Ontogenetic development of the teeth

The ontogenetic development of teeth is a complex process in which teeth arise from embryonic cells , grow and emerge in the mouth . Many vertebrates have teeth and their development in humans and other living things is very similar. Thus human teeth have a healthy oral environment must be during embryogenesis enamel , dentin , cementum and periodontal ligament develop (periodontal). The primary teeth are created from the sixth to eighth week before the birth, the permanent teeth in the twentieth week. If the teeth do not begin to develop around this time, it will not take place at all. It is generally believed that a factor in the tissue of the first gill arch is necessary to initiate the process.
overview
The tooth bud is a collection of cells from which a tooth can be formed. These cells come from the ectoderm of the first branchial arch and the ecto mesenchyma of the neural crest. The tooth bud is made up of three parts: the enamel organ, the dental papilla, and the dental follicle.
The enamel organ ( Organon enameleum ) consists of an outer and inner enamel ( epithelium enameleum externum and internum ), the Schmelzretikulum ( Recticulum enameleum ) and the intermediate layer ( stratum intermedium ). The cells of the inner enamel epithelium differentiate into ameloblasts , which produce tooth enamel prisms and thus an enamel coating over the dentin . The place where the outer and inner enamel epithelium unite is called the ansa cervicalis . The growth of the cervical cells of the enamel epithelium into deeper tissue forms the Hertwig epithelial sheath , which determines the later shape of the tooth root.
The dental papilla contains cells that develop into the dentin-forming odontoblasts . The connection between the papilla and the inner epithelium determines the shape of the tooth crown. Mesenchymal cells in the papilla are responsible for the formation of the tooth pulp .
The dental follicle creates three important tissues: cementoblasts , osteoblasts, and fibroblasts . Cementoblasts form the root cement, osteoblasts the tooth socket (alveoli) around the tooth root and fibroblasts the periodontal ligaments that connect the tooth with the alveoli through the root cement .
Timeline
The following tables show the development of human teeth over time. The information for the first calcification of the deciduous teeth relates to the times before birth.
Legend to the tables:
- W = weeks
- M = months
- J = years
| central incisor |
lateral incisor |
canine | first molar |
second molar |
||||
|---|---|---|---|---|---|---|---|---|
| Teeth in the upper jaw | ||||||||
| first calcification | 14 W. | 16 W | 17 W. | 15.5 W | 19 W | |||
| Crown complete | 1.5 M. | 2.5 M. | 9 M. | 6 M. | 11 M. | |||
| Root completely | 1.5 y | 2 y | 3.25 y | 2.5 y | 3 y | |||
| Teeth in the lower jaw | ||||||||
| first calcification | 14 W. | 16 W | 17 W. | 15.5 W | 18 W | |||
| Crown complete | 2.5 M. | 3 M. | 9 M. | 5.5 M. | 10 M. | |||
| Root completely | 1.5 y | 1.5 y | 3.25 y | 2.5 y | 3 y | |||
| central incisor |
lateral incisor |
canine | first premolar |
second premolar |
first molar |
second molar |
third molar |
|
|---|---|---|---|---|---|---|---|---|
| Teeth in the upper jaw | ||||||||
| first calcification | 3-4 sts | 10-12 sts | 4-5 sts | 1.5-1.75 yrs | 2-2.25 yrs | at birth | 2.5-3 y | 7-9 y |
| Crown complete | 4-5 y | 4-5 y | 6-7 y | 5-6 y | 6-7 y | 2.5-3 y | 7-8 y | 12-16 y |
| Root completely | 10 y | 11 y | 13-15 y | 12-13 y | 12-14 y | 9-10 y | 14-16 y | 18-25 y |
| Teeth in the lower jaw | ||||||||
| first calcification | 3-4 sts | 3-4 sts | 4-5 sts | 1.5-2 y | 2.25-2.5 years | at birth | 2.5-3 y | 8-10 y |
| Crown complete | 4-5 y | 4-5 y | 6-7 y | 5-6 y | 6-7 y | 2.5-3 y | 7-8 y | 12-16 y |
| Root completely | 9 y | 10 y | 12-14 y | 12-13 y | 13-14 y | 9-10 y | 14-15 y | 18-25 y |
- Graphical representation of the calcification and decalcification times
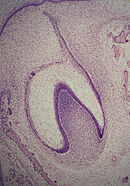
Development of the tooth bud
One of the first steps in the formation of a tooth is the separation of the vestibular and dental lamina . The dental lamina connects the tooth bud with the epithelial layer in the mouth for a certain period of time.
A distinction is made between the following stages in the development of teeth: bud, cap, bell and maturity. The division is the attempt to categorize continuously occurring changes; the exact assignment is often difficult in individual cases (Cate 1998: 81). The determination is made more difficult by various histological sections.
Bud stage
This section is characterized by the appearance of the tooth bud without a clear arrangement of cells. Technically, the stage begins when epithelial cells into ecto mesenchyme penetrate the jaw (Cate 1998: 82). The tooth bud itself is the group of cells at the end of the dental lamina.
Cap stage
The first signs of an arrangement of cells in the tooth bud are at the cap stage. A small group of ectomesenchymal cells stop producing extracellular substances, which leads to the formation of the dental papilla. At this time, the tooth bud grows around the ectomesenchymal arrangement, takes the shape of a cap and becomes the enamel organ. A precipitate of ectomesenchymal cells, called dental follicles, surrounds the enamel organ and delimits the papilla. The enamel organ ultimately produces the enamel, the papilla the dentin and the follicle all supporting structures of a tooth (Cate 1998: 84).
Bell stage
Another differentiation takes place in the bell stage. In this phase, the enamel organ has the shape of a bell and most cells are called "star-shaped reticulum" because of their star-shaped appearance (Cate 1998: 84). The cells on the periphery of the tooth enamel organ divide into three important layers. The cells on the outside are called the outer enamel epithelium. The cells on the dental papilla form the inner epithelium. The cells between the inner epithelium and the enamel reticulum form a layer called the intermediate layer ( stratum intermedium ).
The dental lamina disintegrates, as a result of which the resulting tooth is completely separated from the epithelium of the mouth; the two only connect again when the tooth emerges in the mouth (Cate 1998: 87). The crown of the tooth, which is influenced by the shape of the inner epithelium, takes its shape during this stage. All teeth go through this process; why they form differently shaped crowns (e.g. incisors versus canines) is still unclear. Two hypotheses dominate. One theory is that in the ectomesenchyme there are components for each shape during development. The components for a particular type (e.g. incisors) are localized in one area and quickly broken down in other parts of the mouth. The other model is that the epithelium programs a group of ectomesenchymal cells to produce teeth of a specific shape. This group of cells (clone) stimulates the dental lamina to form a tooth bud. The growth of the lamina continues in a "zone of progress". Once this zone has moved far enough from the first tooth bud, a second bud will develop. The two hypotheses are not necessarily mutually exclusive. Dentistry assumes that both models influence development at certain times (Cate 1998: 89).
In this phase, enamel nodes, ropes and niches can also appear (Cate 1998: 86).
Crown stage
Solid tissues, including tooth enamel and dentin, develop in the next stage called the crown (or maturity) stage. Important cellular changes take place at this time. The rapid division of the epithelial cells ( mitosis ), which in earlier phases led to the enlargement of the tooth bud, now ends at the point where the tips of the teeth form. This is where the first solid, mineralized tissues emerge . At the same time, the cells of the inner epithelium change their shape from cubic to columnar. The cell nuclei move from the papilla closer to the stratum intermedium (Cate 1998: 95).
The neighboring cell layers of the papilla suddenly grow and differentiate into odontoblasts, which form the dentin (Ross 2003: 444). The odontoblasts would not arise without the change in the inner epithelium. They secrete a secretion , an organic matrix, into their immediate surroundings. The matrix contains the material necessary for the formation of the dentin. The odontoblasts migrate to the center of the papilla. In contrast to tooth enamel, the formation of dentin runs from the outside in. Cytoplasmic cantilevers remain on the way in. The unique, tubular appearance of dentin under the microscope is a result of its formation around these cantilevers (Cate 1998: 95).
The cells of the inner epithelium secrete an organic matrix against the dentin, which immediately mineralizes and becomes tooth enamel. Outside the dentin there are ameloblasts that continue the formation of the enamel outwards, so that new material is added on the outside of the emerging tooth.
Formation of firm tissue
Enamel
The formation of tooth enamel, also called amelogenesis , occurs during the crown stage. The formation of dentin and tooth enamel is characterized by reciprocal induction; Dentin always arises before tooth enamel. The latter forms in two phases. In the secretory phase, proteins and an organic matrix form partially mineralized tooth enamel; in the maturation phase, mineralization is completed. (Cate 1998: 197)
The mineralization in the first phase is carried out by the enzyme alkaline phosphatase . (Ross 2003: 445) The mineralized tissue, which usually appears in the third or fourth month of pregnancy , represents the first appearance of tooth enamel in the body, which then spreads outwards.
During the ripening phase, the ameloblasts transport some of the substances used in the production of tooth enamel outside. These are mainly proteins that are used for full mineralization at the end of this stage. The most important proteins are amelogenin, ameloblastin, enamelin and tuftelin. (Ross 2003: 447)
Dentine
The formation of dentin, known as dentinogenesis , is the first recognizable feature in the crown stage. The different stages lead to different types of dentin: Mantle dentin ( Korff dentin ) as well as primary, secondary and tertiary dentin.
The dentin-forming odontoblasts differentiate themselves from the cells of the dental papilla. They begin to secrete an organic matrix around the future tip of the tooth near the inner epithelium. This matrix contains collagen fibers with a large diameter of 0.1-0.2 μm . (Cate 1998: 136) The odontoblasts move towards the center of the tooth and form an offshoot that is known as the odontoblastic process. (Cate 1998: 95) This leads to the secretion of hydroxyapatite crystals and to the mineralization of the matrix. The approximately 150 μm thick layer is the coat dentine. (Cate 1998: 138)
While the mantle dentine arises from an already existing basic substance of the dental papilla, the primary dentine develops in a different way. The odontoblasts become so large that no extracellular resources can contribute to an organic matrix. The larger odontoblasts secrete the collagen in smaller quantities, creating more clearly structured, heterogeneous nuclei. In addition, other substances such as lipids , phosphoproteins and phospholipids are secreted. (Cate 1998: 139)
The secondary dentin is formed - much more slowly - after the root formation is complete. Development takes place faster near the crown than elsewhere on the tooth. (Summit 2001: 13) It lasts throughout life and is responsible for the smaller pulp in older people. (Cate 1998: 128) Tertiary dentine (also known as repairing dentine) is created in response to stimuli such as chewing or dental caries . (Summit 2001: 183)
Tooth germ
Tooth germ is the development stage with an already existing tooth crown but not yet formed tooth root. The surgical removal of a tooth germ is called germectomy .
Root cement
The formation of the cementum , known as cementogenesis , occurs late in the development of the teeth. Cementoblasts are the cells responsible for this. There are two types of root cement: cellular and acellular.
The acellular variant forms first. The cementoblasts differentiate from follicle cells, which can only reach the surface of the tooth root when the Hertwig's epithelial sheath ("Hertwig's Epithelial Root Sheath" - HERS) begins to decay. The cementoblasts secrete fine collagen fibrils at right angles to the root surface before moving away from the tooth. More collagen is deposited along the way to elongate and thicken the fiber bundles. Other proteins such as bone sialoprotein and osteocalcin are also secreted. (Cate 1998: 236) The acellular root cement contains a secretion matrix made of proteins and fibers. When mineralization begins, the cementoblasts move away from the root cement and the fibers that remain on the surface attach to the periodontal ligaments.
The cellular root cement is created when the tooth formation is almost complete and the tooth closes (in contact) with an opposing tooth. (Cate 1998: 241) It forms around the fiber bundles of the periodontal ligaments. The cementoblasts become trapped in the root cement they produce.
The origin of the cementoblasts is different for both types of root cement. The most common hypothesis states that the cells for the cellular root cement come from the neighboring bone, while the cells for the acellular variety come from the dental follicle (Cate 1998: 241 and 243). However, cellular root cement is not found in teeth with one root (Cate 1998: 241). In premolars and molars, it is only found near the tip of the root and between the individual roots.
Formation of the periodontium
The periodontium , the supporting structure of a tooth, consists of the root cement, periodontal ligaments, gums, and alveolar bone. Of these, only the root cement is part of the tooth. The bone surrounds the roots to support them and form a kind of base. The periodontal ligaments connect the bone to the root cement, and the gums are the surrounding tissue visible in the mouth.
Periodontal ligaments
The periodontal ligaments arise from cells in the dental follicles. There are differences between deciduous teeth and permanent teeth as well as in different animal species. (Cate 1998: 245) Anyway, the process begins with fibroblasts from the dental follicle, which secrete collagen, which interacts with the fibers on the surface of the adjacent bones and the root cement. (Ross 2003: 453) This creates an appendix that develops when the tooth protrudes in the mouth. The occlusion continuously affects the formation of the periodontal ligament, resulting in (horizontal or oblique) to the formation of fiber bundles in various alignment. (Cate 1998: 245)
Alveolar bone
When the root and root cement are formed, bone is formed in the area. Bone-forming cells are known throughout the body as osteoblasts . In alveolar bone, these cells come from the dental follicle. (Cate 1998: 244) Similar to the formation of the primary root cement, collagen fibers arise on the surface near the tooth and remain there until they connect with the periodontal ligaments.
Like any other bone in the human body, alveolar bone changes throughout life. Osteoblasts create bones and osteoclasts destroy them, especially when pressure is put on a tooth. (Ross 2003: 452) If, as in the attempt to move the teeth through orthodontics , a tooth exerts a compressive force on the bone below, one reaches a high osteoclastic level, which leads to bone resorption . A bone that is put under tension by periodontal ligaments has many osteoblasts that form new bone.
Gums (gingiva)
The connection between the gums and the tooth is called the dentogingival connection. A distinction is made between gingival, sulcular and connecting epithelium. They are formed from the cells of the epithelial cuff between the tooth and the mouth. (Cate 1998: 247f.)
There are still many unanswered questions regarding the origin of the gums, but it is known that hemidesmosomes between the gingival epithelium and the tooth are responsible for the primary epithelial connection. (Cate 1998: 248) They anchor the cells through small fiber-like structures that represent the remains of ameloblasts. As soon as that happens, the connecting epithelium forms from the reduced enamel epithelium, a product of the enamel organ, and divides quickly. That makes this layer grow quickly. The ameloblasts are no longer supplied with nutrients and stunted, which leads to the formation of a gingival sulcus .
Formation of nerves and vessels
Nerves and blood vessels often run parallel to each other in the body, and they are also formed simultaneously and in a similar way. However, this does not apply in the area around the tooth, where development takes place differently. (Cate 1998: 93)
Formation of nerves
Axons approach the tooth during the cap stage and grow towards the dental follicles. Once there, the nerves develop around the tooth bud and invade the papilla once dentin has started to form. However, they do not grow into the enamel organ. (Cate 1998: 93)
Formation of vessels
Blood vessels grow in the dental follicle and invade the papilla during the capping stage. (Cate 1998: 93) Groups of blood vessels form at the entrance to the papilla. Their number reaches a maximum at the beginning of the crown stage and the papilla becomes the pulp of the tooth. In the course of life, the pulp tissue in the tooth decreases, which is why the blood supply to the tooth decreases with age. (Ross 2003: 452) Due to its epithelial origin, the gum organ is free of blood vessels and the mineralized tissues of the tooth enamel and dentine do not require any nutrients from the blood.
Protrusion of the tooth
Although researchers agree that tooth protrusion ( tooth eruption ) is a complex process, they still argue about the mechanisms that control the process. (Riolo 2003: 142) Some common theories have already been refuted. The tooth is not pushed into the mouth by the growing root or the growing bone. It is also not pushed upwards by pressure from the vessels or a “padded hammock”. (Harris 2002: 1-3) The latter theory presented by Harry Safe was taught from the 1930s to the 1950s. According to this, a band under the tooth, which Safely observed on a histological section under the microscope, was responsible for the protrusion. However, the "tape" was later identified as an artifact that was created in preparation for the cut. (Harris 2002: 3)
According to the most widespread theory today, the periodontal ligaments provide the main impetus in this process. They make the tooth protrude by shrinking their collagen fibers and connecting across them as the fibroblasts contract. (Harris 2002: 5)
When the timing of teeth emergence is different for each individual, there is a general timeline. Humans typically have 20 primary teeth and 32 permanent teeth. In the dentition of the deciduous teeth only the primary teeth are visible. When the first permanent teeth appear, the mixed dentition takes place. When the last milk teeth fall out (exfoliation), one speaks of permanent dentition.
Primary dentition begins with the appearance of the central incisors in the lower jaw (at eight months of age) and continues until the first permanent molars appear at six years of age. (Ash & Nelson 2003: 38,41) The milk teeth usually appear in the following order:
- central incisors
- lateral incisors
- first molar
- canine
- second molar
(Ash & Nelson 2003: 38)
In general, four teeth appear in six months, the teeth in the lower jaw appear earlier than in the upper jaw, and that the process takes place earlier in female individuals than in males. During primary dentition, the tooth buds of the permanent teeth develop under the milk teeth, near the palate or tongue .
Mixed dentition begins with the appearance of the first permanent molar (at the age of six) and lasts until the last deciduous tooth falls out at eleven or twelve years of age. (Ash & Nelson 2003: 41) The permanent teeth in the upper jaw appear in a different order than the teeth in the lower jaw.
| upper jaw | Lower jaw |
|---|---|
| first molar | first molar |
| central incisor | central incisor |
| lateral incisor | lateral incisor |
| first premolar | canine |
| second premolar | first premolar |
| canine | second premolar |
| second molar | second molar |
| third molar | third molar |
Since there are no premolars in primary dentition, the molars of the deciduous dentition are replaced by permanent premolars. If milk teeth fall out before permanent teeth are available to replace, permanent teeth can slip forward, which means that space for more teeth is lost in the mouth. This can lead to deformities lead ( malocclusion ), which is a orthodontic treatment may require a eugnathes teeth to produce.
Permanent dentition begins with the loss of the last milk tooth between the ages of 11 and 12. As a result, the third molars ( wisdom teeth ) are often removed due to carious destruction or eruption problems due to lack of space . The most common reasons for tooth loss are carious destruction or periodontal disease .
| Times when the teeth stick out | ||||||||
|---|---|---|---|---|---|---|---|---|
| central incisor |
lateral incisor |
canine | first premolar |
second premolar |
first molar |
second molar |
third molar |
|
| Milk teeth | ||||||||
| upper jaw | 10 M. | 11 M. | 19 M. | 16 M. | 29 M. | |||
| Lower jaw | 8 M. | 13 M. | 20 M. | 16 M. | 27 M. | |||
| permanent teeth | ||||||||
| upper jaw | 7-8 y | 8-9 y | 11-12 y | 10-11 y | 10-12 y | 6-7 y | 12-13 y | 17-21 y |
| Lower jaw | 6-7 y | 7-8 y | 9-10 y | 10-12 y | 11-12 y | 6-7 y | 11-13 y | 17-21 y |
(Ash & Nelson 2003: 53)
M = months; J = years
nutrition
As with other aspects of human growth, diet has an effect on tooth development. Essential nutrients for a healthy tooth include calcium , phosphorus , fluoride , and vitamins A , C and D . Calcium and phosphorus are required for the formation of hydroxyapatite crystals and their proportion in the blood is regulated by vitamin D. Vitamin A is responsible for the formation of keratin and vitamin C for collagen . Fluoride can become part of the crystal in the tooth, making it more resistant to demineralization and tooth decay . (Ross 2003: 453)
A lack of nutrients can have numerous consequences for the development of teeth. If there is a lack of calcium, phosphorus and vitamin D, the solid components of the tooth may be less mineralized. A lack of vitamin A leads to a reduction in tooth enamel. A lack of fluoride accelerates demineralization when the tooth is exposed to an acidic environment and delays re-mineralization. Fluoride overdoses lead to fluorosis , in which white to brown discoloration in the form of spots or streaks forms on the surface of the tooth enamel.
Abnormalities
Various abnormalities can occur in the development of teeth.
With anodontics , tooth development does not take place at all, with hypodontia only partially. Anodontia is rare, most commonly associated with ectodermal dysplasia , while hypodontia is one of the most common abnormalities, affecting 3.5–8.0% of the population (not counting the wisdom teeth). The lack of wisdom teeth can be observed in 20-23% of the population, followed by the second molar tooth ( molar ) and lateral incisor. Hypodontia is often associated with the absence of the dental lamina, which makes it vulnerable to external influences such as infections or chemotherapeutic medications and is associated with some syndromes such as Down's syndrome or Crouzon's disease . (Neville 2002: 70)
With hyperdontia , excess teeth develop. It occurs in one to three percent of Europeans and more frequently in Asians . (Neville 2002: 70) In 86% of the cases, the hyperdontia mostly affects a single additional incisor in the upper jaw. (Kahn 2001: 49) The cause of hyperdontia is assumed to be an excess of dental lamina.
A dilaceration is an abnormal bend to a tooth, which is almost always through a trauma caused by the moved the resulting tooth bud. When it arises, a force can move the tooth from its original position, causing the rest of the tooth to form at an unnatural angle. Cysts or tumors near the tooth bud can also cause dilaceration. Deciduous teeth can also be pushed into the gums by trauma, thereby moving the tooth bud of the permanent tooth. (Neville 2002: 86)
Tooth malformations
The causes of regional odontodysplasia (tooth malformation) are unknown; they are certainly not genetic . A disorder of the development of the mesenchymal and ectodermal structures of the teeth, a disorder in the cells of the neural crest , an infection or a lack of vascular supply are suspected , the latter hypothesis being the most common. A radiation therapy can lead to odontodysplasia. (Neville 2002: 99) Teeth affected by this abnormality can persist, i.e. not erupt, have crowns that are too small and have unnatural shapes. The teeth are smaller, show increased pits and furrows and often have a brown to yellowish discoloration. Radiographically, a large pulp lumen with a thin layer of hard substance can be seen, root growth is delayed, enamel and dentin can hardly be distinguished from one another, and radio opacity is reduced. These teeth often appear transparent and "fluffy" on X-rays, which has earned them the nickname " ghost teeth" .
This must be differentiated from enamel formation disorders such as molar incisor hypomineralization , which can result from trauma , medication, nutrition, birth incidents and numerous acute or chronic childhood diseases or their treatment, although the cause is still largely unknown. This also includes the Turner tooth , whose germ damage to the permanent tooth is caused by diseased milk teeth. The Amelogenesis imperfecta is a genetic disease in which there to a disturbance of enamel formation occurs. Tetracycline teeth are formed by the administration of tetracycline during pregnancy or in childhood, as tetracyclines and calcium are incorporated into the child's tooth enamel in an irreversible complex formation.
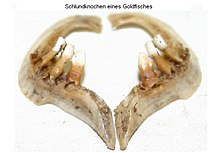
Development of teeth in animals
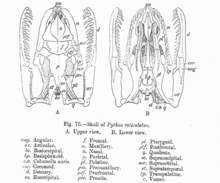
Historically, the teeth of vertebrates are derived from specialized scales of skin ( placoid scales ), which in original vertebrates sometimes cover the entire body and form a kind of exoskeleton.
This can be done e.g. B. can be understood well in the relatively primitive sharks (see cartilaginous fish ), whose tooth formation differs significantly from that of the other vertebrates. Because their teeth have no roots, sharks simply lose teeth when they eat, which must therefore be continuously replaced. Zoologists estimate that a single shark can lose up to 2,400 teeth in a year. Shark teeth are formed from the placoid scales mentioned near the tongue and move outward in rows on the jaw, where they are used and later fall out.
While in mammals , to which humans also belong, the teeth form a row in the upper and lower jaw (there are differences in the morphology, the number, the timeline and the types of teeth), in other vertebrate groups there are sometimes several Rows of teeth in different locations. Certain groups of vertebrates such as B. Birds and turtles have lost their teeth in the course of development. Birds that are derived from the dinosaurs (cf. Archeopteryx ), for example, have not formed any teeth for about 70 million years, but have apparently still partially retained the associated genetic makeup, which under special circumstances, e.g. B. in the context of mutations, can induce tooth formation ( atavism ).
The formation of tooth enamel is almost identical in humans and other mammals. The ameloblasts and the enamel organ including the dental papilla work similarly. (Frandson 1992: 305) While the ameloblasts die in humans and most other animals - which makes further formation of tooth enamel impossible - the development in rabbits , chinchillas and guinea pigs and some teeth of other mammals (" rootless teeth ") continues what makes them wear down their teeth by chewing on various materials. If chewing is not possible, their teeth can poke through the mouth ( pike bite ). The rootless teeth consist of two halves, the counterparts to the crown and root. The half of the lip is covered with enamel and resembles a crown, while the half of the tongue is covered with dentin and resembles a root. Both arise at the same time and grow for a lifetime.
The mineral distribution in rodent tooth enamel differs from that in monkeys , dogs , pigs, and humans. In horse teeth , the enamel and dentin layers are bonded together, which increases the strength and reduces the wear and tear of the teeth.
Even among mammals, some groups of animals, such as B. certain whales, armadillos, anteaters and sloths the formation of tooth enamel (enamelum) or the formation of teeth in general abandoned. This was accompanied by a loss of function of the associated enamelin gene ENAM.
literature
- Major M. Ash, Stanley J. Nelson: Wheeler's Dental Anatomy, Physiology, and Occlusion. 8th edition. 2003, ISBN 0-7216-9382-2 .
- AR Ten Cate: Oral Histology: Development, Structure, and Function. 5th edition. 1998, ISBN 0-8151-2952-1 .
- RD Frandson, TL Spurgeon: Anatomy and Physiology of Farm Animals. 5th edition. Lea & Febiger, Philadelphia 1992, ISBN 0-8121-1435-3 .
- Edward F. Harris: Craniofacial Growth and Development . 2002.
- Michael A. Kahn: Basic Oral and Maxillofacial Pathology . 2001.
- BW Neville et al. a .: Oral & Maxillofacial Pathology. 2nd Edition. 2002, ISBN 0-7216-9003-3 .
- Michael L. Riolo, James K. Avery: Essentials for Orthodontic Practice . 2003, ISBN 0-9720546-0-X .
- Michael H. Ross, Gordon I. Kaye, Wojciech Pawlina: Histology: A text and atlas. 4th edition. 2003, ISBN 0-683-30242-6 .
- James B. Summit, J. William Robbins, Richard S. Schwartz: Fundamentals of Operative Dentistry: A Contemporary Approach. 2nd Edition. Quintessence Publishing, Carol Stream, Illinois 2001, ISBN 0-86715-382-2 .
Web links
- Database with different genes in the emerging tooth
- Integumentary Development Tooth (May 15, 2013 memento on the Internet Archive ) by Mark Hill of the University of New South Wales Embryology Resource
Individual evidence
- ↑ a b c d e f g h i j k l m n o p q r s t u v w x y z A. R. Ten Cate: Oral Histology: development, structure, and function. 5th edition. 1998.
- ↑ a b c d e B. Steiniger, H. Schwarzbach, V. Stachniss: Microscopic anatomy of the teeth and the periodontium. 1st edition. Thieme Verlag, 2010, ISBN 978-3-13-160391-3 .
- ↑ a b c d e f g h Michael H. Ross, Gordon I. Kaye, Wojciech Pawlina: Histology: A text and atlas. 4th edition. 2003.
- ^ A b c d e Major M. Ash, Stanley J. Nelson: Wheeler's Dental Anatomy, Physiology, and Occlusion. 8th edition. 2003.
- ↑ usc.edu
- ↑ a b James B. Summit, J. William Robbins, Richard S. Schwartz: Fundamentals of Operative Dentistry: A Contemporary Approach. 2nd Edition. Quintessence Publishing, Carol Stream IL 2001.
- ^ Clarke Johnson: Biology of the Human Dentition. ( Memento of October 30, 2015 in the Internet Archive ) 1998.
- ↑ a b c d e f A. R. Ten Cate: Oral Histology: Development, Structure, and Function. 5th edition. 1998.
- ↑ Michael L. Riolo, James K. Avery: Essentials for Orthodontic Practice . 2003.
- ^ A b c Edward F. Harris: Craniofacial Growth and Development . 2002.
- ^ Dental Health and Your Child's Teeth . WebMD
- ↑ Exploration of the Month ( Memento of May 18, 2006 in the Internet Archive ) charfac.umn.edu
- ^ Nutritional Factors in Tooth Development and Maintenance
- ^ Table II. Effects of nutrient deficiencies on tooth development
- ↑ a b c d B. W. Neville u. a .: Oral & Maxillofacial Pathology. 2nd Edition. 2002.
- ^ A b Michael A. Kahn: Basic Oral and Maxillofacial Pathology . 2001.
- ↑ ms-starship.com
- ↑ marinebiology.org
- ↑ scientificamerican.com
- ↑ RD Frandson, TL Spurgeon: Anatomy and Physiology of Farm Animals. 5th edition. Lea & Febiger, Philadelphia 1992.
- ↑ T. Caceci: Veterinary Histology, Digestive System: Oral Cavity. ( Memento from April 30, 2006 in the Internet Archive )
- ↑ O. Fejerskov: human dentition and experimental animals. PMID 105027
- ↑ phenomena.nationalgeographic.com
- ↑ phenomena.nationalgeographic.com