Fracture of the radial head
The radial head fracture is a fracture in the upper end of the spoke . With 3% of all broken bones, the fracture of the radial head is relatively common and the most common fracture in the elbow area . The cause of this is usually a fall on the outstretched arm, often with a valgus thrust. In addition to simple fractures, complex fractures with accompanying injuries are described.
A special form is the radius neck break , in which the radius head is broken off as a whole and is intact. These are particularly common in children (see below).
Diagnosis
Often those affected report pain that pulls on the spoke side over the forearm to the hand. During the examination, however, there is usually a well localizable pain on the radial head, which can be aggravated by turning the forearm. The bruise in the joint or displaced bone fragments can limit mobility, particularly when straightening the elbow.
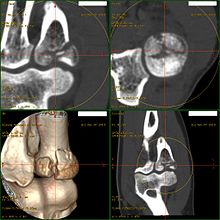
X-rays of the elbow confirm this . However, unshifted breaks in the standard exposures can easily be overlooked. The so-called fat pad sign, which indirectly indicates a joint effusion, is often helpful here . If the situation is unclear, two 45 ° oblique exposures, a computer tomography or a magnetic resonance tomography can also be performed. The latter are also suitable for showing accompanying bone fractures, for example in the adjacent part of the humerus (the humerus capitulum ) or the ulna near the elbow (the coronoid process ).
Accompanying injuries
Adjacent ligaments and bones are often affected, especially in the case of displaced, unstable, complex and fragmentary fractures. First and foremost, there are tears in the collateral ligaments of the elbow, especially the collateral ligament on the elbow (the ligamentum collaterale ulnare ), which, like the radial head, stabilizes the elbow against valgus forces. In addition, impression fractures of the humerus capitulum adjacent to the radius as part of the humerus and avulsion fractures of the coronoid process of the ulna can occur. If the olecranon ruptures at the same time, a simultaneous backward dislocation can occur, which is also known as a posterior Monteggia fracture . The interosseous membrane of the forearm can also tear , known as an Essex-Lopresti injury .
Scientific studies show that concomitant injuries occur more frequently than is generally assumed. Many of them are harmless, but even with simple fractures of the radial head, up to 11% of accompanying damage requiring treatment can occur.
Also, in elbow dislocations, there are often fractures of the radial head, which are often combined with breaks in the coronoid process of the ulna and both serve to stabilize the bony. In the event of dislocation and fracture of both bones with an additional ulnar ligament tear, there is severe instability, which Tscherne calls a terrible triad .
In high-speed and high-energy trauma, complex comminuted fractures are particularly common, together with a spoke fracture near the wrist ( distal radius fracture ), a scaphoid fracture or a fracture of the upper arm near the shoulder ( proximal humerus fracture ).
Nerve injuries are rare and almost always transient, i. H. Complete recovery occurs after a few days to weeks. Valgization during a fall can result in an injury to the ulnar nerve and, through direct contact with the bone fracture, an injury to the radial nerve , but also to the ulnar nerve and the posterior interosseus nerve .
Classification
The most common classification in addition to the AO classification , which, however, groups (proximal) fractures of the ulna and radius close to the elbow under a common category "21", is that according to Mason or one of the modifications:
- Type 1 : nondisplaced head fracture (sometimes also called nondisplaced chisel fracture ), most common form.
- Type 2 : displaced head fracture , also called chisel fracture . A type 2 is usually spoken of if there is a step formation of more than 2 mm or a fragment of> 30% of the joint surface. However, the delimitation is not uniform
- Type 3 : comminuted fracture
In the Bakalin classification, there are also two special forms:
- Type 4 : non-displaced radius neck fracture
- Type 5 : displaced radius neck fracture
No classification has been generally accepted so far, all classifications show a low reproducibility (low interobserver reliability ). A therapy decision cannot be derived with certainty either.
The vast majority of partial radial head fractures type 1 and 2 affect the anterolateral quadrant; in one study this was 22 of 24 fractures
Therapy indication
Most fractures of the radial head can be treated conservatively with good results.
Surgical therapy is often recommended, depending on concomitant diseases, age and life situation, if there is instability or a significant displacement of the bone fracture fragment (type 2) and especially if the forearm rotation is restricted. A significant shift usually occurs when the fracture fragment has sunk by more than 2 mm. If the fragment makes up more than 25% of the articular surface, there is an increased risk of later displacement and surgery is often recommended, as is the case with comminuted fractures (type 3).
However, there have been reports that even with large displaced fragments, the results of nonsurgical therapy are good if the forearm rotation is not restricted.
In the case of combined injuries, particularly with accompanying instability of the elbow joint, surgical stabilization is usually recommended, which includes the accompanying injuries, e.g. B. the suture of the inside (ulnar) collateral ligament.
Conservative therapy
In the case of severe pain and significant effusion in the elbow joint, a relieving joint puncture is often performed under local anesthesia, which is performed either through the tendon of the triceps brachii muscle above the tip of the olecranon or radially to the side of the olecranon in the so-called Hueter triangle .
If conservative therapy or delayed surgical therapy after swelling is chosen, the patient is usually immobilized in an upper arm plaster splint with the elbow held in a 90 ° flexion position. If the fractures are not or only slightly displaced, physiotherapeutic exercises can be started from the plaster splint after a few days, often after a week . After the elbow is swollen, prefabricated splints (elbow orthoses ) or a removable, individually made plastic plaster splint are often used . A splint is rarely necessary for more than three weeks, and early mobilization is particularly important to avoid permanent restriction of movement in the elbow joint ( contracture ), which can occur quickly, especially in the elbow joint. After six weeks, a largely free range of motion is usually achieved.
In the Anglo-American region, immobilization is often only carried out for five to seven days in a collar and cuff sling, in which the wrist is grasped and held around the neck with a sling when the elbow is bent.
Operative therapy
Open reduction and osteosynthesis Especially with displaced fragments (more than 2 mm displacement) that make up more than a third of the articular surface, open reduction is often indicated, especially when the forearm rotation is restricted. Reduction with osteosynthesis can also be carried out with more complex and unstable fractures. The aim is to achieve stable osteosynthesis with anatomical repositioning.
Small, preconfigured plates that are placed in the “safe” zone of the radial head that has no joint partner are ideal for osteosynthesis. However, the shape of the radius head is very variable, so that the plates often still have to be adjusted. Despite their now quite small dimensions, they are still bulky and can irritate the capsule and the ligamentous apparatus. Alternatively, individual small headless or countersunk screws (1.5 to 2.5 mm) can be used. This is particularly useful as a bouquet technique for displaced neck breaks.
In the case of impacted fractures, the fragments must first be separated, sometimes with small hooks or narrow K-wires . The bone defect can be filled with a spongiosaplasty , which can be obtained from the olecranon or the lateral humeral epicondyle .
The results of osteosynthesis are generally considered to be good, with poorer results for more than three fracture fragments. However, adhesions and restricted mobility can often occur. Also, a nonunion , osteonecrosis of the radial head or individual fracture fragments and postoperative osteoarthritis has to be possible, so be revised. It is possible that pure screw osteosynthesis is superior to plate osteosynthesis; studies indicate less rigidity and less metal removal.
Radial head resection This procedure is a surgical option, especially in the case of fractures, if reduction and stable osteosynthesis are not possible. Since the radial head stabilizes the elbow joint against a valgus position, such a misalignment as cubitus valgus can develop after a resection . Risk factors for this are a resection of more than 2 cm, hard physical work and accompanying injuries, especially instability of the ulnar collateral ligament ( lig. Collateral ulnare ). The muscular force exerted on the elbow normally exerts pressure on the radial head, which presses it against the capitulum. After a resection, the entire radius can be pushed forward instead, which is then reflected in the wrist as the relative excess length of a cubit. During the resection, the attachment of the biceps tendon must be retained for good function.
Radial head prosthesis For severe and complex fractures where osteosynthesis is not possible, or for complications after osteosynthesis, prosthetic replacement is a good indication. There are several variants, some monopolar and bipolar prostheses as well as modular prostheses, and cemented or uncemented prostheses. Exact placement is difficult; it can be excessively long or shortened. this can result in pain, instability and osteoarthritis. If it is too long, the increased contact pressure can also cause osteonecrosis of the capitellum. Other typical complications of prosthetic replacement are infection, dislocation and mechanical loosening. Loose seams in the radial shaft can be found on X-rays in up to 94%, but without any correlation to symptoms or functional restrictions. The medium-term results are good, long-term results are hardly available. the results may be better with a prosthetic fitting in the first ten days after the accident. If the ligament is injured at the same time, it seems that functional losses tend to occur.
Postoperative follow-up treatment Postoperative immobilization is usually only carried out for seven to ten days in an upper arm plaster splint or an orthosis. This is followed by passive exercises with a gradually increasing range of motion. Full extension should be avoided in the first four weeks, especially if the ligament is injured. From six weeks postoperatively, a largely normal range of motion should be achieved - but this is often problematic, since both conservative and surgical therapy often have permanent end-level restrictions on movement. Strengthening exercises can usually be started after eight to twelve weeks.
Complications
A nonunion is rare and can most likely occur with insufficient repositioned radial neck fractures. On the other hand, with conservative treatment, painful incorrect healing ( malunion ) with remaining deformity or step formation can occur more frequently , which in the medium term can result in post-traumatic arthrosis of the elbow joint and painful restriction of movement, especially in the forearm rotation. Then the surgical measures can be carried out secondarily, a corrective osteotomy of the radial head is also possible.
Immobilization can result in permanent restriction of movement of the elbow joint ( contracture ), which is particularly common at the elbow joint and can be caused by too long immobilization, but also by the fracture itself. First and foremost, there is a extension deficit and reduced Supinationsfähigkeit in the forearm. The causes are usually adhesions in the joint or shrinkage of the capsule, which can be treated surgically if physiotherapeutic and manual therapy is unsuccessful. Both an open arthrotomy and an arthroscopy can be performed; the results are usually very good.
Heterotopic ossifications are also common on the elbow (around 7%). Risk factors include severe instabilities, multiple surgical interventions, delayed surgical therapies and a long period of immobilization. Therapy with indomethacin or radiation does not differ from the general therapy of heterotopic ossifications in other locations, although the healing of the fracture can be delayed by radiation.
Inadequate stabilization of the ligamentous apparatus and further misalignment of the radial head can result in chronic valgus instability.
Due to the operation, depending on the access route, the ulnar nerve and the posterior interosseous nerve are particularly at risk of injury . However, most nerve injuries are temporary, permanent lesions are rare, and neurolysis is rarely necessary.
Childish fractures
1.3% of all broken bones in children are radius head fractures. They are almost always subcapital; H. localized on the radius neck. Three quarters of all radius head fractures are subcapital without involvement of the growth plate in the metaphysis , while a quarter are epiphyseal solutions with or without a metaphyseal wedge (i.e. Salter I or II). Epiphyseal fractures are very rare and only occur in adolescents shortly before the growth plate closes.
Since the epiphysis is supplied exclusively by the periosteal vessels of the radial neck, at least partial osteonecrosis of the radial head usually occurs, resulting in widening and possibly slight shortening of the epiphysis. This can limit the rotation of the forearm in the long term.
On the other hand, fractures in children have a high potential for spontaneous correction, so that in children under ten years of age, kinks in the frontal and sagittal planes of up to 50 ° can be tolerated, and from 10 years of age still 20 °. But lateral displacements of more than half the width of the shaft are not corrected on the radial head (unlike on other parts of the body) and must then be repositioned in a closed manner. This can be done especially with retrograde prévot nails (ESIN).
As a rule, conservative therapy with plaster of paris immobilization for 10-14 days can be carried out, with subsequent early mobilization to avoid stiffening. Physiotherapy is usually not required and can cause additional damage to the epiphysis. A closed reduction under anesthesia is recommended if the shaft is displaced by more than half the width of the shaft and tilted by more than 50 ° for children under 10 years of age and more than 20 ° for children aged ten and over.
The child's radial head fracture usually heals stably after two weeks and can be moved freely. Exercise can often be resumed after three weeks. Since movement is often only completely free again after a few months, some restrictions have to be accepted when doing sports.
Follow-up examinations up to two years after the accident are considered sufficient if there are no more axis deviations during this time and movement is free. Particularly on the ulnar side of the radial head, there can occasionally be a partial joint closure, which can lead to a valgus malalignment of the radial head. This can after complete joint lock by a subcapital osteotomy be corrected. If the radial head is greatly enlarged with the resulting restriction of movement, especially in the forearm rotation, a head resection can also be considered after the joint has closed (16-18 years of age).
A very rare but very difficult to treat complication is post-traumatic radioulnar synostosis with forearm rotation canceled.
A retrospective analysis of 151 children (8.4 years ± 2.9) displaced radius neck fractures from Boston showed a high rate of non-optimal results (31%), which were observed particularly in children over ten years of age and with a major deformity. A closed repositioning was not successful in 50% of all fractures with more than 64% deformity, some of them had to be repositioned secondarily. Immediate open reduction was recommended in Boston for all open fractures, fractures with neurovascular complications, and for malocclusions greater than 100%.
Individual evidence
- ↑ P. Vavken, J. Vavken, S. Demarmels, D. Rikli: Associated Injuries in Radial Head Fractures. In: Z Orthop accident. 155 (2), Apr 2017, pp. 220-225. Epub 2017 Apr 25. German. PMID 28444676
- ↑ Ryan M. Zimmerman, Leslie A. Kalish, Timothy Hresko, Peter M. Water, Donald S. Bae: Surgical Management of Pediatric Radial Neck Fractures. In: The Journal of Bone & Joint Surgery . Volume 95-A, Edition 20, 2013, October 16, 2013, pp. 1825–1832. doi: 10.2106 / JBJS.L.01130
literature
- M. Lapner, GJ King: Radial head fractures. In: The Journal of bone and joint surgery. American volume. Volume 95, Number 12, June 2013, pp. 1136-1143, ISSN 1535-1386 . PMID 23943926
- Bernhard Weigel: Radius head and radius neck fracture. In: Bernhard Weigel, Michael Nerlich: Praxisbuch Unfallchirurgie. Volume 1, Springer-Verlag, Berlin 2005, ISBN 3-540-41115-1 , pp. 337-340.
- Lutz von Laer: fractures of the proximal end of the radius. In: Lutz von Laer: fractures and dislocations in growing age. 3. Edition. Thieme-Verlag, Stuttgart 1996, ISBN 3-13-674303-2 , pp. 156-168.