Sickle cell disease
| Classification according to ICD-10 | |
|---|---|
| D57.0 | Sickle cell anemia with crises
Hb-SS disease with crises |
| D57.1 | Sickle cell anemia without crises |
| D57.2 | Double heterozygous sickle cell disease |
| D57.3 | Sickle cell genetic makeup
Heterozygous hemoglobin S. |
| D57.8 | Other sickle cell diseases |
| ICD-10 online (WHO version 2019) | |
The sickle cell disease (also sickle cell (s) anemia ) or drepanocytosis is an inherited disease of the red blood cells ( erythrocytes ). It belongs to the group of hemoglobinopathies (disorders of hemoglobin ) and leads to corpuscular hemolytic anemia . Those affected have a mutation in the β chain of hemoglobin. Either all β-chains can be affected (severe, homozygous form) or only a part (milder, heterozygous form).
The disease occurs mainly in people from Sub-Saharan Africa and their descendants, but also in parts of the Mediterranean and the Middle East as far as India and has spread globally through migration. It is still associated with high mortality in developing countries . The disease was described by James Herrick and Ernest Lyons in a patient from the Caribbean in 1910 , and the term sickle cell anemia was first used by Vernon Mason in 1922.
properties
Those affected produce abnormal hemoglobin ( sickle cell hemoglobin , HbS ), which tends to form fibrils when there is a lack of oxygen . The red blood cells are deformed into sickle-shaped structures by the fibers they contain, clump together and clog small blood vessels, which causes inflammation . In the homozygous form, clumping and vascular blockage can lead to attack-like, painful, sometimes life-threatening circulatory disorders ( sickle cell crises ), which among other things can lead to venous thrombosis . People affected by heterozygous diseases, in whom only one of the two hemoglobin genes is changed, are protected from the severe forms of malaria . As a result, the mutated hemoglobin gene is relatively common in malaria areas.
The destruction of red blood cells leads to severe chronic anemia ( haemolytic anemia ). Due to the tendency of hemoglobin S to polymerize and the sickle-shaped deformation of the erythrocytes, small arteries become occluded with recurrent circulatory disorders . This leads to severe pain and damage to multiple organ systems: brain ( ischemic stroke ), splenic infarction , lungs ( pneumonia , pulmonary hypertension ), eye , heart and kidney failure , muscle , bone ( osteonecrosis ) or priapism . The life expectancy is reduced. A glomerulopathy with hyperfiltration occurs in up to one third of patients with homozygous phenotype in childhood. Damage to the renal medulla leads to papillary necrosis , loss of the kidneys' ability to concentrate and bloody urine (macrohematuria) . Damage to the kidney corpuscles (glomeruli) leads to increased protein excretion in the urine ( micro and macro albuminuria , nephrotic syndrome ). In the histological examination , the predominant glomerular damage is focal segmental glomerulosclerosis . Proteinuria occurs in up to a third of patients in the first decades of life, and terminal kidney failure in five percent.
Only homozygous carriers of the sickle cell gene show this severe form of the disease, in which all of the hemoglobin is abnormal sickle cell hemoglobin (irregular hemoglobin). In heterozygous carriers, only about one percent of all erythrocytes are deformed. Symptoms are significantly worse when people are physically active or at high altitudes. This is because the sickle shape of the erythrocytes forms when the oxygen partial pressure is low , because under these conditions the hemoglobin is fibrous (the solubility of hemoglobin in sickle cell anemia is 25 times less than the solubility of normal hemoglobin).
Symptoms can appear for the first time from around the age of six months, when the breakdown of fetal hemoglobin is already well advanced. They are then usually expressed in what is known as a sickle cell crisis: External influences such as exertion reduce the oxygen partial pressure in the blood, and the sickle cells become hemolytic .
root cause
Due to a point mutation in the HBB gene (c.20A> T) on chromosome 11 is in sickle cell anemia at position six of the β-globin - protein subunit of hemoglobin, the amino acid glutamic acid by valine replaced. The designation of this variant in the official genetic nomenclature is HBB-p.E6V. The affected erythrocytes become sickle-shaped with decreasing oxygen partial pressure, easily get caught in the capillaries and moreover lyse very quickly. By hemolysis are hemoglobin , arginase and free oxygen radicals released. Free hemoglobin binds nitric oxide about 1000 times more strongly than intracellular, and arginase converts nitric oxide to nitrite and nitrate. Nitric oxide is the most important vasodilator , and the decrease in concentration leads to vasoconstriction and thus to circulatory disorders.
Sickle cell hemoglobin is referred to as HbS in contrast to HbA, the normal hemoglobin of adults. In addition to HbS, heterozygous carriers of the trait also produce HbA in sufficient quantities to largely maintain the function of the erythrocytes in these people.
Using sickle cell anemia as an example, the connection between a defect in a molecule and a disease was demonstrated for the first time in a famous work by Linus Pauling , Harvey Itano and Seymour Jonathan Singer from 1949. The difference in the hemoglobin of the two red blood cells was shown in gel electrophoresis , which Itano performed. The authors already suspected that there were differences in the amino acids, which Vernon Ingram confirmed in 1956, who also showed that the difference consisted in exchanging exactly one amino acid. James Van Gundia Neel (1915–2000) also clarified the inheritance pattern of the disease in 1949 .
Inheritance
Sickle cell anemia is an autosomal codominant hereditary disease .
- The genetic makeup of a healthy person contains the two incompletely dominant (A and S are codominant at the molecular level) alleles (AA) for hemoglobin A. His red blood cells are always elastic.
- A transmitter (conductor) with the genotype AS (= heterozygous ) contains both the allele A and the mutated allele S, which causes the changed hemoglobin S. Its red blood cells contain HbA and HbS in a 1: 1 ratio. Under normal conditions, the red blood cells show no changes, the disease does not break out. Only when there is a very strong lack of oxygen do the red blood cells deform into sickle-shaped structures, which impairs the blood flow to the organs.
- A carrier of the genotype SS ( homozygous ) only produces the modified HbS. Even under a physiological lack of oxygen, as it is for. B. in the capillaries of oxygen-consuming organs, there is a strong deformation of the red blood cells. They lose their elasticity and easily get caught in one another. This leads to a closure of the capillaries. Under normal conditions, the hemoglobin in the red blood cells is always finely divided. When the pH value and oxygen content of the blood decrease, the hemoglobin molecules clump together to form rod-shaped, crystalline structures in HbS. This causes the erythrocyte to become sickle-shaped and lose its elasticity.
diagnosis
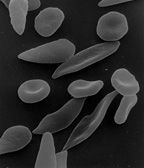
The diagnosis of sickle cell anemia is initially based on anamnestic , whereby the origin and other cases of the disease in the family should be inquired about; then clinically based on the symptoms and finally in the laboratory, where hemolytic anemia can appear in a blood count and the typically shaped drepanocytes appear when the blood is examined under the microscope - especially if the blood has been stored under the exclusion of oxygen for 24 hours (sickle cell test). In addition, electrophoresis of the hemoglobin can conclusively identify the changed molecules. Finally, the gene segment for hemoglobin can also be examined in a restriction analysis and the point mutation can be shown at the level of the DNA.
Family tree analysis
If the genotypes of the parents are known, the Hardy-Weinberg law can be used to calculate the probability that sickle cell anemia will occur in a child:
| Parent genotype | Children's genotypes | Inheritance probabilities and phenotype of children | |
|---|---|---|---|
| AA x AA | AA | 100% | healthy children |
| AA × AS | AA | 50% | Probability that a child is healthy |
| AS | 50% | Chances of a child becoming a heterozygous HbS carrier | |
| AS × AS | AA | 25% | Probability that a child is healthy |
| AS | 50% | Chances of a child becoming a heterozygous HbS carrier | |
| SS | 25% | The likelihood of a child having the more severe, homozygous form | |
| AA × SS | AS | 100% | all children become heterozygous carriers of HbS |
| AS × SS | AS | 50% | Chances of a child becoming a heterozygous HbS carrier |
| SS | 50% | The likelihood of a child having the more severe, homozygous form | |
| SS × SS | SS | 100% | The children certainly have the more severe, homozygous form |
Sickle cell test
The blood to be examined is mixed with EDTA and stored for 24 hours under the exclusion of oxygen. As a result of the lack of oxygen in the erythrocytes, the sickle shapes of the cells develop, which can be easily recognized under the microscope at 40x magnification. In addition, the sickle cell formation effect can be accelerated by adding sodium disulfite ( sodium metabisulfite ).
Electrophoresis
Since a change in the red blood cells of vectors (genotype AS) only occurs under extreme oxygen deficiency, the genotype AA cannot be distinguished from the genotype AS by examining the red blood cells under the microscope . In contrast, the genotype can be clearly determined with the help of electrophoresis : blood is taken from the test subjects and processed until pure hemoglobin is available. This is applied to a gel. The two types of hemoglobin migrate differently in the electric field , as HbS shows a different migration behavior due to its changed protein structure.
Molecular genetics
The causal mutation in the HBB gene (c.20A> T) can be detected using molecular biological testing methods. The sequencing of the HBB gene is increasingly replacing other methods such as restriction analysis .
distribution
It is noticeable that the sickle cell allele is relatively common in areas of malaria . It was concluded from this that it confers a resistance against malaria , so that the healthy carriers (AS) of the sickle cell allele in these areas have a selection advantage (the so-called heterozygote advantage ) over those without sickle cell alleles (genotype AA), who are more likely to die of malaria, and also over the Sickle cell disease (SS genotype) who die prematurely from sickle cell anemia. For example, in Africa there are areas where nearly a third of the population is heterozygous for this trait. In other parts of the world the sickle cell allele is practically non-existent, as this selection advantage is not effective here due to the lack of malaria. In Germany, between 500 and 1100 cases of malaria are found each year. About 85% of homozygous carriers come from Africa.
Reliable data on the frequency in Germany are not available. The total number of sickle cell disease patients living in Germany was estimated to be at least 2000 for 2017.
Significance of sickle cell anemia in malaria
There may be a selective advantage of heterozygous carriers in infections with malaria . The malaria pathogen is transported to or in the erythrocytes during part of its development cycle. The hemoglobin of people with the heterozygous form of HbS leads, by reducing the oxygen saturation of the hemoglobin under extreme conditions, to sickle-like deformation of the red blood cells, which are then broken down or clumped in the spleen and then perish. One hypothesis says that those cells that are infected by plasmodia would deform themselves through the influence of the merozoites or trophozoites , even without this reduction in pressure, and would be recognized and broken down by the spleen.
Another hypothesis is the direct killing of the parasites, because the sickle cells produce more oxygen radicals. Superoxide anions and hydrogen peroxide are produced , and both compounds are toxic to the parasites.
Another theory says that if the plasmodia that cause malaria attack erythrocytes, the microbes release acids as waste products of their metabolism over time. The hemoglobin now releases the oxygen, stimulated by H + ions (shift to the right of the oxygen binding curve ). The sickle shape primarily affects the deoxy shape of the erythrocytes. So the infected cells quickly become sickle cells, and these are then broken down in the spleen along with the microbes. This explains the resistance of the carriers of sickle cell anemia to malaria (see figure).
The last theory states that hemoglobin polymers are formed in the process, which in turn leads to the direct killing of the parasites.
therapy
Currently, approaches to enhance the gene expression of HbF studied in adolescents and adults.
Hydroxyurea can induce the formation of HbF. Red blood cells with a high proportion of HbF do not form sickle cells and are therefore less likely to break down and cause occlusions of small vessels. Treatment with hydroxyurea can reduce the frequency of vascular occlusions, alleviate chronic organ damage, and extend survival. This was recently shown to children in sub-Saharan Africa .
Furthermore, adoptive cell transfer is being investigated.
On October 12, 2016, a treatment option based on a change in the affected genes using the CRISPR / Cas method was published. With the help of gene scissors, the researchers replaced the pathogenic mutation with the correct DNA bases. For the first time, enough healthy blood cells were generated to be able to cure patients with this method in the future, as reported by researchers working with Jacob Corn from the University of California , Berkeley. It is still too early to speak of a workable solution, but the first step has been taken to combat the causes instead of treating the symptoms.
Other drugs are the oxygen affinity modulator voxelotor and the monoclonal antibody crizanlizumab .
literature
- Fernando Ferreira Costa, Nicola Conran (Ed.): Sickle Cell Anemia. From Basic Science to Clinical Practice , Springer 2016
Web links
- Detailed practical guide from the University of Bonn
- Sickle Cell Disease (English) Harvard University website on sickle cell disease
- Sickle Cell Anemia (English) Full site from US National Library of Medicine and National Institutes of Health
- Sickle Cell Disease Website of the Cold Spring Harbor Laboratory with lots of animations and videos
- IST eV - Sickle Cell Disease and Thalassemia Interest Group
- deutschlandfunk.de Science in focus December 16, 2018, Thomas Reintjes : Experimental therapies for sickle cell patients
Individual evidence
- ↑ Compact Lexicon Biology, Spectrum Academic Publishing House
- ↑ Frederic Piel, Thomas Williams, Sickle Cell Anemia: History and Epidemiology . In: Fernando Ferreira Costa, Nicola Conran (eds.): Sickle Cell Anemia. From Basic Science to Clinical Practice . Springer, 2016, p. 24.
- ^ Piel, Williams, in Costa, Conran, Sickle Cell Anemia, Springer 2016, p. 24
- ^ Herrick, Peculiar elongated and sickle-shaped red blood corpuscles in a case of severe anemia, Arch. Int. Med., Vol. 6, 1910, pp. 517-521.
- ↑ Vernon Mason, Sickle Cell Anemia, J. Am. Med. Assoc., Vol. 79, 1922, pp. 1318-1320.
- ↑ K. Sun, Y. Xia: New insights into sickle cell disease: a disease of hypoxia. In: Current Opinion in Hematology . Volume 20, Number 3, May 2013, pp. 215-221, ISSN 1531-7048 . doi: 10.1097 / MOH.0b013e32835f55f9 . PMID 23549375 .
- ↑ E. Sparkenbaugh, R. Pawlinski: Interplay between coagulation and vascular inflammation in sickle cell disease. In: British Journal of Hematology . Volume 162, Number 1, July 2013, pp. 3-14. doi: 10.1111 / bjh.12336 . PMID 23593937 . PMC 3878906 (free full text).
- ^ BE Gee: Biologic complexity in sickle cell disease: implications for developing targeted therapeutics. In: TheScientificWorldJournal. Volume 2013, 2013, p. 694146, ISSN 1537-744X . doi: 10.1155 / 2013/694146 . PMID 23589705 . PMC 3621302 (free full text).
- ↑ MY Lim, KI Ataga, NS Key: Hemostatic abnormalities in sickle cell disease. In: Current opinion in hematology. Volume 20, Number 5, September 2013, pp. 472-477, ISSN 1531-7048 . doi: 10.1097 / MOH.0b013e328363442f . PMID 23817169 .
- ↑ S. Sheth, M. Licursi, M. Bhatia: Sickle cell disease: time for a closer look at treatment options? In: British Journal of Hematology . Volume 162, Number 4, August 2013, pp. 455-464, ISSN 1365-2141 . doi: 10.1111 / bjh.12413 . PMID 23772687 .
- ^ Harrison's Internal Medicine, 15th Edition, p. 1754.
- ↑ Raimund Hirschberg: Glomerular filtration hyper in sickle cell disease . In: Clinical Journal of the American Society of Nephrology . 5, No. 5, May 2010, ISSN 1555-905X , pp. 748-749. doi : 10.2215 / CJN.01340210 . PMID 20299367 .
- ↑ a b NM_000518.5 (HBB): c.20A> T (p.Glu7Val) AND HEMOGLOBIN S - ClinVar - NCBI. Retrieved April 10, 2020 .
- ↑ L. Pauling, Harvey A. Itano, SJ Singer, Ibert C. Wells: Sickle Cell Anemia, a Molecular Disease, Science, Volume 110, 1949, pp. 543-548
- ↑ D. Lowe, Das Chemiebuch, Librero 2017, p. 354
- ↑ Microsoft PowerPoint - Transfusion Medicine and Migration - Prof. R. Heinz.ppt - Heinz.pdf . Retrieved February 3, 2014.
- ↑ Dietmar P. Berger, Rupert Engelhardt, Roland Mertelsmann : The Red Book: Hematology and Internal Oncology . Hüthig Jehle Rehm, December 11, 2013, ISBN 978-3-609-51218-1 .
- ↑ Sickle Cell Anemia - HBB - Human Genetics - Analysis Spectrum - Lademannbogen Laboratory. Retrieved April 10, 2020 .
- ↑ 2013 - 43 13.pdf . In: Epidemiological Bulletin . Retrieved February 3, 2014.
- ↑ TN Williams, SK Obaro: Sickle cell disease and malaria morbidity: a tale with two tails. In: Trends in parasitology. Volume 27, Number 7, July 2011, pp. 315-320, ISSN 1471-5007 . doi: 10.1016 / j.pt.2011.02.004 . PMID 21429801 .
- ↑ Joachim B. Kunz, Stephan Lobitz, Regine Grosse, Lena Oevermann, Dani Hakimeh: Sickle cell disease in Germany: Results from a national registry . In: Pediatric Blood & Cancer . tape 67 , no. 4 , 2020, ISSN 1545-5017 , p. e28130 , doi : 10.1002 / pbc.28130 .
- ↑ JI Malowany, J. Butany: Pathology of sickle cell disease. In: Seminars in diagnostic pathology. Volume 29, Number 1, February 2012, pp. 49-55, ISSN 0740-2570 . PMID 22372205 .
- ↑ AU Orjih, R. Chevli, CD Fitch: Toxic heme in sickle cells: an explanation for death of malaria parasites . In: The American journal of tropical medicine and hygiene . 34, No. 2, March 1985, ISSN 0002-9637 , pp. 223-227. PMID 3885769 .
- ↑ Script of the Harvard Medical School ( Memento of the original from November 27, 2011 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. (English)
- ↑ I. Akinsheye, A. Alsultan, N. Solovieff, D. Ngo, CT Baldwin, P. Sebastiani, DH Chui, MH Steinberg: Fetal hemoglobin in sickle cell anemia. In: Blood . Volume 118, Number 1, July 2011, pp. 19-27. doi: 10.1182 / blood-2011-03-325258 . PMID 21490337 . PMC 3139383 (free full text).
- ↑ OS Platt, SH Orkin, G Dover, GP Beardsley, B Miller: Hydroxyurea enhances fetal hemoglobin production in sickle cell anemia . In: The Journal of Clinical Investigation . tape 74 , no. 2 , 1984, ISSN 0021-9738 , pp. 652–656 , doi : 10.1172 / JCI111464 , PMID 6205021 , PMC 370519 (free full text).
- ↑ Winfred C Wang, Russell E Ware, Scott T Miller, Rathi V Iyer, James F Casella: Hydroxycarbamide in very young children with sickle-cell anemia: a multicentre, randomized, controlled trial (BABY HUG) . In: Lancet (London, England) . tape 377 , no. 9778 , May 14, 2011, ISSN 1474-547X , p. 1663–1672 , doi : 10.1016 / S0140-6736 (11) 60355-3 , PMID 21571150 , PMC 3133619 (free full text).
- ↑ Ersi Voskaridou, Dimitrios Christoulas, Antonios Bilalis, Eleni Plata, Konstantinos Varvagiannis: The effect of prolonged administration of hydroxyurea on morbidity and mortality in adult patients with sickle cell syndromes: results of a 17-year, single-center trial (LaSHS) . In: Blood . tape 115 , no. 12 , March 25, 2010, ISSN 1528-0020 , p. 2354-2363 , doi : 10.1182 / blood-2009-05-221333 , PMID 19903897 .
- ↑ Léon Tshilolo, George Tomlinson, Thomas N Williams, Brígida Santos, Peter Olupot-Olupot: Hydroxyurea for Children with Sickle Cell Anemia in Sub-Saharan Africa . In: New England Journal of Medicine . tape 380 , no. 2 , January 10, 2019, ISSN 0028-4793 , p. 121-131 , doi : 10.1056 / NEJMoa1813598 .
- ↑ C. Oringanje, E. Nemecek, O. Oniyangi: Hematopoietic stem cell transplantation for people with sickle cell disease. In: The Cochrane database of systematic reviews. Volume 5, 2013, pp. CD007001, ISSN 1469-493X . doi: 10.1002 / 14651858.CD007001.pub3 . PMID 23728664 .
- ↑ http://www.nature.com/news/crispr-deployed-to-combat-sickle-cell-anaemia-1.20782
- ↑ http://www.scinexx.de/wissen-aktuell-20717-2016-10-13.html
- ↑ OXBRYTA voxelotor tablet, film coated . DailyMed .
- ↑ ADAKVEO-crizanlizumab injection . DailyMed .