Alexander disease
| Classification according to ICD-10 | |
|---|---|
| E75. 2 | Other sphingolipidoses |
| ICD-10 online (WHO version 2019) | |
The Alexander's disease (Crohn's Alexander) is a rare disease from the group of leukodystrophies . It is a genetic disorder in which there is progressive degeneration of the white matter of the brain and spinal cord. Clinically, Alexander's disease often makes itself felt in infancy with a delay in psychomotor development and an increase in the size of the skull . Cause of the disease occurring in the structural changes of the supporting cells of the brain ( astrocytes ) and a demyelination are usually spontaneously occurring dominant mutations of the GFAP gene encoding a astrozytäres structural protein , the glial fibrillary acidic protein , encoded . The disease cannot be cured. As a rule, sick small children do not survive the age of six.
Historical aspects
The disease was named after the New Zealand pathologist William Stewart Alexander , who, as a young doctor in London with the neuropathologist Dorothy Stuart Russell (1895–1983), had worked through the autopsy of a 15-month-old child and who first described the disease in 1949.
Epidemiology
The majority of cases of illness occur sporadically, i.e. without familial accumulation. In the majority of patients, Alexander's disease begins in infancy, with girls appearing to develop the disease slightly more often than boys. The disease is very rare and has so far been confirmed by molecular genetics in around 150 patients.
Clinical picture
Depending on the age of onset, different forms of Alexander's disease can be distinguished.
The infantile form that occurs in children is the most common. The disease becomes noticeable around six months of age, but can also set in between the first and 24th month of life. The unspecific leading symptom in affected children is a pronounced disorder of motor and mental development. Enlargement of the skull ( macrocephalus ) and brain ( macroencephaly ), problems with feeding, swallowing disorders, ataxia , spasticity and seizures may also occur.
The neonatal form (in newborns) shows the fastest progressing course with the worst prognosis.
The juvenile form (in adolescents) is milder, the patients do not always have macrocephaly, and the neurological deficits appear later.
In the adult form , which occurs in adults, the extent of degenerative changes in the white matter is less and bulbar symptoms with swallowing and speech disorders are often in the foreground, since the brain stem is particularly affected. Myoclonus of the soft palate can occur.
Diagnosis
The disease cannot be diagnosed clinically, that is, not based on a physical examination alone. Rather, technical investigation procedures are necessary. Until a few years ago, biopsy or autopsy detection of the pathological changes in the brain tissue characteristic of Alexander's disease was necessary to confirm the diagnosis. Since the responsible gene was characterized, DNA analyzes have increasingly been carried out in suspected cases . A magnetic resonance tomography examination of the brain can also allow differentiation from other diseases. The following neuroradiological criteria have been suggested for the diagnosis of childhood disease:
- Extensive frontal medullary changes
- A periventricular border ( signal-intensive in the T1 weighting )
- A periventricular border ( low signal on the T2-weighted image)
- Changes in the basal ganglia , thalamus, and brain stem
- Enrichment of contrast media in certain brain regions
In the presence of four of the five criteria, the diagnosis of Alexander's disease is considered likely. In the adult form, atrophy and signal changes can be demonstrated in the area of the brain stem and spinal cord .
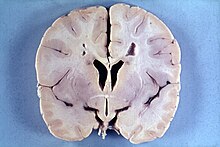
pathology
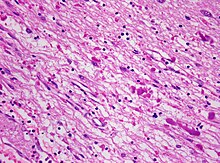
Alexander's disease is primarily a disease of the astrocytes , supporting cells of the brain ( glia ), whose intermediate filament GFAP is incorrectly formed . When combined with other proteins, astrocytic inclusions known as Rosenthal fibers are formed. In the case of the disease, Rosenthal fibers can be detected as fine tissue in the entire central nervous system (brain and spinal cord ), but are preferably found periventricular and in the vicinity of blood vessels . Electron microscopy shows a close connection between the Rosenthal fibers and intermediate filaments .
In addition, there is poor myelination in children and demyelination in older patients . Both sensory and motor nerve fibers are affected. Myelinization disorder is often accompanied by macrocephaly and sometimes hydrocephalus , especially in young children .
The distribution pattern of the demyelinated areas does not agree with that of the Rosenthal fibers; So myelination disorder and fiber formation appear to be independent manifestations of the disease. It is believed that changes in the astrocytes are secondary to myelination disorder.
genetics
The autosomal dominant Alexander disease is usually caused by spontaneously occurring mutations in the GFAP gene, which codes for an astrocytic intermediate filament, the acidic glial fiber protein. A GFAP mutation can be detected in about 94% of cases, and a large number of different mutations have been described. These mostly concern changes in amino acid residues that are evolutionarily highly conserved and are responsible for the dimerization of proteins and the formation of microfilaments. Apparently, there is a connection between the type of genetic change and the severity of the disease, the phenotype : patients with a point mutation (R79H) affecting codon 79 are generally less seriously ill than patients with codon 239.
Individual families have been described in which several children of healthy parents fell ill. In these rare cases there is presumably either an autosomal recessive inheritance or a germline mosaicism with transmission of the dominant mutation in cells of the germline of healthy parents. In fact, the GFAP mutation appears to predominantly affect the father's allele , suggesting that the mutation occurred during sperm formation . Genetic counseling is therefore recommended to parents of affected children if they continue to want to have children .
Prognosis and therapy
Despite the clarification of the underlying mutation, no cure has yet been possible and treatment of Alexander's disease is therefore exclusively symptom-related and supportive. Children who develop Alexander disease as young children typically do not survive the age of six.
Veterinary medicine
A fibrinoid leukodystrophy, which is clinically similar to the human Alexander disease, is described as a single case description in two Labrador retrievers as well as a Scottish terrier , a miniature poodle and a Bernese mountain dog . The cases occurred between the ages of 13 weeks and nine months and resulted in progressively worsening ataxia . The prognosis is poor and hopeless .
literature
- Rodriguez: Alexander disease. In: Orphanet Encyclopedia. 2004. (Review) (full text as PDF) ( Memento from November 17, 2008 in the Internet Archive )
- Harding & Surtees: Metabolic and neurodegenerative disease of childhood. In: David I. Graham et al. (Ed.): Greenfield's Neuropathology. 7th edition. Arnold, London 2002, ISBN 0-340-74231-3 .
Web links
- ELA - European Association against Leukodystrophy The patient association offers in-depth information and provides medical contacts for Alexander's disease and other leukodystrophies.
- Alexander disease. In: Online Mendelian Inheritance in Man . (English)
- Alexander disease in Orphanet
- Resources to research and molecular genetics of Alexander disease of the University of Wisconsin-Madison
- Gabriele Eisenrieder: Death has its own room . Case history, Berliner Morgenpost from November 15, 2008.
- Susanne Kailitz: Ben's message . Case history, Die Zeit, January 19, 2014.
Individual evidence
- ↑ Scolding: myelin Regenerating. In: Brain. 2004; 127, pp. 2144-2147, PMID 11673315 ( full text ).
- ↑ Alexander: Progressive fibrinoid degeneration of fibrillary astrozytes associated with mental retardation in a hydrocephalic infant. In: Brain. 1949; 72, pp. 373-381, PMID 15409268 (first description).
- ↑ on the basis of this bibliography ( Memento of December 3, 2008 in the Internet Archive ).
- ↑ Pareyson et al.: Adult-onset Alexander disease: a series of eleven unrelated cases with review of the literature. In: Brain. 2008; 131 (Pt 9), pp. 2321-2331, PMID 18684770 .
- ^ Van der Knaap et al: Alexander disease: diagnosis with MR imaging. In: AJNR Am J Neuroradiol. 2001; 22 (3), pp. 541-552, PMID 11237983 ( full text ).
- ↑ Farina et al: Can MR imaging diagnose adult-onset Alexander disease? In: AJNR Am J Neuroradiol. 2008; 29 (6), pp. 1190-1196, PMID 18388212 .
- ↑ Brenner et al.: Mutations in GFAP, encoding glial fibrillary acidic protein, are associated with Alexander Disease. In: Nature Genetics . 2001; 27, pp. 117-120, PMID 11138011 .
- ↑ Gorospe: Alexander disease. In: Gene Reviews. ( Full text )
- ↑ a b c Rodriguez et al: Infantile Alexander disease: spectrum of GFAP mutations and genotype-phenotype correlation. In: Am J Hum Genet. 2001; 69 (5), pp. 1134-1140, PMID 11567214 .
- ↑ Wohlwill include: Dysmyelinogenic leukodystrophy; Report of a case of a new, presumably familial type of leukodystrophy with megalobarencephaly. In: J Neuropathol Exp Neurol . 1959; 18 (3), pp. 359-383, PMID 13665382 .
- ^ Li et al: Propensity for paternal inheritance of de novo mutations in Alexander disease. In: Hum Genet. 2006; 119, pp. 137-144, PMID 16365765 .
- ↑ Fibrinoid leukodystrophy. In: Merck Veterinary Manual. Retrieved June 3, 2011.