Shwachman-Bodian-Diamond Syndrome
| Classification according to ICD-10 | |
|---|---|
| Q45.0 | Other congenital malformations of the digestive system |
| ICD-10 online (WHO version 2019) | |
The Shwachman-Diamond syndrome (SBDS) is a rare inherited disease characterized by a lack of formation of digestive enzymes in the pancreas ( exocrine pancreatic insufficiency ), disturbances of the function of the bone marrow with a tendency to the development of leukemia , skeletal abnormalities and short stature characterized . After cystic fibrosis , it is the second most common cause of exocrine pancreatic insufficiency in childhood.
Synonyms are: Shwachman syndrome; Shwachman-Bodian syndrome; Shwachman-Blackfan-Diamond-Oski-Khaw syndrome; Shwachman Diamond Syndrome
history
The disease was first recognized by Bodian and colleagues in 1964 and described by Shwachman and Diamond that same year. In 2001, a linkage analysis in several SBDS families showed that the gene locus sought must be on chromosome 7 . A year later, the exact region near the centromere was defined and later the association of the SBDS gene with the disease was established.
genetics
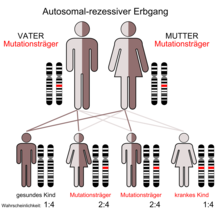
The SBDS is characterized by an autosomal - recessive mode of inheritance. The causative gene (SBDS gene) is on chromosome 7 at position 7q11. It consists of five exons , which for a 1.6 kB large mRNA coding. The SBDS gene is located in a duplicated region. The 97% identical copy is not functional as it contains a number of inactivating mutations and is therefore considered a pseudogene . A study of 158 families found that around 3/4 of disease-related mutations are the result of gene conversion and around 90 percent of those affected had such mutations. A gene conversion takes place when the intact gene and the pseudogen recombine during meiosis and mutated sequences of the pseudogen are copied into the functional gene and thus inactivate it. The most common conversions in the SBDS gene involve a mutation in a splice site and a nonsense mutation in exon 2.
Pathophysiology
The SBDS gene in all tissues expressed and encodes for a protein with 250 amino acids . The function is not known. So far there is no known sequence homology to any other gene from which the function could be inferred. The three-dimensional structure of the SBDS gene orthologous protein of Archaea was investigated and it was found that most mutations affect a region in humans, an unusual structure at the N-terminal relate to the end of the protein. There is a body of evidence that the SBDS protein plays a role in the assembly of ribosomes . The widespread distribution of the protein in all tissues and in eukaryotes and archaea suggests that it is involved in a very fundamental and evolutionarily highly conserved biological process. The localization of the protein in the nucleolus also suggests that the SBDS protein is involved in the metabolism or assembly of the ribosomes . It is not yet clear why the disruption of a very fundamental cellular process causes very specific disorders. However, a similar constellation can also be found in Diamond-Blackfan syndrome , x-linked dyskeratosis congenita and cartilage-hair hypoplasia . Three diseases in which a connection with defective ribosome functions is suspected.
Clinical picture
The patients affected by this disease show a variety of disorders and symptoms. One usually finds the triad of exocrine pancreatic insufficiency , leukopenia and skeletal changes. A neutropenia (special form of leukopenia) may intermittently (intermittent) or occur permanently. The low neutrophil content can be associated with an increased risk of infection and can be life-threatening for the patient. Also, anemia (anemia) and a lack of platelets ( thrombocytopenia ) may occur. The cause of these changes in the blood count is a decrease in the number of cells in the bone marrow , which shows a break in cell maturation in the myeloid cells. As a result, patients may experience increasing bone marrow failure or develop acute myeloid leukemia .
Pancreatic exocrine insufficiency is a result of the loss of the acinar cells in the pancreas that make digestive enzymes . These decrease in number and are replaced by fatty tissue. The lack of digestive enzymes leads to a disorder of fat digestion, resulting in malabsorption syndrome . In contrast to other disorders with congenital exocrine pancreatic insufficiency - for example Johanson-Blizzard syndrome , in which the dysfunction of the pancreas has a progressive character - pancreatic function can improve with SDS over time.
More than half of the patients show a short stature that is not related to the nutritional status. The skeletal changes affect metaphyseal dysostosis in every second patient , just as often changes in the chest , for example with shortened ribs . The skeletal changes are a very variable symptom. However, they seem to occur in all patients with a confirmed diagnosis, albeit to a very different extent. The symptoms are different in individuals with the same genotype . A genotype- phenotype relationship could not be observed.
diagnosis
When the first symptoms are noticed, SBDS may be similar to cystic fibrosis . Cystic fibrosis can be ruled out with a normal sweat test . The varying degrees of symptoms, their temporary nature, and the fact that some symptoms get better over time sometimes make it difficult to diagnose SBDS. This can present either with a malabsorption syndrome or with changes in the blood count. In some patients, the skeletal changes are prominent, including deformation of the ribs, which can make breathing difficult. Usually, the suspected diagnosis is made in the presence of exocrine pancreatic insufficiency with blood count disorders in childhood. The skeletal changes and short stature can support the diagnosis. Since the gene responsible for the disease has been identified, genetic diagnostics can be carried out, although this does not make a careful clinical diagnosis superfluous.
treatment
The exocrine pancreatic insufficiency can be treated by a substitution of the pancreatic enzymes ( pancreatins , fungal enzymes ) and the skeletal abnormalities can make surgical interventions necessary. Neutropenia can be treated with G-CSF . Fears that treatment with G-CSF would increase the risk of leukemia could not be confirmed. If patients have progressive bone marrow depression, a stem cell transplant may be necessary. However, patients with SBDS are said to have an increased risk of developing a graft-versus-host reaction . It is hoped that the investigation of the genetic disorder on which SBDS is based will provide an improved understanding of the molecular causes of the disease and thus possibly new therapeutic options.
Used literature
- C. Shammas, TF Menne, C. Hilcenko, SR Michell, B. Goyenechea, GR Boocock, PR Durie, JM Rommens, AJ Warren: Structural and mutational analysis of the SBDS protein family. Insight into the leukemia-associated Shwachman-Diamond Syndrome . In: J Biol Chem . tape 280 , no. 19 , 2005, pp. 19221-19229 , doi : 10.1074 / jbc.M414656200 , PMID 15701631 .
- S. Cesaro, R. Oneto, C. Messina, BE Gibson, A. Buzyn, C. Steward, E. Gluckman, R. Breddius, M. Boogaerts, C. Vermylen, P. Veys, J. Marsh, I. Badell , G. Michel, T. Gungor, D. Niethammer, P. Bordigoni, C. Oswald, C. Favre, J. Passweg, G. Dini: Haematopoietic stem cell transplantation for Shwachman-Diamond disease: a study from the European Group for blood and marrow transplant . In: Br J Haematol . tape 31 , no. 2 , 2005, p. 231-236 , doi : 10.1111 / j.1365-2141.2005.05758.x , PMID 16197455 .
- J. Donadieu, G. Michel, E. Merlin, P. Bordigoni, B. Monteux, B. Beaupain, G. Leverger, JP Laporte, O. Hermine, A. Buzyn, Y. Bertrand, JL Casanova, T. Leblanc, E. Gluckman, A. Fischer, JL Stephan: Hematopoietic stem cell transplantation for Shwachman-Diamond syndrome: experience of the French neutropenia registry . In: Bone Marrow Transplant . tape 36 , no. 9 , 2005, p. 787-792 , doi : 10.1038 / sj.bmt.1705141 , PMID 16151425 .
- Austin KM, Leary RJ, Shimamura A.: The Shwachman-Diamond SBDS protein localizes to the nucleolus . In: Blood . tape 106 , no. 4 , 2005, p. 1253-1258 , doi : 10.1182 / blood-2005-02-0807 , PMID 15860664 .
- O. Makitie, L. Ellis, PR Durie, JA Morrison, EB Sochett, JM Rommens, WG Cole: Skeletal phenotype in patients with Shwachman-Diamond syndrome and mutations in SBDS . In: Clin Genet . tape 65 , no. 2 , 2004, p. 101-112 , doi : 10.1111 / j.0009-9163.2004.00198.x , PMID 14984468 .
- GRB Boocock, JA Morrison, M. Popovic, N. Richards, L. Ellis, PR Durie, JM Rommens: Mutations in SBDS are associated with Shwachman-Diamond syndrome . In: Nat Genet . tape 33 , no. 1 , 2003, p. 97-101 , doi : 10.1038 / ng1062 , PMID 12496757 .
- M. Popovic, S. Goobie, J. Morrison, L. Ellis, N. Ehtesham, N. Richards, G. Boocock, PR Durie, JM Rommens: Fine mapping of the locus for Shwachman-Diamond syndrome at 7q11, identification of shared disease haplotypes, and exclusion of TPST1 as a candidate gene . In: Eur J Hum Genet . tape 10 , no. 4 , 2002, p. 250-258 , doi : 10.1038 / sj.ejhg.5200798 , PMID 12032733 .
- OP Smith: Shwachman-Diamond syndrome . In: Semin Hematol . tape 39 , no. 2 , 2002, p. 95-102 , doi : 10.1053 / shem.2002.31915 , PMID 11957191 .
- S. Goobie, M. Popovic, J. Morrison, L. Ellis, H. Ginzberg, GR Boocock, N. Ehtesham, C. Betard, CG Brewer, NM Roslin, TJ Hudson, K. Morgon, TM Fujiwara, PR Durie, JM Rommens: Shwachman-Diamond syndrome with exocrine pancreatic dysfunction and bone marrow failure maps to the centromeric region of chromosome 7 . In: Am J Hum Genet . tape 68 , no. 4 , 2001, p. 1048-1054 , doi : 10.1086 / 319505 , PMID 11254457 .
- M. Cipolli: Shwachman-Diamond syndrome: clinical phenotypes. In: Pancreatology . tape 1 , no. 5 , 2001, p. 543-548 , doi : 10.1159 / 000055858 , PMID 12120235 .
- M. Cipolli, C. D'Orazio, A. Delmarco, C. Marchesini, A. Miano, G. Mastella: Shwachman's syndrome: pathomorphosis and long-term outcome . In: J Pediatr Gastroenterol Nutr . tape 29 , no. 3 , 1999, p. 265-272 , doi : 10.1097 / 00005176-199909000-00006 , PMID 10467990 .
- H. Ginzberg, J. Shin, L. Ellis, J. Morrison, W. Ip, Y. Dror, M. Freedman, LA Heitlinger, MA Belt, M. Corey, JM Rommens, PR Durie: Shwachman syndrome: phenotypic manifestations of Sibling sets and isolated cases in a large patient cohort are similar . In: J Pediatr . tape 135 , no. 1 , 1999, p. 81-88 , doi : 10.1016 / S0022-3476 (99) 70332-X , PMID 10393609 .
- VV Michels, GK Donovan: Shwachman syndrome: unusual presentation as asphyxiating thoracic dystrophy . In: Birth Defects Orig Artic Ser . tape 18 , 3B, 1982, pp. 129-134 , PMID 7139093 .
- H. Shwachman, LK Diamond, FA Oski, KT Khaw: The syndrome of pancreatic insufficiency and bone marrow dysfunction . In: J Pediatr . tape 65 , 1964, pp. 645-663 , doi : 10.1016 / S0022-3476 (64) 80150-5 , PMID 14221166 .
- M. Bodian, W. Sheldon, R. Lightwood: Congenital hypoplasia of the exocrine pancreas . In: Acta Pediatr . tape 53 , 1964, pp. 282-293 , doi : 10.1111 / j.1651-2227.1964.tb07237.x , PMID 14158482 .
- Individual evidence
- ↑ M. Bodian et al: Congenital hypoplasia of the exocrine pancreas. In: Acta Pediat. 53, 1964, pp. 282-293. PMID 14158482
- ↑ H. Shwachman, L. Diamond et al .: The syndrome of pancreatic insufficiency and bone marrow dysfunction. In: J Pediat. 65, 1964, pp. 645-663. PMID 14221166 .
- ↑ ensembl.org: Gene: SBDS (ENSG00000126524) Shwachman-Bodian-Diamond syndrome . Retrieved June 26, 2010.
- ↑ C Leong Ng, David G Waterman, Eugene V Koonin, Alison D Walters, James PJ Chong, Michail N Isupov, Andrey A Lebedev, David HJ Bunka, Peter G Stockley, Miguel Ortiz-Lombardía, Alfred A Antson: Conformational flexibility and molecular interactions of an archaeal homologue of the Shwachman-Bodian-Diamond syndrome protein. In: BMC Structural Biology. 2009, 9, p. 32. doi: 10.1186 / 1472-6807-9-32 ( Open Access )
- ^ GW Hall, P. Dale, JA Dodge. Shwachman-Diamond syndrome: UK perspective. In: Arch Dis Child . 2006 Jun; 91 (6), pp. 521-524. PMID 16714727
- ↑ O. Mäkitie, L. Ellis, PR Durie, JA Morrison, EB Sochett, JM Rommens, WG Cole: Skeletal phenotype in patients with Shwachman-Diamond syndrome and mutations in SBDS. In: Clin Genet. 2004 Feb; 65 (2), pp. 101-112. PMID 14984468
- ^ Confer / Miller: Long-term safety of filgrastim (rhG-CSF) administration. In: British Journal of Hematology . (2007); 137 (1), pp. 76–80, PMC 1920544 (free full text)
- ↑ L. Burroughs, A. Woolfrey, A. Shimamura: Shwachman-Diamond syndrome: a review of the clinical presentation, molecular pathogenesis, diagnosis, and treatment. In: Hematol Oncol Clin North Am. 2009 Apr; 23 (2), pp. 233-248. PMID 19327581 .
Web links
- Shwachman-Bodian-Diamond Syndrome. In: Online Mendelian Inheritance in Man . (English)
- Shwachman-Bodian-Diamond Syndrome. In: Orphanet (Rare Disease Database).
- GeneReviews / NCBI / NIH / UW entry on Shwachman-Diamond Syndrome
- Shwachman-Diamond Syndrome research study of Inherited Bone Marrow Failure Syndromes (IBMFS)
- Shwachman-Diamond Syndrome Foundation