI as signs of instability . An important clinical symptom of instability of the OD focus is a blockage in the joint function, which occurs as a sign of the involvement of the articular surface in the disease process. In addition, the age of the patient plays a certain role. If the growth plates are still wide open - that is, boys up to 14 years of age and girls up to 13 years of age - the spontaneous healing chances are better. On average, in all studies, 50% of OCD cases of the knee joint heal without surgical measures. Healing always takes months to years because the necessary bone remodeling by osteoclasts and osteoblasts takes a long time. For this, bony structures have to be dissolved, removed and rebuilt.
Conservative therapy
First, except in the case of dissected or dissection-prone (unstable) findings and findings with relevant cyst formation, a conservative attempt without surgery should be made for at least 3–6 months. For this purpose, the mechanical stress on the joint in question is massively reduced through a strict sports ban. Good cooperation between doctor, parents and patient plays a decisive role here (triad). In the case of persistent complaints, it may also be necessary to use forearm crutches for lesions on the knee or ankle until the pain has subsided. Immobilization of joints, e.g. B. in a plaster cast or relief with z. B. a Thomas splint , are no longer used in current treatment concepts.
Regardless of the surgical aspects of the therapy, treatment of any vitamin D3 deficiency is indicated. It is safest to conduct a laboratory test of the calcium metabolism . Regardless of this, the German Nutrition Society has been recommending a basic supply of 800E per day for everyone in Germany from the 1st year of life for a few years. As therapy for existing osteochondrosis dissecans, at least 2000 U must be administered per day. Alternatively, 20,000 E per week can be set more simply according to the osteological recommendation. This basic measure is also indicated for surgical therapy.
Operative therapy
If the knee or ankle complaints persist or increase despite a consequent sports break, especially if mechanical symptoms such as blockages or joint snapping and if there is an increase in size or indications of instability in the MRI, an arthroscopy of the joint concerned is recommended in order to be able to assess the condition of the articular cartilage, which cannot be reliably achieved with magnetic resonance imaging. Hard criteria for an operation are a large focus, cyst formations over 2.3 mm and signs of instability in the MR.
If the cartilage is intact in the arthroscopic diagnosis and no delimitation of the affected area can be seen on the joint side, a retrograde (from outside the joint) or anterograde (from the joint surface and through the cartilage) drilling of the damaged zone is indicated to revitalize the bone. For retrograde drilling, special cannulated drills are used, in which the correct position in the fluoroscopic x-ray is first checked with a guide wire and then overdrilled definitely. Vessels , growth factors and stem cells can penetrate through the drill holes into the changed bony area and thus allow the OD scale to heal again with the surrounding bone.
If the affected area has not yet been detached, but an incipient demarcation can be identified, a retrograde spongiosaplasty can be performed through a drill channel or an open bone transplant and drilling can be carried out using the detached findings (cartilage-bone cover) . This procedure is particularly useful for stubborn findings on the talus, which rarely heal spontaneously.
In the case of a loosened or loosened unstable dissecate, refixing (reattaching) the dissecate is always indicated in adolescent patients in addition to drilling into the surrounding bone. The healing rate is very good here. Resorbable pins are preferably used for this, after mini-screws made of titanium were previously used. However, these had to be removed again by surgery after healing. The dissolved dissecate and the “mouse bed” must be freshened up and possible substance defects filled with autologous cancellous bone . If the dissecate is destroyed or dead, a bone-cartilage transplant is usually the treatment of choice for adults . In contrast to pure drilling, these operations are carried out openly via a joint opening ( arthrotomy ). The advantage of cartilage-bone transplantation is that it can also be used for deep bony lesions, such as those often found in OCD. However, removal defects occur here. For the appropriate technique, see the section on osteochondral transplant
Newer methods of cartilage cell transplantation use the transplantation of the body's own (autologous) cartilage cells grown in the laboratory into the cartilage defects under a protective layer of the body's own periosteum or of collagen matrix fleece as autologous chondrocyte transplantation (ACT) or in matrix substances as matrix-associated chondrocytes (MACI). The cell-free implantation of collagen matrix in the bone prepared defect site as AMIC (autogenous matrix-induced chondrogenesis) has meanwhile also been successful . The avoidance of time-consuming and costly cell cultivation with known only incomplete complete differentiation into cartilage cells is advantageous here. In deep bony necrosis zones, however, these cartilage regeneration procedures alone are not suitable. In addition, an autologous (body's own) cancellous bone transplantation must be performed under the cartilage layer.
Furthermore, some groups try to revitalize the dissecat with extracorporeal shock wave therapy, provided that it has not yet split off as a joint mouse. Other groups are trying hyperbaric oxygen therapy . There is no scientific evidence or individual reports for the success of either approach.
Results
The younger the patient, the better the healing prognosis. Patients who have closed the growth plates (15–17 years of age depending on gender) have a significantly poorer chance of healing without surgery. The aim of treatment is to fully restore the structure and function of the affected joint. This requires healing and restructuring (remodeling) of the changed bone areas. Since bones can generally heal and remodel completely without scars and in a physiological structure, no residual anatomical or mechanical damage is to be expected as long as the cartilaginous joint surface is not affected. Smaller and stable findings in adolescents can spontaneously regress or heal within one year at the earliest if there is a consistent break in exercise. In the case of larger, also stable, non-dissected findings, despite surgical measures (drilling), healing can take several years. If conservative therapy has stopped, an operation should be planned. The criteria for the assessment can only be found reliably in the MR. After such findings have healed, the results can usually be described as very good and good. Once an OD has healed, it never occurs again. The reason for this is that it originated years ago as a circulatory disorder of the growth cartilage, which at the time of healing had already completely passed into the bone.
Unstable diseases in which an osteochondral dissection has partially or completely fallen out of the joint, the aim is to anatomically fit the joint part into the "mouse bed" and to ensure that it is stable. The mouse bed and the dissecat are first freed of all loose tissue with sharp instruments until the bony base is reached. Then drill deep into the healthy bone from the contact area in order to enable vessels and stem cells to grow in here as well. Then the bone defect created by the removal of the loose tissue is filled with a bone graft . The dissectic scale is then fixed in a mechanically stable manner with several resorbable polymer pins. With the best technology, good and in some cases very good results can be achieved here.
Installation and remodeling processes take a long time (years) in the bone. The resilience of such an affected and operated joint is significantly limited for many months.
Good results can also be achieved in the case of dissected osteochondrosis with loss or disintegration of the dissecate if an osteochondral transplant is carried out from a cartilage-bone cylinder from a joint area that is not under stress into the defect area. The notch entrance (edge of the zone between the femoral condyles, which is occupied by the cruciate ligaments) and the rear (dorsal) condyle are ideal here . Only autologous cartilage cell transplants cannot compensate for the bony defect and are therefore not suitable for profound damage to the joint surfaces. The results of cell transplants can therefore only be compared to osteochondral transplantation in connection with simultaneous bone transplantation or through the use of synthetic matrix substances.
literature
- M. Krause, D. Lehmann, M. Amling, T. Rolvien, KH. Frosch, K. Püschel, K. Bohndorf, NM Meenen: Intact Bone Vitality and Increased Accumulation of Nonmineralized Bone Matrix in Biopsy Specimens of Juvenile Osteochondritis Dissecans: A Histological Analysis . In: Am J Sports Med 2015 43, 6: 1337 . 2015 (English).
- M. Krause, A. Hapfelmeier, M. Möller, M. Amling, K. Bohndorf, NM Meenen: Healing Predictors of Stable Juvenile Osteochondritis Dissecans Knee Lesions After 6 and 12 Months of Nonoperative Treatment. In: Am J Sports Med. 2013 Jul 22 . 2013, PMID 23876519 (English).
- Eric J. Wall, Jason Vourazeris, Gregory D. Myer, Kathleen H. Emery, Jon G. Divine, Todd G. Nick, Timothy E. Hewett: The Healing Potential of Stable Juvenile Osteochondritis Dissecans Knee Lesions . In: The Journal of Bone & Joint Surgery (American Edition) . tape 90 , no. 12 . JBJS, Needham, MA 2008, pp. 2655-2664 , PMID 19047711 (English).
- NM Meenen, B. Rischke: Autogenous osteochondral transplantation (AOT) for cartilage defects on the femoral condyle . In: Operative Orthopedics and Traumatology . tape 15 , 2003, p. 38-56 , doi : 10.1007 / s00064-003-1061-z .
- JP Petersen, A. Ruecker, D. von Stechow, P. Adamietz, R. Poertner, JM Rueger, NM Meenen: Present and future therapies of articular cartilage defects . In: European Journal of Trauma . tape 29 , no. 1 , 2003, p. 1-10 , doi : 10.1007 / s00068-003-1215-6 .
- K. Baumbach, JP Petersen, P. Ueblacker, J. Schröder, C. Göpfert, A. Stork, JM Rueger. M. Amling, NM Meenen: The fate of osteochondral grafts after autologous osteochondral transplantation: a one-year follow-up study in a minipig model . In: Arch Orthop Trauma Surg . tape 128 , no. 11 , 2008, p. 1255-1263 , PMID 18064477 (English).
- K. Olstad, B. Ytrehus, S. Ekman, CS Carlson, NI Dolvik: Early Lesions of Articular Osteochondrosis in the Distal Femur of Foals . In: Vet Pathol . tape 48 . Sagepub, 2011, p. 1165–1175 , doi : 10.1177 / 0300985811398250 (English).
- K. Olstad, KG Shea, PC Cannamela, JD Polousky, S Ekman, B Ytreus, CS Carlson: Juvenile osteochondritis dissecans of the knee is a result of failure of the blood supply to growth cartilage and osteochondrosis . In: Osteoarthritis Cartilage . tape 26 . WB Saunders, London, 2018, pp. 1691–1698 , doi : 10.1016 / j.joca.2018.06.019.Epub2018Sep21 (English).
- Jungeblut, OD, Berger-Groch, J, Meenen, NM, Stuecker, R, Rupprecht, M .: Validity of Ultrasound Compared with Magnetic Resonance Imaging in Evaluation of Osteochondritis Dissecans of the Distal Femur in Children . In: Cartilage . Febr. Sagepub, 2019, p. epub ahead of print , doi : 10.1177 / 1947603519828434 (English).
Individual evidence
- ↑ Identification of Areas of Epiphyseal Cartilage Necrosis at Predilection Sites of Juvenile Osteochondritis Dissecans in Pediatric Cadavers 2018 F Toth, MA Tompkins, KG. Shea, JM. Ellermann CS. Carlson J Bone Joint Surg Am. 100: 2132-9 PMID 30562294
- ↑ Juvenile osteochondritis dissecans of the knee is a result of failure of the blood supply to growth cartilage and osteochondrosis Olstad K, et al. 2018 Osteoarthritis and Cartilage 26: 1691-1698 PMID 30248503
Web links
- The illustrations in the Commons do not correspond in every detail to current ideas about the disease, especially since it has been shown that it is not an osteonecrosis, but a healing disorder.


