Potassium channel
The potassium channel ( engl. Potassium Channel ) denotes an ion channel , of the passage in a specific manner for potassium ion allowed. The transport of potassium ions through the potassium channel occurs passively by diffusion . Its direction is determined by the electrochemical driving force for potassium ions.
Mechanisms of activation of different potassium channels
Voltage activated potassium channels
Voltage- activated potassium channels ( TCDB : 1.A.1.2 ) open when the membrane potential changes and support e.g. B. the repolarization during the action potential of a neuron . This type of potassium channel is activated by depolarizing the membrane at the same threshold potential as that of the sodium channels . However, the opening of the potassium channel of this type is much slower and lasts longer than that of the sodium channel.
Another voltage-activated potassium channel opens and closes extremely quickly during the depolarization (10 −4 to 10 −5 s), causing a short-term repolarizing potassium outflow ( A-current , I A ) and thus enables a quick " Firing “of the nerve cells.
A distinction is made between outward and inward rectifying potassium channels ( outward rectifier (K or ) and inward rectifier (K ir ) ). The respective direction (outward or inward) only refers to the kinetically favored, but not to the actual direction of the ion current. An inward rectifying potassium channel occurs almost ubiquitously in human cells, but this causes an outward current of potassium ions due to the electrochemical driving force for potassium.
Calcium-activated potassium channels
( TCDB : 1.A.1.3 ) They open when the intracellular calcium ion concentration rises sharply and thereby repolarize or hyperpolarize the cell membrane .
G protein activated potassium channels
These are potassium channels that are regulated directly by G proteins or indirectly by second messengers . After activation of the G protein-coupled receptor ( GPCR ) by the ligand (e.g. acetylcholine in the case of the muscarinic acetylcholine receptor ), GDP is exchanged for GTP in the Gα unit of the G protein . In the protein activated as a result, the α unit now detaches from the rest, which means that Gβγ can bind to the potassium channel and open it. This remains open until the bound GTP on Gα hydrolyzes again to GDP and the subunits form again. These channels play an important role for the regulation of the heart rate through the parasympathetic part of the autonomic nervous system and at inhibiting synapses in the central nervous system.
Mechanically activated potassium channels
They open by pushing or pulling the membrane. This is how z. B. the potassium channels at the tip links of the stereocilia , i.e. the sensory hair cells in the inner ear .
ATP-sensitive potassium channels
They open when the cellular ATP level drops and are e.g. B. contained in the insulin-producing beta cells of the pancreas and in neurons of the hypothalamus .
ATP-sensitive potassium channels ( TCDB : 1.A.2 ) are an important part of the blood sugar sensor system . They consist of an outer ring made up of four identical regulatory subunits called SUR1 and an inner ring made up of four identical, smaller subunits called Kir6.2 that surround the central pore. The task of the ATP-sensitive potassium channels of the beta cell of the pancreas is to link the nutritional metabolism of the beta cell with its electrical membrane activity. If the blood sugar level is low, the cell can produce little ATP, the ATP-sensitive potassium channel is open, and a resting membrane potential develops on the membrane of the beta cell . If the blood sugar level rises, more glucose gets into the beta cell through the non- insulin dependent glucose transporter 2 , and more energy-rich ATP can be formed. ATP binds to the regulatory subunit of the ATP-sensitive potassium channel, the potassium channel is closed. This leads to an increase in the intracellular potassium concentration, the membrane potential decreases, and depolarization occurs . Voltage-dependent calcium channels are opened by the depolarization and calcium flows into the cell. The increased intracellular calcium concentration is the signal for insulin-containing vesicles to fuse with the cell membrane and thus to secrete insulin . The rise in insulin then leads to a fall in blood sugar.
ATP-sensitive potassium channels are blocked by drugs from the group of sulfonylureas . Activating mutations in the ABCC8 gene , which codes for the regulatory subunits ( SUR1 ) of the ATP-sensitive potassium channel, are responsible for approx. 12% of cases of congenital diabetes mellitus in the newborn ( neonatal diabetes mellitus ). Activating mutations in the KCNJ11 gene , which codes for the Kir6.2 subunits of the ATP-sensitive potassium channel, underlie approximately 35–58% of cases of neonatal diabetes. Neonatal diabetes mellitus can be successfully treated with sulfonylureas ( Frances Ashcroft , Andrew Hattersley ) Inactivating mutations in the ABCC8 gene, on the other hand, lead to hypoglycaemia in early childhood ( familial hyperinsulinemic hypoglycaemia ).
The potassium channel KIR4.1 is found on glial cells in the central nervous system , especially on astrocytes , oligodendrocytes and Bergmann glial cells. The main task seems to be spatial buffering of the potassium gradient in order to maintain axonal stimulus transmission. Knock-out mice without Kir4.1 showed severe hypomyelination and axonal changes. IgG autoantibodies against the potassium channel were found in a subgroup of patients with multiple sclerosis . Mutations in the KIR4.1-encoding gene KCNJ10 are associated with EAST or SeSAME syndrome, which is associated with epilepsy , ataxia , renal tubulopathy, and deafness .
selectivity
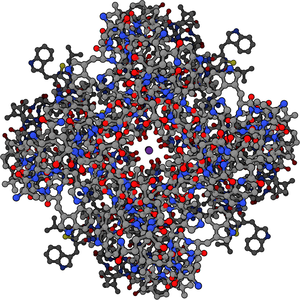
Potassium channels form a pore in the membrane. The so-called selectivity filter is located on the extracellular side of the pore. This pore is formed from the polypeptide backbone, whereby the carbonyl oxygen atoms of the peptide bonds are precisely aligned so that they can "take over" the role of oxygen in the water molecules of the hydration shell of the potassium ion. This creates energetically stabilized positions for the potassium ion in the selectivity filter (more precisely 4), which facilitates dehydration and thus passage of the potassium ion through the pore. Inside the pore there is a pocket of water molecules where the potassium ions are immediately rehydrated. For example, sodium ions do not pass the selectivity filter even though they are smaller than potassium ions. This is because the carbonyl oxygen atoms are too far away for them and thus they cannot replace the oxygen atoms in the water (here no energetic stabilization).
Inhibition of the potassium channel
Like other channels, potassium channels can also be specifically blocked by molecules or peptides. Depending on the type of potassium channel, different substances are capable of doing this. So z. For example, calcium-dependent potassium channels can be specifically blocked without affecting other channels. Therefore, not every inhibitor has the same effect in the body, since the different types of channels differ in their occurrence and function.
Often, the inhibitor acts directly on the pore of the channel by closing this (for example, the. Tetraethylammonium - cation ) be it from the outside or the inside of the channel. Many natural plant and animal toxins contain proteins that inhibit potassium channels. For example, over 40 peptides from scorpion poisons are known that have an inhibiting effect on potassium channels. But insect venoms such as apamin in bees are also specific for calcium-dependent potassium channels.
See also
swell
- ↑ MA Sperling: ATP-Sensitive Potassium Channels - Neonatal Diabetes Mellitus and Beyond. ( Memento from January 20, 2007 in the Internet Archive ) In: N Engl J Med. 355, Aug 3, 2006, s. 507-510.
- ↑ H. Yokoshiki et al.: ATP-sensitive K + channels in pancreatic, cardiac, and vascular smooth muscle cells . In: American Journal of Physiology-Cell Physiology . 274, 1998, pp. C25-C37.
- ↑ AP Babenko et al: Activating Mutations in the ABCC8 Genes in Neonatal Diabetes Mellitus. In: N Engl J Med. 355, 2006, pp. 456-466.
- ↑ ER Pearson et al .: Switching from Insulin to Oral Sulfonylureas in Patients with Diabetes Due to Kir6.2 Mutations. In: N Engl J Med. 355, 2006, pp. 467-477.
- ↑ PM Thomas et al: Mutations in the sulfonylurea receptor gene in familial persistent hyperinsulinemic hypoglycemia of infancy. In: Science. 268 (5209), Apr 21, 1995, p. 426.
- ^ Anne H. Cross, Emmanuelle Waubant: Antibodies to Potassium Channels in Multiple Sclerosis. In: New England Journal of Medicine. 367, 2012, pp. 172-174.
- ↑ Rajneesh Srivastava, Muhammad Aslam, Sudhakar Reddy Kalluri, Lucas Schirmer, Dorothea Buck, Björn Tackenberg, Veit Rothhammer, Andrew Chan, Ralf Gold, Achim Berthele, Jeffrey L. Bennett, Thomas Korn, Bernhard Hemmer: Potassium Channel KIR4.1 as an Immune Target in Multiple Sclerosis. In: New England Journal of Medicine. 367, 2012, pp. 115-122.
- R. MacKinnon: ion conduction and the atomic basis of selective ion conduction (Nobel Lecture). In: Angew. Chem. Int. Ed. Engl. 43, 2004, pp. 4265-4277.