Johanson Blizzard Syndrome
| Classification according to ICD-10 | |
|---|---|
| Q45.0 | Other congenital malformations of the digestive system |
| ICD-10 online (WHO version 2019) | |
The Johanson-Blizzard syndrome (JBS) is a rare, often fatal, genetic disease of multiple organ systems , by an impaired development of the pancreas , nose is characterized and scalp with mental retardation , hearing loss and short stature associated. The disorder is sometimes described as ectodermal dysplasia and is commonly viewed as an inherited disease of the pancreas. The disease is named after the American pediatricians Ann J. Johanson and Robert. M. Blizzard, who first described this disorder in 1971.
Inheritance
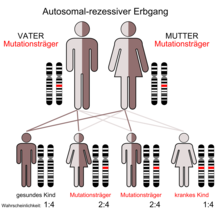
Johanson-Blizzard syndrome is inherited as an autosomal recessive trait. This means that mutations on both alleles of the ubiquitin gene are necessary in order to express the corresponding phenotype. The parents of those affected (carriers) are usually phenotypically healthy.
Pathophysiology
The JBS is caused by mutations in the UBR1 gene. UBR1 encodes a ubiquitin - ligase . Ubiquitins are proteins that are universally expressed in eukaryotic organisms. They play a role in the post-translational modification of other proteins by marking them for degradation when necessary. Ubiquitins work in such a way that the ubiquitin ligases covalently bind a ubiquitin to a lysine residue of the (faulty) target protein. The ubiquitin ligases repeat this process so that over time a chain of ubiquitins forms on the target proteins. This is called polyubiquination. This is a signal for the proteasome to break down the defective target protein. In this way, the ubiquitin-proteasome system plays a central role in the lysosomal degradation of intracellular proteins.
But ubiquitins can also be involved in the post-translational modification of normal proteins. Both processes, post-translational degradation and modification, are important in eukaryotic cells for the regulation of central processes such as cell division , signaling pathways , apoptosis , the response to inflammatory stimuli and the control of developmental processes .
In JBS, the mutations of the UBR1 gene lead to the synthesis of the ubiquitin ligase being disturbed or interrupted. In healthy individuals, more UBR1 is made in the pancreatic ducts than in any other cell in the body. The dysfunction of the ubiquitin-proteasome complex, which can be traced back directly to the reduced production of the ubiquitin ligase, is the direct cause of the chronic inflammatory processes in the pancreas, which is associated with the replacement of the organ stroma by adipose and connective tissue and to errors in the innervation of the acini and islets of Langerhans. It is also responsible for the failure of apoptosis in damaged cells and for faulty protein production. This also applies to other tissues that are susceptible to defective UBR1 expression, particularly the craniofacial area, the central nervous system , skeletal muscle innervation and tooth formation .
In JBS, mutations have been found in the UBR1 gene that lead to chain termination ( nonsense mutations ), those that lead to an amino acid exchange ( missense mutations ) and splice site mutations in both parents of affected patients. This confirms the assumption that the JBS phenotype is homozygous . The variable expression of the phenotype with residual ubiquitin ligase activity in some patients is explained by the occurrence of so-called hypomorphic mutations in one of the parents. The UBR1 gene is located on human chromosome 15 .
Clinical picture
Disorders of the pancreatic function
The cardinal symptom of JBS is exocrine pancreatic insufficiency . The associated lack of lipase , trypsin , trypsinogen and other components of the pancreatic secretion leads in particular to fat malabsorption and, together with a disturbance of the endocrine pancreatic functions (disturbed glucagon secretion when the pancreas does not react to hypoglycaemia ), is the main problem in patients with A JBS. In JBS, exocrine pancreatic insufficiency, which occurs together with developmental disorders of apoptosis in the pancreatic tissue, as well as prenatal and chronic inflammatory damage to the pancreatic ducts, can appear as a result of congenital obesity of the pancreatic ducts. Cases have been reported of complete obesity of the pancreas. This is an ongoing, sometimes fatal, process.
As already mentioned, the JBS is also associated with endocrine pancreatic insufficiency. In the islets of Langerhans , the hormones glucagon , insulin and somatostatin produced. JBS can lead to connective tissue remodeling of the pancreas, resulting in fatty replacement or defective innervation of the islets. This often leads to diabetes mellitus . In one case, insulin resistance was also described as the cause . The production of pancreatic secretions along with electrolytes and bicarbonate is often unaffected in patients with JBS.
Other endocrine disorders
Other endocrine disorders can occur with JBS. Thus, hypothyroidism , growth hormone deficiency and pituitary insufficiency have been observed. In the latter, hamartomas and disorders of the adenohypophysis were found to be the cause. The growth disturbance and the resulting short stature in JBS can be a consequence of the growth hormone deficiency in anterior pituitary insufficiency and the associated fat malabsorption .
nose
The malformations of the nostrils is a characteristic feature of JBS. A partial application and complete absence of cartilage , muscle and connective tissue of the nose are described. This results in a very unusual appearance of the nose in patients.
Nervous system
Many patients with JBS show a lack of talent , which can be differently pronounced. Individual cases with normal intelligence and age-appropriate social development have been described.
Hearing
Changes in the inner ear lead to bilateral inner ear hearing loss in many patients with JBS . Cystic changes of the cochlea and equilibrium organ with a consequent expansion have been described as the cause . Changes to the temporal bone contribute to the hearing loss because it affects the innervation and development of the inner ear.
Craniofacial dysmorphism
Changes that affect the head, face, jaw (anatomy) and teeth are summarized under the term craniofacial dysmorphism . The changes found during the JBS are varied, they relate to the following organs or body parts: defects of the scalp with an irregular hair growth, thin scalp until Aplasia cutis congenita , enlarged fontanelle , size reduction of the head ( microcephaly ), curved end, absence of eyebrows and eyelashes , Eye shape similar to Down's syndrome , fistulas of the lacrimal duct , flattened auricles., Micrognathia (small jaws, mainly affecting the lower jaw), congenital fissure formation in the bones around the eye socket and incorrectly placed milk teeth in the absence of permanent teeth, or microdontics .
Disorders of other organ systems
Other congenital disorders affect other organs. The less common disorders are: anal atresia , vesicorenal reflux ; Double structures of the uterus and vagina in girls, jaundice in the newborn due to liver fibrosis with portal hypertension ; Dilated cardiomyopathy , dextrocardia , atrial septal defect, and ventricular septal defect ; low birth weight , failure to thrive , hypotonia ; Congenital cataracts (medicine) * and café-au-lait spots .
Diagnosis and differential diagnosis
Review articles by various authors have described exocrine pancreatic insufficiency as a cardinal symptom, regardless of the number of cases published to date. Clinically, however, this is not always observed from the start due to the progressive nature of the tissue damage. During the first year of life, a typical picture of a malabsorption syndrome with bulky, greasy stools usually develops. If one looks at the most common symptoms, then about a dozen publications (n = 38) find the combination of malabsorption syndrome due to exocrine pancreatic insufficiency, hypoplasia of the nostrils, giftedness and scalp lesions. Older studies also listed short stature as a frequent symptom with a lower number of cases (n = 22). In cases in which the patient has no or only discrete further signs, the differential diagnosis of congenital pancreatic insufficiency then arises. Apart from JBS, essentially only cystic fibrosis and Shwachman-Bodian-Diamond syndrome (SBDS) come into question. If CF is not an option due to the other clinical findings, the differential diagnosis to SBDS can be made simply on the basis of the intact bicarbonate excretion in JBS. A genetic analysis then confirms the suspected diagnosis. In the overwhelming majority of cases described so far, a suspected diagnosis can be made based on the combination of pancreatic insufficiency and the most common abnormalities. These are (in almost all cases) hypoplasia or aplasia of the ala associated with the presence of a narrow, long upper lip, which gives the patient a very characteristic appearance, as well as (less often) scalp defects, inner ear hearing loss and microcephaly. Short stature and mental retardation to a very variable extent can also be present.
treatment
While there is no cure for JBS, alleviating individual symptoms can be quite effective. The severity of the severity of individual symptoms determines the necessity and the chances of success of the selected treatment method. Pancreatic insufficiency is usually substituted with pancreatin , and rizoenzymes are also available. The craniofacial and skeletal deformities can be corrected surgically if necessary. In the event of hearing loss, hearing aids can be prescribed and appropriate training courses indicated. Patients with less talent benefit from occupational therapy measures specially adapted for JBS sufferers .
See also
Individual evidence
- ^ Johanson A, Blizzard R: A syndrome of congenital aplasia of the alae nasi, deafness, hypothyroidism, dwarfism, absent permanent teeth, and malabsorption . In: J. Pediatr. . 79, No. 6, December 1971, pp. 982-7. PMID 5171616 .
- ↑ a b c d e f g h i j k l m n o p q r s t u v w Alkhouri N, Kaplan B, Kay M, Shealy A, Crowe C, Bauhuber S, Zenker M: Johanson-Blizzard syndrome with mild phenotypic features confirmed by UBR1 gene testing Archived from the original on February 18, 2012. Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice. (Free full text) In: World journal of gastroenterology: WJG . 14, No. 44, November 2008, pp. 6863-6866. doi : 10.3748 / year 14.6863 . PMID 19058315 .
- ↑ a b c d e f g h Zenker M, Mayerle J, Lerch MM, Tagariello A, Zerres K, Durie PR, Beier M, Hülskamp G, Guzman C, Rehder H, Beemer FA, Hamel B, Van Lieferinghen P, Gershoni Baruch R, Vieira MW, Dumic M, Auslender R, Gil-Da-Silva-Lopes VL, Steinlicht S, Rauh M, Shalev SA, Thiel C, Ekici AB, Winterpacht A, Kwon YT, Varshavsky A, Reis A: Deficiency of UBR1, a ubiquitin ligase of the N-end rule pathway, causes pancreatic dysfunction, malformations and mental retardation (Johanson-Blizzard syndrome). . In: Nature Genetics . 37, No. 12, December 2005, pp. 1345-1350. doi : 10.1038 / ng1681 . PMID 16311597 .
- ↑ a b c Wang J, Maldonado MA: The ubiquitin-proteasome system and its role in inflammatory and autoimmune diseases . In: Cell. Mol. Immunol. . 3, No. 4, August 2006, pp. 255-61. PMID 16978533 .
- ↑ a b Ciechanover A: The ubiquitin-mediated proteolytic pathway: mechanisms of action and cellular physiology . In: Biological Chemistry Hoppe-Seyler . 375, No. 9, September 1994, pp. 565-81. PMID 7840898 .
- ↑ a b Ciechanover A, Iwai K: The ubiquitin system: from basic mechanisms to the patient bed . In: IUBMB Life . 56, No. 4, April 2004, pp. 193-201. doi : 10.1080 / 1521654042000223616 . PMID 15230346 .
- ↑ a b c d Zenker M, Mayerle J, Reis A, Lerch MM: Genetic basis and pancreatic biology of Johanson-Blizzard syndrome . In: Endocrinology and metabolism clinics of North America . 35, No. 2, June 2006, pp. 243-253, vii-viii. doi : 10.1016 / j.ecl.2006.02.013 . PMID 16632090 .
- ↑ a b c d Al-Dosari MS, Al-Muhsen S, Al-Jazaeri A, Mayerle J, Zenker M, Alkuraya FS: Johanson-Blizzard syndrome: report of a novel mutation and severe liver involvement . In: Am. J. Med. Genet. A . 146A, No. 14, July 2008, pp. 1875-9. doi : 10.1002 / ajmg.a.32401 . PMID 18553553 .
- ↑ a b
- ^ A b Sandhu BK, Brueton MJ: Concurrent pancreatic and growth hormone insufficiency in Johanson-Blizzard syndrome . In: J Pediatr Gastroenterol Nutr . 9, No. 4, November 1989, pp. 535-8. PMID 2621533 .
- ↑ a b c Steinbach WJ, Hintz RL: Diabetes mellitus and profound insulin resistance in Johanson-Blizzard syndrome. . In: Journal of pediatric endocrinology & metabolism: JPEM . 13, No. 9, November 2000, ISSN 0334-018X , pp. 1633-1636. PMID 11154160 .
- ↑ a b c d e Rosanowski F, Hoppe U, Hies T, Eysholdt U: Johanson-Blizzard syndrome. A complex dysplasia syndrome with aplasia of the nasal alae and inner ear deafness . In: ENT . 46, No. 10, October 1998, pp. 876-878. doi : 10.1007 / s001060050328 . PMID 9846268 .
- ↑ a b c d Takahashi T, Fujishima M, Tsuchida S, Enoki M, Takada G: Johanson-blizzard syndrome: loss of glucagon secretion response to insulin-induced hypoglycemia. . In: Journal of pediatric endocrinology & metabolism: JPEM . 17, No. 8, August 2004, ISSN 0334-018X , pp. 1141-1144. PMID 15379429 .
- ↑ a b c d e f Daentl DL, Frías JL, Gilbert EF, Opitz JM: The Johanson-Blizzard syndrome: case report and autopsy findings. . In: American journal of medical genetics . 3, No. 2, 1979, pp. 129-135. doi : 10.1002 / ajmg.1320030203 . PMID 474625 .
- ↑ Jones NL, Hofley PM, Durie PR: Pathophysiology of the pancreatic defect syndromes in Johanson-Blizzard: a disorder of acinar development. . In: The Journal of Pediatrics . 125, No. 3, September 1994, pp. 406-408. doi : 10.1016 / S0022-3476 (05) 83286-X . PMID 8071749 .
- ^ A b Nagashima K, Yagi H, Kuroume T: A case of Johanson-Blizzard syndrome complicated by diabetes mellitus . In: Clinical genetics . 43, No. 2, February 1993, ISSN 0009-9163 , pp. 98-100. PMID 8448911 .
- ↑ a b c Gould NS, Paton JB, Bennett AR: Johanson-Blizzard syndrome: clinical and pathological findings in 2 sibs. . In: American journal of medical genetics . 33, No. 2, June 1989, pp. 194-199. doi : 10.1002 / ajmg.1320330212 . PMID 2669481 .
- ↑ a b c d Kulkarni ML, Shetty SK, Kallambella KS, Kulkarni PM: Johanson - blizzard syndrome . In: Indian journal of pediatrics . 71, No. 12, December 2004, pp. 1127-1129. doi : 10.1007 / BF02829829 . PMID 15630323 .
- ↑ Hoffman WH, Lee JR, Kovacs K, Chen H, Yaghmai F: Johanson-Blizzard syndrome: autopsy findings with special emphasis on hypopituitarism and review of the literature. . In: Pediatric and developmental pathology: the official journal of the Society for Pediatric Pathology and the Pediatric Pathology Society . 10, No. 1, January 2007, pp. 55-60. doi : 10.2350 / 06-05-0085.1 . PMID 17378628 .
- ↑ a b c d e f g h Fichter CR, Johnson GA, Braddock SR, Tobias JD: Perioperative care of the child with the Johanson-Blizzard syndrome . In: Pediatr Anaesth . 13, No. 1, January 2003, pp. 72-5. PMID 12535044 .
- ^ Johanson-Blizzard Syndrome. In: Online Mendelian Inheritance in Man . (English)
- ^ A b Moeschler JB, Polak MJ, Jenkins JJ, Amato RS: The Johanson-Blizzard syndrome: a second report of full autopsy findings . In: Am. J. Med. Genet. . 26, No. 1, January 1987, pp. 133-8. doi : 10.1002 / ajmg.1320260120 . PMID 3812553 .
- ↑ a b c d Braun J, Lerner A, Gershoni-Baruch R: The temporal bone in the Johanson-Blizzard syndrome. A CT study . In: Pediatr Radiol . 21, No. 8, 1991, pp. 580-3. PMID 1815181 .
- ↑ Bamiou DE, Phelps P, Sirimanna T: Temporal bone computed tomography findings in bilateral sensorineural hearing loss . In: Arch. Dis. Child. . 82, No. 3, March 2000, pp. 257-60. PMID 10685935 . PMC 1718255 (free full text).
- ^ A b c Mardin MK, Ghandour M, Sakati NA, Nyhan WL: Johanson-Blizzard syndrome in a large incorporated kindred with three involved members . In: Clin Genet. . 14, No. 5, November 1978, pp. 247-250. PMID 709902 .
- ↑ a b c Kobayashi S, Ohmori K, Sekiguchi J: Johanson-Blizzard syndrome facial anomaly and its correction using a microsurgical bone graft and tripartite osteotomy . In: J Craniofac Surg. . 6, No. 5, September 1995, pp. 382-385. doi : 10.1097 / 00001665-199509000-00011 . PMID 9020718 .
- ↑ Motohashi N, Pruzansky S, Day D: Roentgencephalometric analysis of craniofacial growth in the Johanson-Blizzard syndrome . In: J Craniofac Genet Dev Biol. . 1, No. 1, 1981, pp. 57-72. PMID 7341643 .
- ↑ a b c Dumić M, Ille J, Bobonj G, Kordić R, S Batinica: [The Johanson-Blizzard syndrome] . In: Lijec Vjesn . 120, No. 5, May 1998, pp. 114-6. PMID 9748788 .
- ↑ Vieira MW, Lopes VL, Teruya H, Guimarães-Lamonato L, Oliveira LC, Costa CD. Johanson-Blizzard syndrome: the importance of differential diagnostic in pediatrics. In: J Pediatr (Rio J). 2002 Sep-Oct; 78 (5): 433-6. PMID 14647752
- ↑ Hurst JA, Baraitser M. Johanson-Blizzard syndrome. in: J Med Genet . 1989 Jan; 26 (1): 45-8. PMID 2645405
- ↑ Schneider et al .: Pancreatic enzyme replacement therapy: Comparative effects of conventional and enteric-coated microspheric pancreatin and acid-stable fungal enzyme preparations on steatorrhoea in chronic pancreatitis. Hepato Gastroenterol. 32: 1985, pp. 97-102.
- ↑ Prater JF, D'Addio K: Johanson-Blizzard syndrome - a case study, behavioral manifestations, and successful treatment strategies . In: Biol. Psychiatry . 51, No. 6, March 2002, pp. 515-7. PMID 11922888 .
Web links
- Johanson Blizzard Syndrome. In: Online Mendelian Inheritance in Man . (English)