Laser in situ keratomileusis
The Lasik ( LASIK ) is a eye surgery with the excimer laser for correction of optical vision defects , in contrast to the Photo refractive keratectomy (PRK) is not (in-situ) at the surface, but only in the inner part of the cornea (Stroma), but its optical effect unfolds on the surface of the cornea. After weighing the advantages and disadvantages as well as the risks inherent in the system, it is an alternative to eliminating the ametropia through glasses or contact lenses . The procedure is currently the most common method in refractive surgery .
Basics
This laser method, which has been used since 1990, changes the curvature of the cornea by removing tissue from the cornea. Tissue removal in the cornea is made possible by cutting and opening a lamella, the so-called flap. A LASIK patient has sharp vision very quickly and relatively painlessly, as the operation is carried out under the pain-sensitive corneal surface and the epithelium , in contrast to surface treatments ( PRK , Trans-PRK ), does not have to grow back first. However, the operation- related corneal incision ( flap ) results in a different risk potential than with the superficial PRK.
LASIK offers the chance to correct the broadest spectrum of ametropia from nearsightedness (up to -10Dpt), farsightedness (up to + 4Dpt) and astigmatism (up to -5Dpt), but usually also represents a surgical procedure on a principally healthy organ. In the best case, the remaining refractive error is less than ± 0.5 diopters and the patient can usually live without visual aids (glasses, contact lenses). The uncorrected visual acuity , i.e. H. unaided visual acuity usually improves dramatically, ideally reaching 1.0 or more. The best corrected visual acuity (visual acuity with optimal eyeglass correction), on the other hand, remains mostly unchanged or changes slightly (depending on the treatment method).
Historical development of refractive surgery
Years of Radial Keratotomy (RK)
The operation on an organically healthy eye, which only needs a visual aid, i.e. glasses or contact lenses, in order to see clearly without them, was not an innovation that the university professors brought about. It was the pioneering deeds of "single perpetrators" of practical applied ophthalmology, who were often driven by their own handicap of being dependent on glasses, to find a scientifically based solution for themselves to eliminate ametropia. The first publication on this topic is probably the report by the Norwegian ophthalmologist Hjmar Schiotz , written in the then dominant scientific language of German, in 1885, who reported in the archives of ophthalmology about the surgical correction of extreme astigmatism through cleverly chosen corneal incisions. The Japanese ophthalmologist Tsutomu Satō took up this concept of changing the refractive power of the cornea through corneal incisions, only to leave it to the Russian ophthalmologist Svyatoslav Fyodorov after a series of disappointing operations at the end of the 1940s to use the method of radial keratomy through an overwhelming number of operations to perfect that, with the help of the nomograms he developed , it was possible to achieve somewhat predictable changes in refractive power through cutting depth, length and position of the cuts, ideally even freedom from glasses and contact lenses. This method was later implemented by Theo Seiler during the first eye laser treatment with the excimer laser . However, the corneal scars produced by the corneal incisions proved to be disadvantageous, which often reached close to the center of the optically effective visual axis and, especially at night with a wide pupil, led to considerable scattering and glare effects. It also soon became clear that patients operated on with radial keratotomy had to accept fluctuations in visual acuity during the day, as well as a tendency towards progressive farsightedness , which, especially in old age, increased presbyopia and thus the need for reading glasses. The RK has led to widespread use, particularly in the USA.
LASIK pioneering days
At almost the same time, the Spanish ophthalmologist José Ignacio Barraquer in Colombia developed a surgical method to transform the optical refractive powers of the cornea by plane-parallel splitting of the cornea and intrastromal changes: the so-called keratomileusis (ancient Greek Κερατων cornea; Μιλευσισ shaping). At that time there was no formal training in refractive surgery at any university, but the pioneers ordered this newly emerging field of ophthalmology through self-study, self-organized workshops, clinical experimental procedures, meetings at small satellite congresses of larger conferences of the specialist group or personal tutorials . Since instruments such as microsurgical instruments for processing the cornea, such as keratomas , calibratable corneal knives , and later also the excimer lasers were freely available for sale by the industry that was flourishing in this sector, the unregulated training for refractive eye surgeons caused systemic complications from the early days to the partly justified reputation Refractive eye surgery is extremely dangerous. A split in ophthalmology didctrine developed very early on, whereby one group recognized the future potential of these operations and saw the basis for a legitimate surgical intervention in the existing scientific knowledge, while the other group assessed it as a violation of professional ethics Eye that achieved the best-corrected visual acuity through glasses or contact lenses to carry out "unnecessary" surgical interventions. As early as 1995, under the leadership of ophthalmologist Michael Knorz (Mannheim), the Refractive Surgery Commission (KRC) was founded in Germany , a merger of the German Ophthalmological Society (DOG) and the Professional Association of Ophthalmologists in Germany (BVA), which regulates the Training as a laser doctor, offering annual certification training and since then has published recommendations on the indication and contraindication of refractive surgery based on the latest scientific findings. On September 21, 2007, NASA's team of ophthalmologists led by Steven Schallhorn announced that Femto-LASIK could be judged to be so safe that this operation could also be approved for astronauts.
International cooperation
In the early 1990s, there was an international spirit of optimism in refractive corneal surgery supported by the excimer laser (EXCIted dIMer LasER). Steven Trokel from Columbia State University / New York as clinician, John Marshall from Moorfield's Eye Hospital, London as histopathologist and Charles Munnerlyn (USA) as physicist laid the foundations for the laser technology application of the excimer laser and its interaction with the cornea. The previous decade was dominated by mechanical cutting techniques of the cornea such as radial keratotomy / RK by SN Fyodorowin of the USSR, the automatic lamellar keratotomy / ALK by Luis Ruis in Colombia, by Jörg Krumeich in Bochum / Germany or, since 1982, the excimer laser (supported) - Radial keratotomy (RK) by Theo Seiler in Germany. The use of the excimer laser developed by IBM for the production of computer circuit boards promised the necessary exponential increase in precision into the micrometer range in order to be able to accurately change the refractive power of the cornea (approx. 15 µm ≈ 1 D). The ablation algorithms developed by Charles Munnerlyn on the animal model represent the principles of excimer laser programming that are still valid today. Patent disputes between two American founding companies, SUMMIT and VISX, continued to occupy the American courts for years and ended with a million dollar settlement for Steven Trokel and the merger of the two founding companies (personal communication Marguerite McDonald). The first photorefractive keratectomy (PRK) performed worldwide on a seeing human eye was carried out by Marguerite McDonald on March 25, 1988 in New Orleans / USA. This eye was made available by a patient to science for this experiment because it had to be removed because of a malignant melanoma. This historical treatment can be seen as the first clinical evidence that was able to confirm the procedure developed on the animal model for changing the refractive power of the eye by means of PRK in humans.
The years marked by PRK (photorefractive keratectomy)
The approval studies submitted to the FDA (Federal Drug Administration / USA) and the unsecured legal situation for first-time laser surgeons in the USA led to a real patient tourism from the USA across the border to Canada to the eye laser pioneers Gordon Balazsi & Marc Mullie in Montreal , who, beginning in 1993, were able to present progress studies on PRK with a large number of patients at international congresses in a short time. The FDA approval in the USA for PRK took place in 1995, that for keratome LASIK in 1998 and led to an extremely rapid increase in treatment centers with the excimer laser in the USA as well. However, the actual innovative steps of refractive laser eye treatment using LASIK took place in less regulated Europe. In 1991 José Güell and colleagues in Barcelona , Joannis Pallikaris in Heraklion / Crete, Lucio Buratto in Milan / Italy, Michael Knorz in Mannheim and Theo Seiler in Dresden / Germany started using the excimer laser to eliminate myopia. Lucio Buratto introduced Steven Slade and Stephen Brint to laser technology who, back in the USA, initiated the approval studies at the FDA (Federal Drug Administration) for the SUMMIT laser. With the exception of the University of Mannheim and Dresden / Germany, which had committed representatives of the newly developing subject in their department heads Michael Knorz and Theo Seiler, other universities were reluctant to intervene on otherwise healthy eyes that were only changed by deviating refractive power. Thomas Neuhann Munich / Germany, who later became an internationally renowned excimer laser doctor, who had completed his habilitation on wound healing through perforating keratoplasty / cornea transplantation, was initially very reserved about the method. In 1992, Wolfgang Pfäffl was given the opportunity to use the excimer laser from the company MEDITEC Erlangen / Germany from Miro Stambuck in Blaubeuren / Germany and founded the VisuMed team with colleagues, which started operations in 1993 in Munich under Wolfgang Pfäffl and Gerold Fiedler and in Cologne under Matthias Maus an excimer laser eye center. One of the most innovative excimer lasers in Germany at that time was the KERACOR 116 developed by Kristian Hohla / Puchheim, of colleagues such as Luis Ruiz (Bogota / Colombia), Michael Knorz (Mannheim / Germany), Wolfgang Pfäffl (Munich / Germany) and Matthias Maus (Cologne / Germany), as well as Gordon Balazsi and Marc Mullie (Montreal / Canada) in a joint effort to improve excimer laser technology. Sinan Goeker (Istanbul / Turkey), who also used the same laser, had the first experimental clinical results of this excimer laser on the human eye, which were necessary for the approval of the device. Due to the problems of PRK such as reduced suitability for night driving, loss of the best corrected visual acuity due to central tissue remnants ("central islands") or corneal scar formation ("haze"), too small optical zones as well as low long-term stability of the laser eye result threatened the laser eye procedure to fall into disrepute in the rainbow press. A new alternative was the keratome LASIK technique developed by Luis Ruiz, which came from Colombia and which was quickly established by Michael Knorz in Mannheim under the protection of university research. Laser eye surgeons from all over Europe now also came to Mannheim to be introduced to the technology by Michael Knorz. Problems such as pain after the operation and "haze" formation have now been replaced by corneal inflammation (diffuse lamellar keratitis), epithelial ingrowth in the corneal "flap" or irregular corneal ablation with the phenomenon of the central one already known from the PRK Tissue island formation in the "broad beam laser profile". Emanuel Rosen (London / UK), who tried to introduce PRK in England together with John Marshall at an early age, found even more reluctance to use modern technology in conservative England than he did in Germany and withdrew from excimer laser treatments during this time. He only started again with eye laser treatments when the more modern “flying spot laser profile” came onto the market under Kristian Hohla in order to avoid the patent dispute with an American laser manufacturer.
The LASIK operation is gaining in importance
In 1995 Wolfgang Pfäffl, inspired by Michael Knorz from Mannheim, who had got to know this technique with Luis Ruis in Bogota, performed his first keratome LASIK. In the same year, Thomas Neuhann, who invited Steven Slade from the USA as a tutor, began to operate in the LASIK technique. The first laser-assisted keratome LASIKs were performed using the “free flap” technique with the “Automated Corneal Shaper” from Ruiz. The cut “flap” was put aside during the excimer laser exposure to the cornea and then returned to the cornea treated by the excimer laser according to the markings previously made. Lucio Buratto (Milan / Italy) relocated the laser ablation to the back of the “flap”, a technique that was unable to establish itself due to technical difficulties. We owe the LASIK technique with the folded-back flap, which is common today, to the more or less accidental discovery of Ioannis Pallikaris Heraklion / Greece, to whom the keratoma got stuck at the end of the incision during a planned "free flap". Since the working area for the laser was large enough, he continued the treatment with the excimer laser and discovered that the corneal cap, the "flap", which was still attached, came to lie much more perfectly on the corneal bed when it still remained connected to the cornea at its hinge. In the period that followed, almost all of the "corneal shapers" available on the market were modified and fitted with a stopper so that Pallikaris' hinge technology could be implemented as planned. This mechanical cutting technique in various variants dominated the eye laser market for over a decade. Because of the possibly greater potential of a wrong cut, a too small “flap” or irregular “flaps” (“buttonhole” “button hole”) through the inserted keratome, which can detach from the eye if suction is lost, this technique was also criticized Laser ophthalmologists who, despite its problems, touted PRK as a safer method, as PRK had also received approval for aviation in the USA. The enthusiasm for the new technique of keratome LASIK seduced the eye laser doctors to laser up to −25 Dpt at the beginning, an indication for refractive corneal surgery, which according to current knowledge would be regarded as malpractice. Michael Knorz published his negative experiences in this regard and as a result the KRC (Commission for Refractive Surgery) in Germany restricted the reliable treatment range to a maximum of -10 Dpt. Major concern arose when the incidence of medically induced keratoconus from corneas that were too thin, either pre-existing or induced by the keratome and laser treatment, was observed.
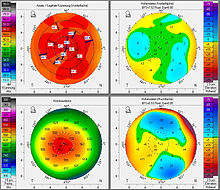
Customized laser eye treatment using wavefront technology
The occurrence of complications after refractive corneal interventions and their elimination sparked the development of new examination methods in the optical industry such as wavefront analysis and optical path measurement for the generation of tailor-made laser treatments, which have been the subject of many refractive-surgical congresses since 1999. Here so-called "higher order aberrations" are reflected from the retina by a "lens array system" consisting of over 100 diagnostic laser beams arranged in grid form. The deviations from the ideal line in the running speed between the individual laser beams are measured and smoothed in a computationally intensive, complex correction program. Excimer laser ablation profiles can be programmed that also significantly improve, if not completely eliminate, decentered corneal treatment zones or optical zones that are too small
The transition from keratome LASIK to femto LASIK
The trend therefore had to lead to more precise and as thin as possible "flaps" in order to be able to leave as much residual thickness as possible on the cornea. That is why the femtosecond LASIK (“femto-LASIK”), which came onto the market in 2004, was quickly adopted. In 2006, at the 24th Congress of the ESCRS ( European Society of Cataract and Refractive Surgery ), John Marshall presented the histologically substantiated advantages of Femto-LASIK and coined the term “SBK-LASIK”. With this technique, all the dangers of the mechanical cutting technique are eliminated, because the corneal cap, the "flap", is created within the tissue through the " photodisruption " of the femto laser, before access to the virtual space between the corneal cap and cornea is made through the edge incision -Bed is possible. The problem here was how to remove the "flap" still connected to the corneal bed via tissue bridges from its base. Parry Binder (Los Angeles / USA), Wolfgang Pfäffl (Munich / Germany) Steven Slade (Houston / USA) and Dan Durrie (Overland Park / USA) were among the first eye laser surgeons to have access to the first clinically applicable femtosecond lasers of the laser Manufacturer IntraLase and intensively and scientifically dealt with the new technology, which presented the laser eye doctor with new operational challenges. Parry Binder, Steven Slade, Dan Durrie and others determined the energy setting, the firing distance of the pulses, as well as optimal depth of photodisruption and showed the uniformity of the corneal cap. John Marshall investigated the histological tissue effects and benefits of tissue saving and created the term "SBK" ("sub-Bowman's Keratomileusis"). Using real-time pachymetry, Wolfgang Pfäffl and his team at the Technical University of Munich demonstrated the independence of the "Femto-Flap" from the many setting parameters that no longer had to be taken into account as with keratome LASIK, as well as the low variance of the flap- Thickness of the "flap" thickness set on the femto laser. Both groups described their own new surgical technique for opening the corneal cap preformed in the tissue by the femto laser: Parry Binder the so-called "hinge-opening technique" and Wolfgang Pfäffl the so-called "flaporhexis". In a study Michael Knorz was able to show the better adhesion of the Femto-Flap compared to the Keratome-Flap on the corneal bed. A controlled comparative study between the femtosecond laser and the mechanical keratome in approx. 1000 eyes from 2009 deals with the comparison between the mechanical keratome and the femtosecond laser. In this study it is believed to be able to prove that the postoperative recovery time after the femto-LASIK is much faster than after the keratome-LASIK, whereby the results of the visual acuity test align after 3 months.
The femto laser as the ideal cutting instrument in eye surgery
Femto laser technology has proven to be the ideal tool for controlled computer-controlled surgery on the optical media of the eye and has led to other applications such as femto-cataract surgery and SMILE surgery , an alternative to LASIK surgery. The evaluation of these methods is still part of the current scientific discussion. However, it is already becoming apparent that the same basic physical principles prevail in the SMILE operation, if they are not observed, the same complications threaten as with the femto-LASIK or the keratome-LASIK.
Treatment area and contraindications
The LASIK method is indicated for the correction of:
The Commission for Refractive Surgery (KRC) distinguishes between areas of application , i.e. H. the area in which the method is to be regarded as suitable and complications are rare and the limit area in which the method can still be used, side effects and complication rate are expected to be higher. Stricter information to the patient applies to the border area.
scope of application
Myopia up to -8.0 dpt, farsightedness up to +3.0 dpt and astigmatism up to 5 diopters, whereby the two values added together must not exceed -6.0.
Border area
Myopia up to -10.0 dpt, farsightedness up to +4.0 dpt and astigmatism up to 6 diopters, whereby the two values added together must not exceed -10.0.
These limits can be one to two diopters higher or lower depending on the country, clinic and laser system used . The German Ophthalmological Society (DOG), for example, only classifies LASIK as "scientifically recognized" for myopia up to −10 dioptres and astigmatism up to 3 dioptres.
Contraindications are circumstances that prohibit LASIK treatment or allow it only after careful consideration of the existing risks, for example the presence of signs of corneal disease.
An essential requirement for LASIK treatment is a sufficiently thick cornea and the absence of abnormal corneal changes (indication). The normal area of the cornea is a range of 480–600 µm. A cornea that is too thin is a strict contraindication if there are additional risk factors such as particularly steep corneas (e.g.> 49 Dpt) or irregular astigmatism or bulging of the back of the cornea (subclinical keratoconus). Modern topography devices use computer-aided calculation models to generate probability calculations for the presence of pathological corneal conditions. A residual thickness of at least 250 µm after the treatment is considered to be the limit value for the feasibility of an excimer laser operation. In Germany, the surgeon should also take into account a reserve of 30 µm for any subsequent correction when planning the operation. This residual thickness is calculated from the corneal thickness minus the flap thickness and the maximum depth of removal. LASIK should not be performed if there is chronic progressive corneal disease. Treatment is prohibited, especially in the case of keratoconus , as the cornea is further weakened and the clinical picture would worsen dramatically. If the patient's refraction (optics) is not stable, i.e. if the refraction determinations deviate significantly from one another in relatively short time intervals, LASIK treatment should not be carried out. The eye diseases glaucoma with visual field damage and symptomatic cataract continue to be considered contraindications . General diseases that rule out LASIK treatment are collagenoses , autoimmune diseases and wound healing disorders . Finally, LASIK patients should be at least 18 years old. For some corneal diseases, eye laser treatment in the form of a PTK (phototherapeutic keratectomy) is the therapy of choice and is then financially supported by the statutory health insurance.
Preliminary examinations for laser eye surgery
The expectations of the treatment result vary greatly from patient to patient and should be discussed extensively with the attending physician in advance.
First of all, in addition to a detailed specialist eye examination, the focus is on determining the current ametropia. The refraction determination, i.e. H. the refractive power of the glasses value should be done at least twice with an interval of at least 2 weeks, since fluctuations of up to 0.50 dpt are considered normal. A long enough break from contact lenses before the examination is mandatory. The refraction should be determined by an experienced ophthalmologist or an optometrist . A single refraction determination with an automatic refractometer is to be classified as insufficient in any case. It is desirable for the surgeon to determine the refraction personally, since he is essentially responsible for a treatment error. Furthermore, the corneal thickness must be determined, usually with the help of a so-called pachymeter . The decisive parameters for an eye laser operation leading to the target is the ideal combination of corneal thickness, size of the planned optical zone and the number of diopters to be corrected. The more ametropic the patient is or the wider the diameter of his pupil at night, the more cornea has to be removed in order to achieve a visually perfect result. If the cornea is too thin or the optically effective zone cannot be planned to be sufficiently large, the responsible ophthalmologist will refuse the operation for safety reasons or recommend the patient to reduce the planned target correction. If there are deviations from the therapy plan or if the KRC criteria are exceeded, which may be necessary in individual cases, the patient in Germany must be informed in writing about this risk. The risk profile of laser eye surgery has been sufficiently scientifically researched that, as a rule, both eyes can be operated on in one day.
The preliminary examinations serve on the one hand to record the correct treatment data, but on the other hand also to rule out contraindications. The patient should not wear contact lenses for at least two weeks prior to the preliminary examinations.
Overall, the following examinations should be performed before the operation:
- Determination of the corneal thickness with an ultrasonic pachymeter or anterior chamber OCT
- Corneal topography for determining the corneal curvature and detection of corneal irregularities
- Measurement of the pupil size (pupillometry)
- Intraocular pressure measurement
- Tear film determination
- General ophthalmological examination including slit lamp examination
- Examination of the retina with the pupil wide open (mydriasis / cycloplegia)
- anamnese
Treatment process
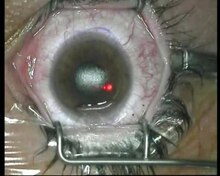
First, the eye is anesthetized locally with drops and an eyelid retractor is used to keep the eye wide open. With a microkeratome (corneal plane) or a femtosecond laser (so-called Femto-LASIK) a thin lamella (diameter approx. 8 to 9.5 mm and thickness between 100 and 160 µm) is cut into the cornea. This flap is not completely separated, but maintains a connection to the rest of the cornea, which serves as a "hinge". Today, this “hinge” is usually placed superiorly (i.e. at the top), but occasionally also nasally (towards the nose) (partly depending on the microkeratome) or programmed as an oval flap with the femto laser for severe astigmatism.
The microkeratome as well as the interface of the femto laser usually consists of two parts, a suction ring for fixation and a movable cutting head with an oscillating blade. Laser beam exit lens. During this process, the eye temporarily loses its light perception, as the intraocular pressure increases and the blood flow in the retinal vessels is briefly reduced or stopped. The flap cut is done in a few seconds and eyesight returns immediately.
The video on the right shows a typical LASIK treatment with a microkeratome.
The eye is held open by a lid holder and the area around the eye is covered in a sterile manner. Before the microkeratome incision is made, the cornea is marked asymmetrically so that the flap can be repositioned correctly in the event of a complication. The suction ring of the microkeratome is then placed centrally on the eye and the microkeratome itself is inserted. With a rapidly oscillating blade, the microkeratome executes the forward movement and thus cuts the flap (in this case superior ).
After the incision, the flap is opened and the remaining corneal thickness is measured using an ultrasound pachymeter to determine whether the flap had the desired thickness. When the flap is open, it is ensured before the actual treatment that the surface to be treated is evenly dry. If this were not the case, the strong absorption of the excimer light in water would result in uneven tissue removal.
The excimer laser treatment itself is hardly noticeable because the excimer laser light with its wavelength of 193 nm is invisible. You can see minimal changes in shape on the treated corneal surface through the surgical microscope.
Following the laser ablation, the treated area is rinsed and the flap is folded back with further rinsing. Thorough rinsing is important in order to remove any foreign bodies (debris, epithelial cells, methocel particles from the swab, fat from the tear film) from the area between the flap and the cornea (the so-called interface). The excess liquid is sucked out of the interface with a small sponge and the flap is smoothed. The treatment is now over and the eyelid retractor can be removed.
The flap cut with the femtosecond laser is becoming more and more popular over the mechanical microkeratome. It offers various advantages, in particular greater safety, as the cut can be visually monitored, stopped and readjusted. If the laser cut is not carried out correctly (e.g. loosening the connection piece between the eye and the laser exit lens due to loss of suction), the treatment can be repeated or safely terminated depending on the case. As the laser perforates the tissue with tiny bubbles, there are always tissue bridges that the doctor has to separate with a suitable instrument in order to completely separate the tissue. You can think of it like the perforation on postage stamps, which requires effort to separate them, but the separation takes place exactly at the specified point. If the doctor decides to stop the treatment, the vesicles that are created are absorbed by the tissue and the cornea is practically intact. A special technique of corneal cap separation is called flaporhexis . It reduces the mechanical stress on the corneal cap when it is separated from the corneal stroma and leaves the central area above the entrance pupil free from contact with an instrument. This represents the ideal prerequisite for a wavefront-guided ablation with the excimer laser, which is not influenced by mechanical instruments. Another technique of corneal cap separation is known as hinge-opening ("hinge opener").
Another advantage is the precision of the cut, which ensures that the flap has the preset dimensions with high accuracy. This allows much thinner flaps to be cut (minimum 90 µm). The treatment using a femtosecond laser is called Femto-LASIK. It represents a technically more demanding variant with less tissue consumption due to a uniform corneal flap and the associated usually thicker residual thickness of the corneal stroma, as well as a more stable edge geometry. With a so-called "incorrect cut" there are usually no complications to fear the tissue separated by photo-disruption usually heals without any problems and the incision can be repeated after the healing time.
After a successful flap cut, this, including Bowman's basement membrane and epithelium, is folded to the side and the laser treatment is carried out on the underlying tissue in the corneal stroma. The duration of the laser irradiation depends on the extent of the Dpt correction and the treatment diameter, but with modern lasers it is usually less than 30 seconds. During the treatment, a so-called "eye tracking" system follows the eye movements and guides the laser beam to the eye movements to. At the end of the laser treatment, the flap is folded back into its original position, the area between the flap and the cornea is thoroughly rinsed and the flap is carefully positioned. If the doctor is satisfied with the flap position, he removes the eyelid retractor and the patient can close his eye. The epithelium at the edge of the flap heals independently within one to two days. However, it takes several weeks to several months for the entire cut surface to adhere firmly.
Advantages and disadvantages
Advantages of LASIK:
- Hardly any pain during and after the operation.
- Very fast vision recovery , the treatment result can be experienced practically immediately after the procedure.
- Low risk of infection compared to implants.
- We have years of experience from millions of operations worldwide.
disadvantage
- The flap entails various risks (see risks)
- Dry eyes of 6–8 weeks on average, longer if the hormone status (estrogen / thyroxine) is abnormal
Due to the constant further development of the technology, older or long-term studies on LASIK are only of limited informative value. Improvements such as better tracking systems and optimized ablation profiles have not yet been incorporated into some studies. Modern treatment methods and the surgeons' increasing experience provide a high level of predictability. About 85% of those treated are in the range of ± 0.5 diopters.
In a one-year LASIK study, 78% of patients achieved the desired correction (± 0.5 diopters, sometimes with two operations). After twelve months, only 5% had night vision problems. Approximately 94% had the same or better uncorrected visual acuity after that year. The American Food and Drug Administration (FDA) presents very detailed study results on its website. These studies are carried out as part of the approval process for refractive laser devices and are considered to be very reliable. They are strictly monitored and carried out in parallel at several clinics.
Risks
As with any surgical procedure, there are a number of risks with LASIK. The type and frequency of occurrence depend, among other things, on the surgeon's experience, the level of correction, the laser or surgical technique used and individual patient-related influencing factors.
General risks that exist with LASIK, but also with any other type of refractive surgery, are restrictions in twilight and night vision if the optical zone is too small due to reduced contrast sensitivity, glare (glossy effects) and halogons (halos). Short-term to long-term over- or undercorrections as well as a reduction in visual acuity with optimal glasses correction (so-called best-corrected visual acuity) can also occur. Infections of the eye are rare but possible and can usually be treated well with careful postoperative care.
The risk of visual impairment after LASIK treatment also depends on individual risk factors (such as the number of diopters, flat cornea, pupil size). In addition, the surgeon's experience has a serious influence on the complication rate. A study from 1998 compared the intraoperative complication rate of the first 200 treatments by a surgeon with that of the following 4800 treatments. The rate for the first 200 treatments is 4.5%, and only 0.87% for the subsequent treatments.
There is a certain risk in the structural weakening of the cornea after tissue removal. This weakening and the constant intraocular pressure acting on the cornea can lead to a bulging of the cornea ( keratectasia ). The risk of this increases as the remaining thickness of the cornea decreases after the treatment. The minimum value for the remaining thickness is 250 µm. The remaining thickness is calculated from the central corneal thickness minus the flap thickness and the central tissue removal. Post-LASIK keratectasia is a long-term complication that can occur with a latency period of up to 10 years. The frequency of this severe, visually impairing complication is given as around 0.6% and 0.9% or up to 2.5% for higher myopia.
The LASIK method involves a number of risks, especially when it comes to cutting the flap. In the first few days after treatment, the cornea may feel uncomfortable. Very often, in 15–20% of cases, dry eyes occur in the first few weeks or months after treatment. The cause of dry eyes lies in the severing of corneal nerves through the flap incision. The severed nerves can no longer recognize the desiccation of the corneal surface and tear production and blinking frequency are reduced. Patients with chronic dry eye are more likely to get worse.
Cutting the flap is a serious risk, especially when using a microkeratome. The desired shape and size of the flap may not be achieved and in rare cases incomplete or broken flaps (hemi-flap or buttonhole flap) ) come. Another risk, especially with the keratome flap, is the ingrowth of epithelial cells from the incision under the flap. These lead to cloudiness in the affected area, but are relatively easy to remove by the doctor. After the treatment, the flap can be displaced by strong external influences, or even cut off. Such a risk exists especially in sports or car accidents. After all, there is a risk of ectasia with every laser eye operation , possibly to a greater extent with keratome LASIK than with PRK, since the cornea is weakened in a deeper tissue section. In general, it would therefore be desirable to routinely use so-called online pachymetry, which measures the removal of the cornea in real time while the excimer laser is in action, in order to prevent the excimer from accidentally penetrating too deep into the cornea and falling below the critical limit values.
Since the first LASIK treatments were only carried out in 1990, there are now longer-term findings on their possible long-term effects. About <1% of all LASIK patients experience complications during surgery. After the operation, the flap is largely held by adhesive forces. The flap can be raised even after seven years. The flap proves to be extremely stable. Absolute rarities are dislocations with little external influence (rubbing on the eye, contact lenses). These are possible through sports injuries (such as squash balls or rubber expanders), contact with the claws of pets or car accidents with airbags being triggered. Only with a correct and timely revision by a specialist can an acceptable visual acuity be restored in the event of an accident.
Proof of quality
The objective proof of quality is very important for patients. There are various certificates that are used in healthcare.
QM certificate according to ISO 9001
The ISO 9001 certificate is a purely process-oriented quality management seal that is awarded across all industries. It reflects process quality and says nothing about the quality of the medical treatment or the technical status of the instruments used.
LASIK-TÜV (2006-2017)
From 2006 to 2017 there was the so-called LASIK TÜV especially for eye laser centers, which was based on the ISO 9001: 2000 certificate. It was offered by TÜV SÜD and was developed in cooperation with the Refractive Surgery Commission (KRC), the Association of Special Clinics for Laser Eye and Refractive Surgery (VSDAR eV) and the Professional Association of Ophthalmic Surgeons (BDOC). In contrast to the ISO-9001: 2000 certificate, the LASIK-TÜV not only checked the process quality, but also the quality of service and results. The following aspects were specifically examined:
- Qualifications and experience of employees and doctors,
- technical equipment of the facility,
- Facility hygiene standards,
- Treatment results,
- Patient satisfaction.
The issuing of TÜV certificates for LASIK providers was discontinued in January 2017. Since then, the corresponding test marks may no longer be used by the clinics.
Alternatives
Surgical methods with a lower frequency of flap-related complications are:
- Femtosecond lenticle extraction - the flap is cut using a laser
- Small Incision Lenticule Extraction - only a small laser incision of 2 to 4 mm in length is required
literature
- Theo Seiler: Refractive Surgery of the Cornea. Georg Thieme Verlag, Stuttgart 2000, ISBN 3-13-118071-4 .
- Berthold Graf: A life without glasses and contact lenses - eye lasers and other alternatives. Baltic Sea Press, Rostock 2009, ISBN 978-3-942129-14-5 .
- Thomas Kohnen: Refractive Surgery. Springer, Berlin 2010, ISBN 978-3-642-05405-1 .
- Irmgard Huber, Wolfgang Lackner, Wolfgang Pfäffl: Eye laser - the successful therapy for ametropia . 2nd Edition. Schlütersche Verlagsgesellschaft, Hanover 2005, ISBN 3-517-06202-2 .
Web links
- Information from the Refractive Surgery Commission
- Official website of TÜV Süd for the LASIK test seal
Individual evidence
- ↑ H. Schiotz: A case of severe corneal astigmatism after starling extraction. Improvement in an operational way. In: Arch Augenheilkd. 15, 1885, pp. 178-181.
- ↑ T. Sato, K. Akiyama, H. Shibata: A new surgical approach to myopia. In: Am J Ophthalmol. 36 (6 1), Jun 1953, pp. 823-829.
- ^ A b S. N. Fjodorow, VV Durnev: Operation of dosaged dissection of corneal circular ligament in cases of myopia of mild degree. In: Ann Ophthalmol. 11 (12), Dec 1979, pp. 1885-1890.
- ↑ a b c T. Seiler: Recent developments in refractive corneal surgery. In: Curr Opin Ophthalmol. tape 3 , no. 4 , 1992, pp. 482-487 .
- ↑ a b c G. J. Florakis, DA Jewelewicz, NI Fan, SL Trokel: Night vision testing in unoperated eyes . In: J Refract Surg. tape 12 , no. 2 , 1996, p. 311-312 .
- ↑ JI Barraquer: Queratoplastia Refractiva. In: Estudios e Informaciones Oftalomológicas. 10, 1949, pp. 1-21.
- ^ HE Kaufman, MB McDonald: Refractive surgery for aphakia and myopia. In: Trans Ophthalmol Soc U K. 1985, 104 (Pt 1), S, 43-47
- ↑ W. Pfäffl, MR Pertzsch, M. Ulmann: The correction of myopia greater -8,0dpt means Photoablativer keratectomy (PRK) after 2 years . 10th Congress of German Ophthalmic Surgeons (DOC), International Symposium, 12. – 15. June 1997.
- ^ PS Binder: Analysis of ectasia after laser in situ keratomileusis: risk factors. In: Journal of Cataract and Refractive Surgery. 33, 2007, pp. 1530-1538.
- ^ KD Solomon, LE Fernández de Castro, HP Sandoval, JM Biber, B. Groat, KD Neff, MS Ying, JW French, ED Donnenfeld, RL Lindstrom; Joint LASIK Study Task Force: LASIK world literature review: quality of life and patient satisfaction. In: Ophthalmology. 116 (4), Apr 2009, pp. 691-701. doi: 10.1016 / j.ophtha.2008.12.037. Review. PMID 19344821
- ↑ a b Veronika Hackenbroch: The cornea is not suitable for a Lasik. In: Spiegel Online . November 12, 2008 (interview with critics).
- ↑ Brief overview of the methods of refractive surgery . Refractive Surgery Commission (KRC), 2010; Retrieved November 3, 2010.
- ↑ Thomas Kohnen, Anja Strenger, Oliver K. Klaproth: Basic knowledge of refractive surgery. Correction of refractive errors with modern surgical procedures. In: Deutsches Ärzteblatt. Vol. 1051, No. 9129, 2008, pp. 163–177 (PDF).
- ^ PF Stanley, DJ Tanzer, SC Schallhorn: Laser refractive surgery in the United States Navy. In: Curr Opin Ophthalmol. 2008 Jul, 19 (4), pp. 321-324. doi: 10.1097 / ICU.0b013e3283009ee3. Review. PMID 18545015
- ↑ Refractive surgery program policy changes ( English ) US Air Force. May 24, 2007. Accessed July 12, 2019.
- ↑ DP O'Brart, CP Lohmann, FW Fitzke, G. klonos, MC Corbett, MG Kerr-Muir, J. Marshall: Discrimination between the origins and functional implications of haze and halo at night after photorefractive keratectomy. In: J Refract Corneal Surg. tape 10 , no. 2 , 1994, p. 281 .
- ↑ AW Chang, AC Tsang, JE Contreras, PD Huynh, CJ Calvano, TC Crnic-Rein, EH Thall: Corneal tissue ablation depth and the Munnerlyn formula . In: J Cataract Refract Surg. tape 29 , no. 6 , 2003, p. 1204-1210 .
- ↑ CR Munnerlyn, SJ Koons, J. Marshall: Photorefractive keratecomy: a technique for laser refractive surgery . In: Journal of Refractive Surgery . tape 14 , 1988, pp. 46-52 .
- ^ A b Dan Z. Reinstein, Timothy J. Archer, Marine Gobbe: The History of LASIK . In: Journal of Refractive Surgery . tape 28 , no. 4 , April 1, 2012, ISSN 1081-597X , p. 291–298 , doi : 10.3928 / 1081597x-20120229-01 ( healio.com [accessed November 4, 2018]).
- ^ GI Duncker, J. Krumeich, F. Wilhelm, T. Bredehorn: Lamellar Keratoplasty . In: Klin Monbl Augenheilkd . tape 221 , no. 1 , 2004, p. 14-23 .
- ↑ RW Beuerman, MB McDonald, D. Zhang, RJ Varnell, HW Thompson: Diclofenac sodium attenuates neural activity after photorefractive keratectomy in rabbits. In: J Refract Surg. tape 12 , no. 7 , 1996, pp. 783-791 .
- ↑ JL Güell: Time-expanding options in laser corneal refractive surgery. In: Br J Ophthalmol. tape 97 , no. 8 , 2013, p. 951-952 .
- ↑ IG Pallikaris, DS Siganos: Excimer laser in situ keratomileusis and photorefractive keratectomy for correction of high myopia. In: J Refract Corneal Surg . tape 10 , no. 5 , 1994, pp. 498-510 .
- ↑ VJ Katsanevaki, Kalyvianaki, DS Kavroulaki, IG Pallikaris: MI Epipolis laser in-situ keratomileusis: an evolving surface ablation procedure for refractive corrections. In: Current Opinions of Ophthalmology . 4th edition. No. 17 , 2006, p. 389-393 .
- ↑ Larkin Howard: A proud heritage . In: Eurotimes . tape 15 , no. 6 , 2010, p. 4-6 .
- ^ A b I. M. Neuhann, BA Lege, M. Bauer, JM Hassel, A. Hilger, TF Neuhann: Online optical coherence pachymetry as a safety measure for laser in situ keratomileusis treatment in 1859 cases . In: J Cataract Refract Surg. tape 34 , no. 8 , 2008, p. 1273-1279 .
- ↑ a b ARD magazine monitor from October 9, 2003.
- ↑ ES Rosen: LASIK mania. In: J Cataract Refract Surg. tape 26 , no. 3 , 2000, pp. 303-304 .
- ↑ ES Rosen: Uncannily prescient . In: J Cataract Refract Surg. tape 10 , no. 28 , 2002, pp. 1717-1718 .
- ↑ T. Fiore, F. Carones, R. Brancato: Broad beam vs. flying spot excimer laser: refractive and videokeratographic outcomes of two different ablation profiles after photorefractive keratectomy. In: J Refract Surg. tape 17 , no. 5 , 2001, p. 534-541 .
- ↑ GD Kymionis, NS Tsiklis, N. Astyrakakis, AI Pallikaris, SI Panagopoulou, IG Pallikaris: Eleven-year follow-up of Lasik . In: Journal of Cataract and Refractive Surgery . tape 33 , no. 2 , 2007, p. 191-1196 .
- ↑ RD Stulting, JD Carr, KP Thompson, GO Waring 3rd, WM Wiley, JG Walker: Complications of laser in situ keratomileusis for the correction of myopia. In: Ophthalmology . tape 106 , no. 1 , 1999, p. 13-20 .
- ^ MC Knorz, B. Wiesinger, A. Liermann, V. Seiberth, H. Liesenhoff: Laser in situ keratomileusis for moderate and high myopia and myopic astigmatism . In: Ophthalmology . tape 105 , no. 5 , 1998, pp. 932-940 .
- ^ PS Binder: Analysis of ectasia after laser in situ keratomileusis: risk factors. In: Journal of Cataract and Refractive Surgery . tape 33 , 2007, p. 1530-1538 .
- ↑ KD Solomon, E. Donnenfeld, HP Sandoval, O. Al Sarraf, TJ Kasper, MP Holzer, EH Slate, DT Vroman: Flap Thickness Study Group Flap thickness accuracy: comparison of 6 microkeratome models . In: J Cataract Refract Surg. tape 30 , no. 5 , 2004, p. 964-977 .
- ↑ M. Mlocken, M. Kaemmerer, T. Seiler: Wavefront-guided laser in situ keratomileusis: early results in three eyes. tape 16 , no. 2 . J Refract Surg., 2000, pp. 116-121 .
- ↑ Irmgard Huber, Wolfgang Lackner, Wolfgang Pfäffl: Eye laser - successful therapy for ametropia . 2nd Edition. Schlütersche Verlagsgesellschaft, Hanover 2005, p. 46-49 .
- ^ John Marshall: Wound healing and biomechanics of corneal flap creation. In: ESCRS (ed.): XXIV Congress of the ESCRS . London 2006.
- ^ I. Ratkay-Traub et al .: Ultra-short pulse (femtosecond) laser surgery: initial use in LASIK flap creation. In: Ophthalmology clinics of North America . tape 14 , no. 2 , 2001, p. 347-355 .
- ^ SG Slade, DS Durrie, PS Binder: A prospective, contralateral eye study comparing thin-flap LASIK (sub-Bowman keratomileusis) with photorefractive keratectomy . In: Ophthalmology . tape 116 , no. 6 , 2009, p. 1075-1082 .
- ↑ WA Pfaeffl, M. Kunze, U. Zenk, MB Pfaeffl, T. Schuster, C. Lohmann: Predictive factors of femtosecond laser flap thickness measured by online optical coherence pachymetry subtraction in sub-Bowman keratomileusis. In: Journal of Cataract and Refractive Surgery. Volume 34, Number 11, November 2008, pp. 1872-1880. doi: 10.1016 / j.jcrs.2008.07.017 . PMID 19006732
- ↑ a b P. S. Binder: One thousand consecutive IntraLase laser in situ keratomileusis flaps . In: Journal of Cataract and Refractive Surgery . tape 32 , no. 6 , 2006, p. 962-969 .
- ↑ WA Pfaeffl: Opening the Femtosecond Laser Flap . In: Cataract & Refractive Surgery Today . 6th edition. No. 1 , 2006, p. 22-23 .
- ↑ MC Knorz, U. Vossmerbaeumer: Comparison of flap adhesion strength using the Amadeus microkeratome and the IntraLase iFS femtosecond laser in rabbits . In: Journal of Refractive Surgery . tape 24 , no. 9 , 2008, p. 875-788 .
- ↑ M. Tanna, SC Schallhorn, KA Hettinger: Femtosecond laser versus mechanical microkeratome: a retrospective comparison of visual outcomes at 3 months. tape 25 . Journal of Refractive Surgery, 2009, pp. 668-671 .
- ↑ W. Secondo, KS Kunert, M. Blum: Small incision corneal refractive surgery using the small incision lenticule extraction (SMILE) procedure for the correction of myopia and myopic astigmatism: results of a 6 month prospective study . In: British Journal of Ophthalmology . tape 95 , no. 3 , 2011, p. 335-339 .
- ↑ M. Blum, K Täubig, C. Gruhn, W. Secondo, KS Kunert: Five-year results of Small Incision Lenticule Extraction (ReLEx SMILE) . In: British Journal of Ophthalmology . tape 100 , no. 9 , 2016, p. 1192-1195 .
- ↑ DZ Reinstein, TJ Archer, JB Randleman: Mathematical model to compare the relative tensile strength of the cornea after PRK, LASIK, and small incision lenticule extraction . In: Journal of Refractive Surgery . tape 29 , no. 7 , 2013, p. 454-460 .
- ↑ M. Moshirfar, JC Albarracin, JD Desautels, OC Birdsong, SH Linn, PC Hoopes Sr .: ectasia Following small-incision lenticule extraction (SMILE): a review of the literature . In: Clinical Ophthalmolology . tape 15 , no. 11 , 2017, p. 1683-1688 .
- ↑ JB Randleman: ectasia after Corneal Refractive Surgery: Nothing to SMILE About . In: Journal of Refractive Surgery . tape 32 , no. 7 , 2016, p. 434-435 .
- ↑ a b Thomas Kohnen, Anja Strenger, Oliver K. Klaproth: Basic knowledge of refractive surgery. Correction of refractive errors with modern surgical procedures. In: Deutsches Ärzteblatt. Vol. 1051, No. 9129, 2008, pp. 163-177. dgii.org ( Memento of July 6, 2010 in the Internet Archive ) (PDF)
- ↑ Brief overview of the methods of refractive surgery. (No longer available online.) Refractive Surgery Commission (KRC), 2010, archived from the original on March 4, 2016 ; accessed on December 1, 2018 . Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ Patient information on laser in situ keratomileusis (LASIK). (No longer available online.) Refractive Surgery Commission (KRC), 2010, archived from the original on November 27, 2010 ; Retrieved November 3, 2010 . Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ Examinations and measures to be taken before an operation . Lasik Directory, editorial information on eye surgery
- ↑ necessary examinations before the ametropia can be corrected ( memento from January 6, 2013 in the web archive archive.today ). Carl Gustav Carus University Hospital Dresden at the Technical University of Dresden.
- ↑ a b c W. A. Pfaeffl, M. Kunze, U. Zenk, MB Pfaeffl, T. Schuster, C. Lohmann: Predictive factors of femtosecond laser flap thickness measured by online optical coherence pachymetry subtraction in sub-Bowman keratomileusis. In: Journal of Cataract and Refractive Surgery. Volume 34, Number 11, November 2008, pp. 1872-1880. doi: 10.1016 / j.jcrs.2008.07.017 . PMID 19006732
- ^ A b S. E. Wilson, MR Santhiago: Flaporhexis: Rapid and effective technique to limit epithelial ingrowth after LASIK enhancement. In: Journal of Cataract and Refractive Surgery . [electronic publication before going to press] November 2011. doi: 10.1016 / j.jcrs.2011.10.015 . PMID 22082751
- ↑ a b Mihai Pop, Yves Payette: Risk Factors for Night Vision Complaints after LASIK for Myopia. In: Ophthalmology. 111, 2004, pp. 3–10, arcor.de/pinnipedii (PDF).
- ↑ FDA-Approved Lasers for LASIK . Food and Drug Administration, November 27, 2009.
- ↑ Simulator for twilight and night vision according to LASIK depending on the number of diopters and pupil diameter . April 28, 2010.
- ↑ Individual risk factors for halos, loss of contrast, glare, starburst after LASIK . operationauge.de, March 11, 2010.
- ↑ JS Vidaurri-Leal: Complications in 5000 LASIK procedures . In: Group RSSI (Ed.): Refractive Surgery . 1998, p. 61-64 .
- ↑ PS. Binder: Analysis of ectasia after laser in situ keratomileusis: risk factors. In: Journal of Cataract and Refractive Surgery. 33, 2007, pp. 1530-1538.
- ↑ L. Spadea et al: Corneal Crosslinking for Keratectasia after Laser in situ Keratomileusis: A Review of the Literature. In: J Kerat Ect Cor Dis. 2, 2013, pp. 113-120.
- ↑ JL Alio et al .: Laser in situ keratomileusis for −6.00 to −18.00 dioptres of myopia and up to −5.00 dioptres of astigmatism: 15-years follow-up. In: Journal of Cataract and Refractive Surgery. 41, 2015, pp. 33-40.
- ↑ Julie Albietz et al: Chronic dry eye and regression after laser in situ keratomileusis for myopia. In: Journal of Cataract & Refractive Surgery. Volume 30, Issue 3, pp. 675-684, March 2004 ( jcrsjournal.org ).
- ↑ Veronika Hackenbroch: The cornea is not suitable for a Lasik . In: Spiegel Online . November 12, 2008 (interview with critics).
- ↑ Sunil Shah, Vinod Kumar: Has LASEK superseded LASIK? In: Optometry Today. 6/2003, pp. 22-25. laseroogchirurgie.com (PDF).
- ↑ Quentin Franklin et al: Late Traumatic Flap Displacement after LASIK. In: Military Medicine. No. 169, 2004, pp. 334-336, home.arcor.de/pinnipedii (PDF).
- ↑ TH Tsai, KL Peng, CJ Lin: Traumatic corneal flap displacement after laser in situ keratomileusis (LASIK) . In: Int Med Case Rep J. Band 10 , no. April 19 , 2017, p. 143-148 .
- ↑ TÜV Süd: List of certified clinics. Retrieved December 6, 2010 .
- ↑ The LASIK TÜV seal of approval. (No longer available online.) Archived from the original on March 6, 2010 ; Retrieved March 3, 2010 . Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ TÜV-Süd - The LASIK-TÜV SÜD standard has been discontinued