Krabbe's disease
| Classification according to ICD-10 | |
|---|---|
| E75.2 | Other sphingolipidoses Crab disease |
| ICD-10 online (WHO version 2019) | |
The Krabbe's disease (also globoidzellige leukodystrophy or globoid cell leukodystrophy ) is a rare congenital monogenic metabolic disorder from the group of sphingolipidoses . This makes the disease one of the lysosomal storage diseases .
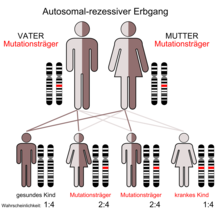
The disease is inherited as an autosomal recessive trait . The cause is a defect in the β-galactocerebrosidase gene (GALC), which codes for the enzyme galactocerebrosidase . The defect can be based on over 200 different mutations .
The lack of the enzyme galactocerebrosidase leads to the accumulation of the cerebroside galactosylceramide in macrophages (formation of "globoid cells "). The accumulation of the metabolite psychosin leads to further damage to the oligodendrocytes . The extensions of these cells form the myelin sheaths, which surround the axons of the nerve cells . The damage to the oligodendrocytes results in demyelination of the nerve cell extensions, an inflammatory reaction and the remodeling of the white matter in connective tissue ( leukodystrophy ).
The majority of cases occur in the first year of life (infantile form). There is also a late form ( late-onset ) that occurs in later childhood and other ages. There is no curative (healing) therapy. The infantile form leads to death in infancy, the prognosis of diseases that occur later varies from person to person.
The disease is named after the Danish neurologist Knud Krabbe , who has described several cases.
Epidemiology
Krabbe's disease is a rare disease . The disease occurs worldwide, with the frequency of occurrence varying regionally. For every 100,000 live births, there are an average of 1–2 infants affected by the infantile form ( incidence ). The other forms of Krabbe's disease occur less frequently, but their incidence may also be underestimated.
genetics
Krabbe's disease is a disease that is based on a genetic defect in the β-galactocerebrosidase gene (GALC). The gene is located on chromosome 14 in section q3.1. The gene product is the enzyme galactocerebrosidase , which breaks down components of the myelin sheath of nerve cells .
The defects in the GALC gene caused by mutations are very heterogeneous. To date, over 200 different pathological gene variants have been detected, including large and small deletions, frameshift mutations and various other point mutations . The most common pathological gene variant results from a large deletion of 30 kb .
The condition is inherited as an autosomal recessive trait. Both parents of an affected person are heterozygous carriers of a pathological GALC gene variant. The probability of illness for one of the couple's children is 25%.
pathology

The enzyme galactocerebrosidase splits galactose from galactocerebrosides in the lysosomes . As a result of defects in the β-galactocerebrosidase gene, the activity of the enzyme in Krabbe's disease is greatly reduced or absent.
The lack of the enzyme galactocerebrosidase leads to the accumulation of the cerebroside galactosylceramide in macrophages (formation of "globoid cells "). Furthermore, the accumulation of psychosin leads to damage to the oligodendrocytes . The extensions of these cells form the myelin sheaths, which surround the axons of the nerve cells . The damage to the oligodendrocytes results in demyelination of the nerve cell extensions, an inflammatory reaction and the remodeling of the white matter in connective tissue ( leukodystrophy ).
Symptoms
The symptoms usually begin at the age of three to six months. The children are easily irritated and tend to have screaming attacks that are difficult to influence. The cognitive - motor development comes to a standstill. External stimuli can lead to tonic extension of the legs. Reflexes can no longer be triggered. In optic atrophy there is blindness .
In the further course deafness , a permanent opisthotonus with bent arms and straight legs as well as hypersalivation and fever develop . The same symptoms occur with the late onset special forms , only the disease begins later and also proceeds more slowly.
diagnosis
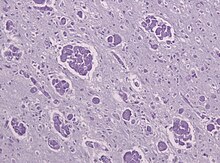
In the cerebrospinal fluid ( liquor cerebrospinalis ) there is typically an increased protein concentration. The nerve conduction speed is reduced. Imaging shows demyelination . In autopsy specimens , monocytes and multinucleated macrophage clusters ( globoid cells ) with PAS-positive but not metachromatic inclusions in gliotically altered brain tissue can be seen.
To confirm the diagnosis, the activity of the enzyme galactocerebrosidase can be determined in leukocytes or fibroblast cultures or a genetic analysis can be carried out. The latter has a mutation in chromosome 14 (section q3.1).
Since it is a recessive inherited disease, the risk for siblings to get sick is also 25%. By prenatal diagnosis can be a Krabbe disease already in utero (in the womb) diagnose or exclude. Relatives can also be examined to see whether they are carriers of the disease.
therapy
The disease cannot be cured. Accordingly, the treatment options for children suffering from the infantile form, who already show signs of the disease, are limited to symptomatic therapy or palliative care. The measures described below may also be necessary in the late-onset form.
The spasticity of the muscles can be favorably influenced with physiotherapeutic measures .
The spasticity can also be improved by administering clonazepam or the muscle relaxant baclofen . The therapeutic use of botulinum toxin on selected muscle groups has also been described.
Make sure you have enough calories and fluids. An upright body position should be maintained during and after feeding to prevent reflux and vomiting. In the further course, liquids often have to be thickened, and a gastrostoma may also be necessary. In case of constipation (constipation) laxatives are indicated. The intestinal motility can be supported by erythromycin .
For the treatment of neuropathic pain and the prevention of seizures is gabapentin used. The rectal administration of diazepam is useful to break through seizures .
The accumulation of residual urine should be avoided in those affected in order to avoid urinary tract infections . Temporary catheterization may be necessary to completely empty the bladder . The permanent application of catheters is not recommended due to the risk of infection.
If the infantile form of the disease is diagnosed before symptoms appear, a stem cell transplant can be attempted. Early therapy within the first few weeks of life can extend life expectancy and improve functional development.
forecast
Children with the infantile form of the Krabbe disease usually die in the first two years of life after the onset of symptoms. A stem cell transplant before the onset of disease can both extend life expectancy and improve functional development.
The prognosis for the late-onset form is very variable.
early detection
Several US states are doing newborn screening for the disease. The aim is to identify affected newborns as quickly as possible and to have a stem cell transplant within the first month of life. Guideline recommendations have now been compiled from the experience gained .
Research history
In 1916, the Danish neurologist Knud Krabbe described five cases of a progressive, fatal illness in infants in the journal Brain , which is characterized by an increase in muscle tone, developmental deficits, fever attacks and opisthotonus . It was the infantile form of globoid cell leukodystrophy, which was named after the person who first described it in the 1940s.
The decreased activity of the enzyme β-galactocerebrosidase in the disease was discovered in the early 1970s. From 1980 a mouse model for the disease was available ( twitcher mouse ). The cDNA coding for β-galactocerebrosidase was cloned in 1993/1994 , and one of the publications also described a nonsense mutation leading to M. Krabbe. The structure of the gene was presented in 1995. In that year the 30kb deletion, which is present in many patients, was also identified.
literature
- Orsini et al .: Crab Disease . In: GeneReviews , 2018.
- D. Wenger, M. Rafi, P. Luzi: Krabbe disease: One Hundred Years from the Bedside to the Bench to the Bedside. In: Journal of Neuroscience Research. 94, 2016, pp. 982-989, doi : 10.1002 / jnr.23743 .
- A. Kohlschütter: Lysosomal leukodystrophies: Krabbe disease and metachromatic leukodystrophy. In: Handbook of Clinical Neurology. 113, 2013, pp. 1611-1618, PMID 23622382 , doi : 10.1016 / B978-0-444-59565-2.00029-0 .
- ML Escolar, T. West, A. Dallavecchia, MD Poe, K. LaPoint: Clinical management of crab disease. In: Journal of Neuroscience Research. 94, 2016, pp. 1118–1125, PMID 27638597 , doi : 10.1002 / jnr.23891 .
Web links
- Krabbe's disease. In: Orphanet (Rare Disease Database).
- Krabbe's disease. In: Online Mendelian Inheritance in Man . (English)
- Krabbe's disease at the European Association against Leukodystrophies (ELA)
Individual evidence
- ↑ Barbara Tappino, Roberta Biancheri u. a .: Identification and characterization of 15 novel GALC gene mutations causing Krabbe disease. In: Human Mutation. 31, 2010, pp. E1894 – E1915, PMID 20886637 , PMC PMC3052420 (free full text), doi : 10.1002 / humu.21367 .
- ↑ a b A. Kohlschütter: Lysosomal leukodystrophies: Krabbe disease and metachromatic leukodystrophy. In: Handbook of Clinical Neurology. 113, 2013, pp. 1611-1618, PMID 23622382 , doi : 10.1016 / B978-0-444-59565-2.00029-0 .
- ↑ MP Wasserstein, M. Andriola u. a .: Clinical outcomes of children with abnormal newborn screening results for Krabbe disease in New York State. In: Genetics in Medicine. 18, 2016, pp. 1235-1243, PMID 27171547 , doi : 10.1038 / gim.2016.35 .
- ↑ Krabbe's disease. In: Online Mendelian Inheritance in Man . (English)
- ↑ a b Orsini et al .: Krabbe Disease . In: GeneReviews , 2018, accessed November 27, 2019.
- ↑ a b c d e M. L. Escolar, T. West, A. Dallavecchia, MD Poe, K. LaPoint: Clinical management of Krabbe disease. In: Journal of Neuroscience Research. 94, 2016, pp. 1118–1125, PMID 27638597 , doi : 10.1002 / jnr.23891 .
- ↑ ML Escolar, MD Poe et al. a .: Transplantation of umbilical-cord blood in babies with infantile Krabbe's disease. In: New England Journal of Medicine . 352, 2005, pp. 2069-2081, PMID 15901860 , doi : 10.1016 / j.bbmt.2018.06.020 .
- ↑ a b M.D. Wright, MD Poe, A. DeRenzo, S. Haldal, ML Escolar: Developmental outcomes of cord blood transplantation for Krabbe disease: A 15-year study. In: Neurology . 89, 2017, pp. 1365-1372, PMID 28855403 , PMC 5649761 (free full text), doi : 10.1212 / WNL.0000000000004418 .
- ↑ JJ Orsini, CA Saavedra-Matiz, MH Gelb, M. Caggana: Newborn screening for Krabbe's disease. In: J. Neurosci. Res. 94, 2016, pp. 1063-1075, PMID 27638592 , PMC 5328187 (free full text), doi : 10.1002 / jnr.23781 .
- ↑ . M. Kwon, D. Matern, et al. a .: Consensus guidelines for newborn screening, diagnosis and treatment of infantile Krabbe disease. In: Orphanet Journal of Rare Diseases. 13, 2018, pp. 30-30, PMID 29391017 , PMC 5796396 (free full text), doi : 10.1186 / s13023-018-0766-x .
- ^ K. Krabbe: A new familial, infantile form of diffuse brain-sclerosis. In: Brain . 39, 1916, pp. 74-114, doi : 10.1093 / brain / 39.1-2.74 .
- ↑ D. Wenger, M. Rafi, P. Luzi: Krabbe disease: One Hundred Years from the Bedside to the Bench to the Bedside. In: Journal of Neuroscience Research. 94, 2016, pp. 982-989, doi : 10.1002 / jnr.23743 .
- ↑ K. Suzuki, Y. Suzuki: Globoid Cell Leucodystrophy (Krabbe's Disease): Deficiency of Galactocerebroside -Galactosidase. In: Proceedings of the National Academy of Sciences. 66, 1970, pp. 302-309, doi : 10.1073 / pnas.66.2.302 .
- ↑ Y. Suzuki, K. Suzuki: Krabbe's Globoid Cell Leukodystrophy: Deficiency of Galactocerebrosidase in Serum, Leukocytes, and Fibroblasts. In: Science. 171, 1971, pp. 73-75, doi : 10.1126 / science.171.3966.73 .
- ↑ LW Duchen, EM Eicher u. a .: Hereditary leucodystrophy in the mouse: the new mutant twitcher. In: Brain . 103, 1980, pp. 695-710, doi : 10.1093 / brain / 103.3.695 .
- ↑ Takuro Kobayashi, Tatsuhiro Yamanaka et al. a .: The twitcher mouse: an enzymatically authentic model of human globoid cell leukodystrophy (Krabbe disease). In: Brain Research. 202, 1980, pp. 479-483, doi : 10.1016 / 0006-8993 (80) 90159-6 .
- ↑ Y. Chen, M. Rafi et al. a .: Cloning and expression cDNA encoding human galactocerebrosidase, the enzyme deficient in globoid cell leukodystrophy. In: Human Molecular Genetics. 2, 1993, pp. 1841-1846, doi : 10.1093 / hmg / 2.11.1841 .
- ↑ a b N. Sakai, K. Inui et al. a .: Krabbe Disease: Isolation and Characterization of a Full-Length cDNA for Human Galactocerebrosidase. In: Biochemical and Biophysical Research Communications. 198, 1994, pp. 485-491, doi : 10.1006 / bbrc.1994.1071 .
- ↑ P. Luzi, MA Rafi, DA Wenger: Structure and organization of the human galactocerebrosidase (GALC) gene. In: Genomics. 26, 1995, pp. 407-409, PMID 7601472 , doi : 10.1016 / 0888-7543 (95) 80230-j
- ↑ MA Rafi, P. Luzi, YQ Chen, DA Wenger: A large deletion together with a point mutation in the GALC gene is a common mutant allele in patients with infantile Krabbe disease. In: Human Molecular Genetics 4, 1995, pp. 1285-1289, PMID 7581365 , doi : 10.1093 / hmg / 4.8.1285 .