Mumps virus
| Mumps virus | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|

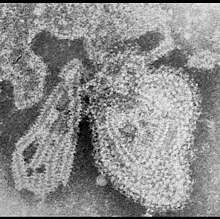
Mumps virus in the TEM illustration |
||||||||||||||||||||
| Systematics | ||||||||||||||||||||
|
||||||||||||||||||||
| Taxonomic characteristics | ||||||||||||||||||||
|
||||||||||||||||||||
| Scientific name | ||||||||||||||||||||
| Mumps orthorubulavirus | ||||||||||||||||||||
| Short name | ||||||||||||||||||||
| MuV | ||||||||||||||||||||
| Left | ||||||||||||||||||||
|
The mumps virus (previously called Paramyxovirus parotitis ) is a virus from the Paramyxoviridae family that only occurs in humans and is the causative agent of mumps ( parotitis epidemica ). The virus was first propagated and characterized in hatched chicken eggs by John Franklin Enders in 1945 . In 1954, the then unusual mumps virus morphology was first examined under the electron microscope .
The mumps virus has a lipid-containing virus envelope that surrounds a twisted, helical capsid . This structure explains the sensitivity of the mumps virus to mild soaps and dehydration. The virus is distributed worldwide as a uniform serotype and has no animal reservoir .
morphology

The virion of the mumps virus appears round to irregular with a mean diameter of 150 nm. The virus envelope contains two envelope proteins (F1 and F2), of which F1 has hemagglutinin and neuraminidase activity. F1 and F2 coalesce as heterodimers and form the fusion protein that is active in this way for entry into the cell. The inside of the envelope is covered by a matrix protein that enables the virus particle to assemble as it exits the cell membrane .
The helical capsid encloses the viral RNA and consists of four different capsid proteins, predominantly the N protein (N: nucleocapsid). The presence of the N-protein is also required for the transcription of the viral RNA. A molecule of the viral RNA polymerase is also packaged inside the virion in order to synthesize a complementary (+) RNA immediately after entering the cell.
Genome
The genome of the mumps virus is a single, linear strand of RNA with negative polarity (ss (-) RNA) and a length of 15,384 nt . The genome contains nine open reading frames (ORF) that code for eight viral proteins : nucleo- (N), phospho- (P), matrix (M), fusion protein (F), large protein (L), V proteins as well a small, hydrophobic (SH) protein. It also encodes a hemagglutinin neuraminidase (HN). The SH protein prevents the infected cell from going into apoptosis . The V protein is only detectable in infected cells and prevents the activation of an interferon-induced antiviral response.
The ORFs are arranged one after the other without overlapping and are separated by short non-coding areas. At the ends of the RNA strand there is neither a 5'-cap structure nor a poly-A tail .
Subtypes and vaccine strains
Several genetically slightly different subtypes of the mumps virus have been isolated worldwide, but they do not differ either in terms of disease or serological response; the mumps virus is thus present in only one worldwide serotype , despite small variants . Some natural strains or strains grown in cell culture are used in a weakened form as attenuated live vaccines for protective vaccination ( mumps vaccine ). In Germany, the vaccine is mainly made from the Jeryl-Lynn strain, which is propagated in incubated chicken eggs. While the mumps infection leaves lifelong immunity, a single vaccination cannot always induce it. The plasma concentration of the specific antibodies (IgG) against the mumps virus drops very quickly and over the course of several years are often only poorly or not at all detectable in the current test procedures; this disappearance of the detectability of the mumps IgG is not necessarily a sign of non-existent cellular immunity.
- Species mumps virus
- Subtype mumps virus strain Belfast
- Subtype mumps virus strain Bristol
- Subtype mumps virus strain Edinburgh 2
- Subtype mumps virus strain Edinburgh 4
- Subtype mumps virus strain Edinburgh 6
- Subtype mumps virus strain Enders
- Subtype mumps virus strain Kilham
- Subtype mumps virus strain Matsuyama
- Subtype mumps virus strain RW
- Subtype mumps virus strain SBL
- Subtype mumps virus strain SBL-1
- Subtype mumps virus strain Takahashi
- Subtype mumps virus strain Jeryl-Lynn
- Subtype mumps virus strain L-Zagreb
- Subtype mumps virus strain Urabe
- Subtype mumps virus strain Miyahara vaccine
- Subtype mumps virus strain Urabe vaccine AM9
Reporting requirement
In Germany, the direct or indirect proof of the mumps virus must be reported by name in accordance with Section 7 of the Infection Protection Act if the proof indicates an acute infection.
swell
- S. Mordrow, D. Falke, U. Truyen: Molecular Virology , Heidelberg Berlin, 2nd edition 2003
- RA Lamb et al .: Genus Rubulavirus . In: CM Fauquet, MA Mayo et al .: Eighth Report of the International Committee on Taxonomy of Viruses , London, San Diego, 2005, pp. 659f
Individual evidence
- ↑ ICTV Master Species List 2018b.v2 . MSL # 34, March 2019
- ↑ a b ICTV: ICTV Taxonomy history: Akabane orthobunyavirus , EC 51, Berlin, Germany, July 2019; Email ratification March 2020 (MSL # 35)
- ^ JH Levens and JF Enders: The hemoagglutinative properties of amniotic fluid from embryonated eggs infected with mumps virus . In: Science (New York, NY) . tape 102 , no. 2640 , August 3, 1945, p. 117-120 , doi : 10.1126 / science.102.2640.117 , PMID 17777358 .
- ^ BG Ray and RH Swain: An investigation of the mumps virus by electron microscopy . In: The Journal of Pathology and Bacteriology . tape 67 , no. 1 , January 1954, p. 247-252 , doi : 10.1002 / path.1700670130 , PMID 13152639 .
- ↑ a b T. Betáková et al .: Overview of measles and mumps vaccine: origin, present, and future of vaccine production . In: Acta Virologica . tape 57 , no. 2 , 2013, p. 91-96 , doi : 10.4149 / av_2013_02_91 , PMID 23600866 .
- ↑ Gaynor Watson-Creed et al .: Two successive outbreaks of mumps in Nova Scotia among vaccinated adolescents and young adults . In: CMAJ: Canadian Medical Association journal = journal de l'Association medicale canadienne . tape 175 , no. 5 , August 29, 2006, p. 483-488 , doi : 10.1503 / cmaj.060660 , PMID 16940266 , PMC 1550754 (free full text).
- ^ Sari Jokinen et al .: Cellular immunity to mumps virus in young adults 21 years after measles-mumps-rubella vaccination . In: The Journal of Infectious Diseases . tape 196 , no. 6 , September 15, 2007, p. 861-867 , doi : 10.1086 / 521029 , PMID 17703416 .