Cirrhosis of the liver
| Classification according to ICD-10 | |
|---|---|
| K74 | Fibrosis and cirrhosis of the liver |
| K74.0 | Liver fibrosis |
| K74.1 | Liver sclerosis |
| K74.2 | Liver fibrosis with liver sclerosis |
| K74.3 | Primary biliary cirrhosis, chronic non-purulent destructive cholangitis |
| K74.4 | Secondary biliary cirrhosis |
| K74.5 | Biliary cirrhosis, unspecified |
| K74.6 | Other and unspecified cirrhosis of the liver |
| K70.3 | Alcoholic cirrhosis of the liver |
| ICD-10 online (WHO version 2019) | |
The liver cirrhosis , outdated cirrhosis (of Greek κίρρωσις kírrosis from kirrós , yellow-orange ',' lemon yellow ',' yellow ', after sometimes yellow by obesity sectional area of René Laënnec term coined) is the final stage of chronic liver diseases . This stage is considered irreversible, even if there are individual reports of cures. Typically, cirrhosis develops over years or decades; faster courses of less than a year are less common. Almost all chronic liver diseases lead to end-stage liver cirrhosis. In Europe , alcohol abuse , non-alcoholic fatty liver disease and chronic viral hepatitis are the most common causes.
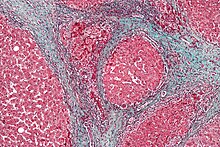
The chronic process of destruction and regeneration of the liver tissue creates a disturbed tissue architecture with nodular changes. In addition, excessive connective tissue forms (fibrosis). These scarred areas can take up more than 50% of the total tissue of a cirrhotic liver. As a result, the blood flow to the liver is disturbed, the blood accumulates in front of the liver in the area of the portal vein ( portal hypertension ).
The incidence , i.e. H. the number of new cases in the industrialized countries is 250 per 100,000 inhabitants per year. The ratio of sick men to women is 2: 1. It is estimated that around one million people in Germany suffer from cirrhosis of the liver.
causes
Alcoholic cirrhosis of the liver
The alcoholism is in developed countries with about 50% of cases, the most common cause of cirrhosis of the liver. The massive consumption of alcohol and the resulting high rate of metabolism of ethanol to ethanal lead to a sharp increase in the NADH / NAD quotient in the body. The increase in the redox potential of the pyridine nucleotides inhibits the citric acid cycle . In this situation, the acetyl-CoA is mainly used in the liver to an increased extent for fatty acid synthesis and ultimately for the accumulation of triglycerides ( fat ). This fatty liver is initially fully reversible, but with continued alcohol consumption it leads to fatty liver disease and thus ultimately to cirrhosis of the liver.
Fatty liver (steatosis hepatis)
Fatty liver is the most common liver finding in Germany. This liver disease is characterized by fat storage in the liver cells, which is still reversible in the initial course. A simple fatty liver that only affects the well-being does not lead to liver damage. However, it can ignite; A distinction is made between alcoholic steatohepatitis (ASH) caused by alcohol consumption and non-alcoholic steatohepatitis (NASH). Both forms can lead to scarring of the liver, which increases the risk of developing liver cirrhosis. In the ASH is Interleukin-8 is increased in the liver tissue, which is neutrophilic granulocytes (white blood cells) can store in the liver. Another mechanism is the formation of leukotriene -B4 from arachidonic acid , which also attracts inflammatory cells .
Other causes
- Liver cirrhosis in chronic viral hepatitis (second most common cause in industrialized countries with 20-25%, most common in Africa with 90%) - mostly hepatitis C , which remains chronic in 85% and leads to cirrhosis in 35%
- cryptogenic liver cirrhosis (without demonstrable etiology )
- Cirrhosis of congestion ( Cirrhosis cardiaque ), typical of right heart failure
- Autoimmune hepatitis
- rare forms of cirrhosis with a defined etiology
- Hemochromatosis
- Wilson disease
- Galactosemia
- hereditary fructose intolerance
- Cystic fibrosis
- Glycogen storage disease
- cholangiodysplastic cirrhosis of the liver
- primary sclerosing cholangitis
- Budd-Chiari Syndrome
- Tropical diseases
- Cirrhosis with alpha-1 antitrypsin deficiency
- primary biliary cholangitis (previously: primary biliary cirrhosis)
- secondary biliary cirrhosis
- Hepatopathy in celiac disease (gluten-sensitive enteropathy)
- Cirrhosis of the liver from substances that are toxic to the liver such as carbon tetrachloride (metal processing) and rarely also from drugs such as methotrexate
| Percentage distribution of the cause | |
| Alcohol abuse | approx. 30-40% |
| chronic viral hepatitis B, C and D | approx. 30% |
| cryptogenic liver cirrhosis | approx. 10% |
| less common causes of cirrhosis of the liver | approx. 10% |
Pathogenesis
The cause of cirrhosis is the necrosis (death) of liver cells. B. by viruses or poisons. The cells release cytokines that activate liver macrophages ( Kupffer cells ) and fat storage cells in the liver ( Ito cells ) on the one hand and monocytes and granulocytes from the blood on the other . Through these cells, the body structure is parenchyma - necrosis , formation of regenerative nodules (Pseudolobuli) and fibrous septa rebuilt destructive. These connective tissue nodes interrupt the ducts of the liver, which bring the bile to the gallbladder via the bile ducts (canaliculi and ducts), carry nutrients from the portal blood into the body, detoxify the hepatocytes with pollutants and supply the liver with oxygen-rich blood. Bile ducts form new, but end up blind. As a result, blood accumulates between the liver and the digestive tract ( portal hypertension ), which causes ascites to form and the spleen to enlarge . In the worst case, esophageal variceal bleeding occurs . The failure of the hepatocytes also causes the hepatic encephalopathy : In cirrhosis of the liver, the ammonia metabolism is reduced by up to 80%, with the ammonia formed in the intestine being conducted past the liver via vascular collaterals. Due to the lack of degradation, the toxin concentration in the blood increases and ammonia crosses the blood-brain barrier. The astrocytes in the brain swell and brain edema can develop, which can lead to mostly episodic cognitive deficits. Ultimately, the inadequate detoxification function of a cirrhotic liver can lead to hepatic coma . The true Hepatic encephalopathy as a predictor of a particularly serious course of liver cirrhosis. In one study, almost half of all liver cirrhosis patients with hepatic encephalopathy died within one month of the diagnosis. Study data also show a reduction in the risk of further liver cirrhosis complications such as spontaneous bacterial peritonitis (SBP) or variceal bleeding in the context of treatment for hepatic encephalopathy .
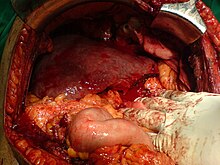
The pathologist distinguishes micronodular, macronodular and mixed-nodular cirrhosis according to the external appearance of the organ. The liver shrinks, its surface becomes wrinkled and knotty. Active or florid (i.e. progressive) and inactive cirrhosis can be distinguished microscopically . The preliminary stage of liver cirrhosis is liver fibrosis .
Symptoms
Early but unspecific symptoms of liver cirrhosis can include decreased performance, poor concentration and tiredness. In addition, the so-called liver skin signs can occur, which are noticeable , among other things, by red-colored little finger pads, yellowish skin ( jaundice ) and spider naevi . Liver cirrhosis often only affects the subjective feeling of the affected patient at a very late stage of the disease. The liver function can be impaired in very different ways with regard to the synthesis function ( coagulation factors , albumin ) and the detoxification function ( liver coma ). Until complications develop, one speaks of compensated liver cirrhosis. A decompensated liver cirrhosis is present as soon as clinically relevant complications such as portal hypertension (resulting esophageal varices = varicose veins in the esophagus), ascites , a larger pleural effusion (or hepatic hydrothorax ) or enlargement of the spleen (lack of platelets ) and hepatic encephalopathy occur. The latter is a brain dysfunction in which the impaired liver function leads to an increase in toxic metabolites that cause brain cells to swell. The symptoms of hepatic encephalopathy also include dizziness, disorientation, tiredness, difficulty concentrating, memory loss, changes in personality and even hepatic coma. Other typical symptoms of liver cirrhosis are reddening of the palms of the hands ( palmar erythema ), caput medusae , spider nevi ( nevus araneus ), rhagades , lacquer tongue and edema . In the so-called Child-Pugh score classification, several of these factors are included ( bilirubin , Quick value , albumin , hepatic encephalopathy and ascites ) and a score is calculated from them; the resulting classification into stages A to C allows a statement to be made about the prognosis of the disease; patients in stage C according to Child-Pugh have a very poor prognosis with regard to survival time. Hepatic encephalopathy and ascites are only assessed in three degrees of severity, which leads to more or less subjective, inaccurate values. That is why the MELD-Score has been used since 2002 , which is calculated from laboratory parameters ( creatinine , bilirubin and INR ) according to a specific formula . Liver cirrhosis is an optional precancerous condition , i.e. This means that a malignant tumor, hepatocellular carcinoma (HCC) , can develop from cirrhosis of the liver .
diagnosis
The examination often reveals jaundice , a larger abdominal circumference (due to ascites ), edema , gynecomastia , skin bleeding and, in the case of hepatic encephalopathy , flapping tremor and impaired consciousness . Typical, but appearing late, are the so-called liver skin signs : Spider Naevi (vascular spider), " milk glass nails" (opaque white discoloration of the fingernails with distal longitudinal red-brown coloration, also called " Terry nails "), prurigo ( itching ), lacquer tongue , Skin atrophy (“banknote skin”) and palmar or plantar erythema (reddening of the palms of the hands or the soles of the feet). However, these signs are not only specific for cirrhosis of the liver, but can also be discreet in other liver disorders, such as B. the fatty liver occur. This can e.g. B. also temporarily be the case during pregnancy . Other signs of the liver are caput medusae , Dupuytren's contractures and a lack of abdominal hair in men (bald head, " bald head ").
In the laboratory, reduced levels of cholinesterase , albumin and some coagulation factors (reduced Quick level ) are noticeable due to the liver's limited synthesis capacity . The liver enzymes AST (GOT) , ALT (GPT) as well as γ-GT , bilirubin and ammonia can be increased. However, the level of the ammonia level alone is not indicative of the presence of hepatic encephalopathy .
The liver is inhomogeneous on ultrasound . The edge of the liver is wavy, the internal vessels are rarefied. The caudate lobe may be enlarged. An ascites and an enlarged spleen ( splenomegaly ) can be recognized very well with the ultrasound . The so-called Fibroscan, also known as transient elastography, represents an improved form of sonography. It can be used to determine the fibrosis, i.e. the remodeling of connective tissue, of the liver, which provides a very reliable result for diagnosis and could replace liver biopsy (see below) in the future. Color duplex sonography can be used to measure reduced elasticity of the liver in the hepatic veins, reduced flow in the portal vein and increased peripheral resistance in the hepatic artery .
The definitive diagnosis is made by a liver biopsy.
The Child-Pugh score , which is used both for staging (Child A – C) and for estimating the prognosis, is created from various examination findings .
therapy
The therapy is based on general nutritional measures such as omitting all substances that are potentially toxic to the liver (alcohol, medication), compensating for a vitamin deficiency (e.g. vitamin B1 in alcoholism) and an adequate supply of energy. Malnourished patients have both an increased mortality in the spontaneous course of the disease and an increased rate of complications. Food should preferably be consumed orally, especially patients with advanced liver cirrhosis benefit from parenteral nutrition. This is not yet indicated in the early stages. The energy intake should be around 145–167 kJ (35–40 kcal) per kilogram of body weight. If the liver cirrhosis is in the end stage, the patient's life is acutely threatened. Due to the scarce availability of donor organs, the severity of the procedure and the subsequent use of drugs that suppress the immune system, liver transplantation is the last possible treatment option to save the patient. A suitable donor organ replaces the cirrhotic liver.
Carbohydrate intake
Inadequate carbohydrate intake can worsen an existing catabolic metabolic situation. This can be explained by the fact that in this situation not only fats but also proteins are metabolized for energy production. The DDG advises diabetics with liver cirrhosis against low-carbohydrate diets.
Protein intake
A daily protein amount of 1.2–1.5 g protein per kg body weight is recommended. Protein restriction should only be used in patients with treatment-resistant chronic hepatic encephalopathy . If necessary, leucine , isoleucine and valine ( branched-chain amino acids ) should be substituted in these patients .
Osteoporosis prophylaxis
Osteoporosis prophylaxis should be initiated in all patients at an early stage. This is done through calcium substitution (1200–1500 mg / d). In patients with cholestatic liver disease, vitamin D3 is also substituted (400–800 IU / d). In patients of advanced age (> 65 years), underweight patients and smokers, a basic diagnosis should be carried out early.
Vitamin substitution
A vitamin K substitution is indicated if there is an increased risk of bleeding and low Quick values . Since the enteral absorption of this lipophilic vitamin is reduced in the case of cholestasis, the substitution should take place in an increased dose (10 mg every 10 weeks) orally or parenterally . Vitamin B1 deficiency is 50% in alcoholic patients . This should also be substituted - especially if you continue to consume alcohol as a prophylaxis for Wernicke encephalopathy .
Non-nutritional measures
The underlying disease must be treated, with alcohol dependence , a withdrawal treatment is attempted, patients with autoimmune hepatitis are treated with immunosuppression , with chronic hepatitis B virus elimination with interferons can be attempted. In hepatitis C , antiviral therapy leads to virus elimination in over 90% of those affected (no viruses can be detected in the blood). Complications of cirrhosis of the liver are treated with specific measures. When bleeding from esophageal varices , the primary goal is to stop the bleeding, as otherwise fatal blood loss can threaten. If there is a severe form of ascites , the ascites can be drained through a targeted puncture. A hepatic encephalopathy is treated with medication; The primary goal is to reduce the further production of ammonia and other toxins. The intestinal-selective antibiotic rifaximin is available as a possible therapy option for preventing recurrence . Among other things, it kills the ammonia-producing bacteria in the intestine and reduces the relative risk of recurring episodes of hepatic encephalopathy. Another drug is lactulose , a synthetic disaccharide that influences the intestinal flora in favor of lactic acid-producing bacteria, thereby suppressing ammonia-producing intestinal bacteria. L-ornithine-L-aspartate , which promotes the conversion of ammonia to harmless urea, can also be used to treat hepatic encephalopathy . The urea can then be excreted in the urine.
Important to regular examinations for early detection of liver cancer . In many cases, a last resort is a liver transplant .
There is some evidence that consuming caffeine in the form of coffee can protect the liver from developing cirrhosis or delay its development. The polyphenols, a group of plant substances that occur in particularly high quantities in coffee, could play a major role here.
The prognosis depends on the cause, successful causal treatment, complications, and stage. The one-year survival rates for patients in stage Child A are almost 100%, for Child B around 85% and for Child C 35%. The MELD score can be used to make statements about survival in the next three months. For example, a patient in the hospital with a score of 20-30 has a 25% risk of dying in the next three months. A cirrhotic with a MELD of 40 will most likely have died in three months.
history
The first macroscopic description of liver cirrhosis in the history of medicine can be found in the notes on the drawing del vecchio by Leonardo da Vinci (1452-1519). The drawings of the vascular anatomy of the liver are based on an autopsy carried out by Leonardo da Vinci in Florence in 1508 on a man over 100 years old.
literature
- Herbert Renz-Polster , Steffen Krautzig: Basic textbook internal medicine . 4th edition. 2006, p. 708 ff .
- Gerd Herold : Internal Medicine . 2009, p. 518 ff .
- German Liver Foundation (Ed.): Internal Medicine . 2009, p. 518 ff .
Web links
Individual evidence
- ↑ Hans Adolf Kühn: Liver cirrhosis. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition ibid. 1961, pp. 863-868, here: p. 863.
- ↑ Hans-Werner Altmann : Disease names as a reflection of medical knowledge. In: Würzburg medical history reports. Volume 3, 1985, pp. 225-241, here: pp. 228 f.
- ↑ Roeb et al. In: Z Gastroenterol , 2015, 53, pp. 668–723
- ↑ Cirrhosis of the liver and its complications . ( Memento of the original from July 2, 2010 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Lebertransplantation.de, 2001; Retrieved October 22, 2010
- ^ Gertrud Rehner, Hannelore Daniel: Biochemistry of nutrition . 3. Edition. Spektrum Akademischer Verlag, 2010, ISBN 978-3-8274-2041-1 , p. 491 .
- ↑ Deutsche Leberhilfe e. V., Fettleber (NASH / ASH) In: Leberhilfe.org, accessed on August 2, 2017
- ↑ Thomas Zilker: Alcoholic cirrhosis of the liver. The toxicologist's point of view. In: Clinic Doctor . tape 41 , no. 6 + 7 , 2012, pp. 310-314 .
- ↑ N Sheron, G Bird, J Koskinas, et al .: Circulating and tissue levels of the neutrophil chemotoxin interleukin-8 are elevated in severe acute alcoholic hepatitis, and tissue levels correlate with neutrophil infiltration. In: Hepatology . tape 18 , 1993, p. 41-46 .
- ^ FJ Roll, HD Perez, LN Serhan: Charactrization of a novel arachidonic acid-derived neutrophil chemoatractant. In: Biochemical and Biophysical Research Communications . tape 186 , 1992, pp. 268-276 .
- ↑ H. Renz-Polster, S. Krautzig: Basic textbook internal medicine 4th ed., 2006, p. 709.
- ↑ hepatitisandmore.de (PDF)
- ↑ JS Bajaj, CM Schubert, DM Heuman, JB Wade, DP Gibson, A Topaz, K Saeian, M Hafeezullah, DE Bell, RK Sterling, RT Stravitz, V Luketic, MB White, AJ Sanyal: Persistence of cognitive impairment after resolution of overt hepatic encephalopathy . In: Gastroenterology , 2010, 138, pp. 2332-2340, doi: 10.1053 / j.gastro.2010.02.015
- ↑ H. Grüngreiff: Thieme Refresher Internal Medicine . 2014, R1-R16
- ↑ KJBühling, J. Lepenies, K. Witt: Intensive Course - General and special pathology . 3. Edition. 2004, p. 233 ff
- ^ Association of Scientific Medical Societies. S2k guideline: complications of liver cirrhosis. November 2018 [Access: May 3, 2019].
- ↑ Jepsen P et al. Hepatology 2010; 51: 1675-1682
- ↑ Kang SH et al .: Aliment Pharmacol Ther 2017; 46: 845-855.
- ↑ Berthold Jany, Tobias Welte: Pleural effusion in adults - causes, diagnosis and therapy. In: Deutsches Ärzteblatt Volume 116, Issue 21/2019, May 24, 2019, pp. 377–386, here: pp. 379 and 382.
- ↑ Dtsch med Wochenschr 2015; 140 (20): 1514-1516
- ↑ Vilstrup H et al., “Hepatic Encephalopathy in Chronic Liver Disease”, J Hepatol 2014; 61 (3) 642-59
- ↑ Zhan T, Stremmel W. “The diagnosis and treatment of minimal hepatic encephalopathy”, Dtsch Ärztebl. Int 2012; 109 (10): 180-7 doi: 10.3238 / arztebl.2012.0180
- ↑ Amir M. Nia, Stefan Ederer, Kristina M. Dahlem, Natig Gassanov, Fikret Er: Terry's nails: a window to systemic diseases . In: The American Journal of Medicine . tape 124 , no. 7 . Elsevier, July 2011, p. 602-604 , doi : 10.1016 / j.amjmed.2010.11.033 , PMID 21683827 .
- ↑ a b c d e Hans Konrad Biesalski, Stephan Bischoff, Christoph Puchstein: Nutritional medicine . 4th, completely revised and expanded edition. Georg Thieme, Stuttgart 2010, ISBN 978-3-13-100294-5 , p. 674 f .
- ^ Bass NM et al. N Engl J Med 2010; 362 (12): 1071-81
- ↑ Archives of Internal Medicine , June 12, 2006: Coffee, Cirrhosis, and Transaminase Enzymes
- ↑ C Taguchi et al .: Estimated Dietary Polyphenol Intake and Major Food and Beverage Sources among Elderly Japanese . In: Nutrients , 2015, 7 (12), pp. 10269-10281; doi: 10.3390 / nu7125530
- ↑ Christian Müller: Liver and risk of surgery . In: Journal for Gastroenterological and Hepatological Diseases. Journal of diseases of the digestive tract . tape 2 , no. 2 . Krause & Pachernegger, 2004, ISSN 1728-6263 , p. 36–39 ( kup.at [PDF]).