Chondrocyte
A chondrocyte (composition of Greek χονδρός chondros , cartilage 'and κντος kytos , cell'), and cartilage cell , is one of chondroblasts emanating and resident of the cartilage cell . Together with the intercellular substances (extracellular matrix), the chondrocytes form the main components of cartilage .
The cartilage cell is the only living part of the cartilage, but only makes up about 1% of the cartilage tissue.
Cartilage growth
Cartilage growth ( chondrogenesis ) can be divided into interstitial growth (growth in length) and appositional growth (growth in thickness).
- Interstitial growth
The cartilage as a whole (like all connective and supporting tissue) is made of mesenchyme . The mesenchymal cells differentiate into rapidly proliferating chondroblasts . These form a cartilage matrix, which, as long as it is still soft, allows the newly formed chondroblasts to move away from each other and continue to divide ( interstitial growth ). With the completion of the interstitial cartilage growth and maturation of the matrix, the cartilage cells that emerged from the last cell divisions remain together in so-called isogenic groups and become chondrocytes that are no longer able to divide.
- Appositional growth
On the surface of the cartilage, the connective tissue cartilage skin, the perichondrium, is formed from the mesenchyme, from the innermost layer of which cells differentiate into chondroblasts, form a matrix and thus ensure appositional growth .
construction
Specific properties
Whether a division and grouping takes place, what the basic substance consists of and what properties the cartilage formed has, depends on the respective type of cartilage or the location of its occurrence.
A distinction is made between the following:
- Hyaline cartilage (e.g. costal cartilage, articular cartilage, tracheal cartilage, nasal cartilage, larynx: cartilago thyroidea, cartilago cricoidea)
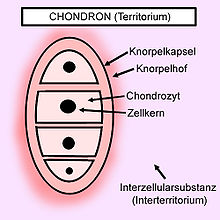
The hyaline cartilage is the most common type of cartilage. At the edge of the hyaline tissue, the chondrocytes have an elliptical shape, with the longitudinal axis running parallel to the cartilage surface - the cartilage cavity is separated from the environment by collagen fibers (type II). Inside the cartilage, they are rounded with finger-shaped appendages and occur in groups of up to 8/10 cells, which are formed from a single cell by division ( isogenic groups ). Several cartilage cavities are also combined into functional units, the chondrons , by collagen fibers . These are pressure-elastic.
A chondron is surrounded by a territorial matrix ( cartilage halo, cell halo).
Fibers running between the chondrons attach the cell structure to the perichondrium or to the bone. Chondronectin promotes the adhesion of chondrocytes to collagen.
- Elastic cartilage (e.g. ear cartilage, larynx: cartilago epiglottica)
The elastic cartilage is rarely found and initially resembles hyaline cartilage. Chondrocytes can occur here individually or in small groups, they are elastic and the cartilage cavity is also separated from the environment by collagen fibers (type II). The chondrons here have one or two, at most three, large chondrocytes. A single chondrocyte is surrounded by a pericellular matrix ( cartilage capsule).
- Fiber cartilage (e.g. symphysis pubica, discus intervertebralis, articular cartilage: temporomandibular joint)
The less elastic chondrocytes of the fibrous cartilage are organized in small groups, but are predominantly found individually in the matrix. They are elongated and are delimited by both Type I and Type II collagen fibers , with Type I dominating in terms of quantity. Proteoglycans only occur in low concentrations here; a perichondrium is missing.
Nonspecific properties
They are embedded in the extracellular matrix they form and are located there in small cavities (lacunae). In addition, they show little metabolic activity ( bradytrophic tissue).
As an expression of their high synthesis performance, they have a well-developed Golgi apparatus and abundant rough endoplasmic reticulum . The structure of the cell is maintained by the vimentin filaments that run through the cytoplasm like a network .
The chondrocytes are supplied by diffusion from the capillaries of the perichondrium , in the case of articular cartilage (which, as an exception, has no perichondrium) through the synovial fluid . Cartilage has no lymphatic vessels and nerves.
Chondrocytes can be isolated and cultured. Corresponding cultures, fixed on carrier material, are used for cartilage regeneration.
function
Chondrocytes belong to the fixed connective tissue cells (fibrocytes, reticular cells, osteocytes, ...) and basically fulfill the function of secretion and mechanical stability. They do not communicate with other cells and are particularly responsible for the formation of the extracellular matrix of the cartilage tissue.
The synthesis of protein, RNA and DNA as well as cell proliferation and the uptake of amino acids are stimulated in the chondrocytes.
The activity of the chondrocytes is increased by thyroxine and testosterone and inhibited by cortisone , hydrocortisone (cortisol) and estradiol .
Diseases
The best-known chondrocyte disease is osteoarthritis . This leads to non-inflammatory, degenerative joint damage and very severe pain. In this disease, the extracellular matrix proteins of the cartilage are broken down by proteases; the exact causes are still largely unclear.
Smaller cartilage defects can be treated with subchondral abrasion arthroplasty . The damaged articular cartilage and the underlying bone tissue are removed. In procedures that open the medullary cavity, the cartilage defect and subchondral bone are drilled so deep that a connection to the bone marrow is created. This allows pluripotent cells to migrate into the effect and form a replacement fiber cartilage. In the case of the Pridie drilling , this connection is achieved through boreholes; in the case of microfracturing , this connection is achieved with a ram. One treatment method for the treatment of cartilage defects is the autologous chondrocyte transplant . With the help of an arthroscopy , chondrocytes are taken from healthy areas. These cells are then enzymatically isolated and multiplied in the laboratory (about three to four weeks) and then used again. After a few weeks, when the chondocytes have integrated, the patient can move freely again. The advantage of this method is that the risk of rejection is low, because the implanted cartilage cells come from the patient's own cells. The method is mainly used for cartilage defects in the knee joint up to a size of 10 cm 2 or when other cartilage repair procedures have failed. Chondrocyte transplantation does not play a role in restoring the knrople coating in osteoarthritis. There are other methods of treating cartilage defects called cell-free methods. Instead of cells, only a membrane with hyaluronic acid is used on the defect. Some clinical studies have shown that hyaluronic acid helps regenerate cartilage tissue.
The achondroplasia is a common mutation that affects the growth of the skeletal system. The result is disproportionate dwarfism with a relatively long trunk and rhizomelic shortening (shortening of the middle extremity regions) of the plump limbs, due to a predominantly quantitative disruption of the enchondral bone growth. The disease is autosomal - dominant inherited. As a result of the mutation, the cartilage cell receptor for the fibroblast growth factor -3 (FGFR-3) is not sufficiently expressed , which leads to a disruption of the chondrocyte proliferation and differentiation in the growth plate, which in turn leads to a disruption of the enchondral ossification.
Web links
- Functional anatomy of the articular cartilage - a literature study (PDF; 5.9 MB) - scientific work hosted at the University of Munich (LMU)
Individual evidence
- ↑ Arthrose therapy directory - an independent inventory / German Arthrosis Forum - at arthrose-therapie-verzeichnis.de
- ↑ Entry on appositional growth in Flexikon , a wiki from DocCheck , accessed on November 25, 2015.
- ↑ a b c d e Michaela Hartmann, Maria Anna Pabst, Gottfried Dohr: Cytology, Histology and Microscopic Anatomy: Light and electron microscopic image atlas . Facultas; Edition: 5th, revised edition. (December 2010), ISBN 3-7089-0682-9 , page 38/39
- ↑ a b c Theodor H. Schiebler, Horst-W. Korf: Anatomy: histology, history of development, macroscopic and microscopic anatomy, topography . Steinkopff; Edition: 10th, completely revised. Edition (September 21, 2007), ISBN 3-7985-1770-3 , p. 47 ff.
- ^ Luiz Carlos Junqueira (author), José Carneiro (author), Manfred Gratzl (ed.): Histologie: Neue Approbationsordnung . Springer, Berlin; Edition: 6th, newly translated. revised A. (September 15, 2004). ISBN 3-540-21965-X , p. 82.
- ^ Luiz Carlos Junqueira (author), José Carneiro (author), Manfred Gratzl (ed.): Histologie: Neue Approbationsordnung . Springer, Berlin; Edition: 6th, newly translated. revised A. (September 15, 2004). ISBN 3-540-21965-X , pp. 82/83.
- ↑ Chondrocyte - definition in the Roche Lexicon of Medicine at tk.de.
- ^ Rainer Klinke (author), Hans-Christian Pape (author), Armin Kurtz (author), Stefan Silbernagl (author): Physiology: Textbook . Thieme, Stuttgart; Edition: 6th completely revised edition. (November 18, 2009), ISBN 3-13-796006-1 , p. 531.
- ↑ AG Prof. Shakibaei - presentation of research projects, hosted at the University of Munich
- ^ A b Hanns-Peter Scharf et al .: Orthopedics and trauma surgery: specialist knowledge according to the new training regulations . 2nd Edition. Elsevier, Urban & Fischer, 2011, ISBN 978-3-437-59455-7 , pp. 32 .
- ↑ Hanns-Peter Scharf et al .: Orthopedics and trauma surgery: specialist knowledge according to the new training regulations . 2nd Edition. Elsevier, Urban & Fischer, 2011, ISBN 978-3-437-59455-7 , pp. 31 .
- ↑ Hanns-Peter Scharf et al .: Orthopedics and trauma surgery: specialist knowledge according to the new training regulations . 2nd Edition. Elsevier, Urban & Fischer, 2011, ISBN 978-3-437-59455-7 , pp. 33 .
- ↑ Hanns-Peter Scharf et al .: Orthopedics and trauma surgery: specialist knowledge according to the new training regulations . 2nd Edition. Elsevier, Urban & Fischer, 2011, ISBN 978-3-437-59455-7 , pp. 33-34 .
- ↑ A. Siclari, G. Mascaro, C. Gentili, R. Cancedda, E. Boux: A cell-free scaffold-based cartilage repair Provides improved function hyaline-like repair at one year. In: Clinical orthopedics and related research. Volume 470, number 3, March 2012, pp. 910-919, doi: 10.1007 / s11999-011-2107-4 , PMID 21965060 , PMC 3270167 (free full text).
- ↑ DM Ornitz, L. Legeai-Mallet: achondroplasia: Development, pathogenesis, and therapy. In: Developmental Dynamics . Volume 246, number 4, 04 2017, pp. 291-309, doi: 10.1002 / dvdy.24479 , PMID 27987249 , PMC 5354942 (free full text) (review).

