Lichen planus mucosae
| Classification according to ICD-10 | |
|---|---|
| L43 | Lichen planus (excl. Lichen pilaris) |
| ICD-10 online (WHO version 2019) | |
The Lichen Planus is the mucosal manifestation of lichen planus (short: Lichen planus or lichen planus , including: lichen ). In the context of a generalized disease or in isolation, lesions usually develop on the mucous membranes of the oral cavity or the genital and anal area, more rarely also the eyes, the nasopharynx, the esophagus and the urinary tract. As with the cutaneous variant of the disease, there is a great morphological diversity, but the most common are white papules or net-like stripes as well as erosions of the mucous membrane.
The diagnosis can usually be made as part of a dental, gynecological or urological examination, if necessary also by taking a tissue sample; if the esophagus is involved, a reflection of the upper digestive tract is required. Cortisone preparations are usually used therapeutically . Since the course of the disease is often chronic, the treatment essentially serves to control symptoms and avoid late effects. This also includes the development of squamous cell carcinoma (white skin cancer).
distribution
Data on the prevalence of oral lichen planus vary between 0.9% and 1.27% of the general population. Lesions of the oral mucosa occur in approx. 60% of the cases of a generalized lichen planus, a pure involvement of the oral mucosa accounts for approx. 15–35% of the cases of an oral lichen planus. In contrast to the cutaneous form of lichen planus, women are affected significantly more frequently than men; the typical age of onset is the seventh decade of life.
Anogenital lesions occur in around 25 to 40% of cases in the context of a classic lichen planus. In women, skin and vulva are simultaneously involved in about 50% of cases.
Mucosal lesions outside the oral cavity and genital area are rare.
root cause
As with the cutaneous variant of lichen planus, the etiology is not fully understood. The disease is based on an autoimmune process that can be triggered by various factors. This includes:
Genetics: Carriers of certain class II HLA genes responsible for regulating the individual immune response are more frequently affected by the disease than other people.
Allergic reactions: the oral lichen planus is related to dental fillings, especially amalgam .
Infections: local bacterial infections of the oral mucosa and systemic infections with human papilloma (HPV) or hepatitis C viruses (HCV) are risk factors for oral lichen planus.
Medication: Lichen planus-typical lesions of the oral mucosa can be caused by various medications.
Disease emergence
The causal factors trigger an autoimmune process by causing a change in the surface structure of the keratinocytes (cells of the upper layer of the mucous membrane) or the changed presentation of antigens by antigen-presenting cells in the mucous membrane epithelium (upper layer of the mucous membrane). Keratinocytes and antigen-presenting cells then release inflammatory mediators , which in turn stimulate T lymphocytes , a subgroup of white blood cells, to migrate into the lamina propria (thin layer of connective tissue under the epithelium). The lymphocytes release further mediators, which lead to the death of keratinocytes in the lower cell layers of the epithelium.
Clinical appearance
Oral lichen planus
Lesions appear on the lips and mucous membrane of the cheeks, oral vestibule, gums, tongue, and hard and soft palates. Various clinical presentations are possible: typically, reticulate-streaky, whitish changes in the mucous membrane (Wickham striae) , often described as fern-like, appear , possibly with more or less papular or plaque-like parts (reticulopapular form). The changes occur symmetrically and particularly frequently on the cheek mucosa and are usually symptom-free.
In the erosive-erythematous form, originally vesicular or bullous (blistered) lesions lead to erosions (superficial mucosal defects) of the often reddened mucous membrane after opening . A diffuse manifestation of this form is also called desquamative gingivitis. The erosions can be painful.
The ulcerous form of oral lichen planus is accompanied by fibrinous ulcerations (deeper-reaching defects in the mucous membrane) of the oral mucosa, which are painful to the touch, alcohol or spicy foods.
Anogenital lichen planus
The most common form of manifestation in this location is the erosive lichen planus, but papular, annular or bullous lesions can also occur.
In women, erosions can be seen on the vulvar, vaginal and cervical mucosa , which may be surrounded by reticulated white stripes. Vulvar lesions can be accompanied by severe itching, but also burning pain and - if localized to the vagina - postcoital bleeding (occurring after sexual intercourse) can occur. If the lesions with scarring heal, vulvar adhesions and vaginal stenosis (narrowing of the vagina) can result.
In men, lesions often develop on the glans, with involvement of the foreskin possibly with phimosis (foreskin narrowing).
Wart-like hypertrophic lesions are more often found on the mucous membrane of the anal area, which in the case of ulceration can lead to painful fissures, possibly with secondary infections.
The simultaneous occurrence of erosive genital lichen planus with oral manifestations on the gingival mucosa (mucous membrane of the gums) is called vulvovaginal-gingival syndrome. It is an unusual picture that occurs even less often than penogingival syndrome in men.
Extracutaneous lichen planus
Overall rare, but most common among the manifestations in the digestive tract, is the lichen planus mucosae of the esophagus, which occurs mostly in women of middle or older age and usually occurs with oral lesions. It is usually associated with chronic pain and can lead to scarring with resulting strictures and stenoses (narrowing) of the esophagus.
Lesions on the eyes are even less common. Here they can manifest as ( kerato) conjunctivitis , ulceration of the cornea (cornea of the eye), iridocyclitis , chorioretinitis , blepharitis or lesions of the eyelids. As a rule, ocular lesions are associated with skin and / or other mucosal manifestations.
diagnosis
In addition to the anamnesis (taking the medical history), the diagnosis includes a clinical examination, whereby in the case of a primarily dermatological examination, manifestations in the oral cavity and in the genital area should also be inquired about and inspected. A more targeted examination of the oral cavity and urogenital tract is carried out as part of a dental, gynecological or urological examination.
If the diagnosis cannot be clinically confirmed, a biopsy (tissue sample) can be taken from abnormal mucous membrane for examination under the microscope. Specially in the case of erosive or ulcerative lesions, sampling is recommended from the edge area in order to capture assessable parts of the epithelium and to minimize the risk of an ulcer-inflammatory overlay of the disease-specific histomorphological features of the lichen planus mucosae. A biopsy examination should also be carried out in the case of permanent lesions, particularly those that persist under therapy. If a second tissue sample is taken from the lesional mucous membrane and sent unfixed to the laboratory, it can be examined using direct immunofluorescence . The examination method is not used in standard diagnostics, but in the case of vesicobuloid lesions it can facilitate the differential diagnosis to other blistering mucosal diseases.
If there is a corresponding clinical suspicion, e.g. B. Due to swallowing difficulties, an endoscopic examination should be performed to determine whether the esophagus is involved. An HCV test may also be performed for patients from regions with high HCV prevalence.
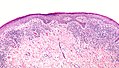
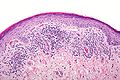
pathology
The reticulopapular form of oral lichen planus is usually associated with orthohyperkeratosis or parakeratosis (excessive cornification) as well as variable, possibly sawtooth-like acanthosis (widening of the stratum spinosum ) and hypergranulosis (widening of the stratum granulosum ) of the epithelium. In contrast, the erosive-erythematous form shows a non-keratinized or atrophic (narrowed) epithelium, possibly with erosions. Genital mucosal lesions can also show both acanthosis and atrophy. There is variable spongiosis (intraepithelial edema ) in both locations . In the basal cell layer (lower cell layer of the epithelium) and in the immediately subepithelial lamina propria there are dead keratinocytes (English: civatte bodies ), which, however, are less common in genital lesions.
As a result of the cell death, crevices can arise in the section along the border between the epithelium and lamina propria, which are mostly due to processing and must be distinguished from real bubbles. The basal keratinocytes obtained occasionally show inflammatory atypia. In oral lesions in particular, the basement membrane (boundary layer between the epithelium and the underlying lamina propria) can appear thickened due to the deposition of fibrinogen.
In the lamina propria there is a ribbon-like infiltrate of lymphocytes that also extends to the epithelium. In the case of gingival or genital lesions, the infiltrate usually contains not only lymphocytes but also plasma cells , which are also more common in erosive and allergic lesions of the oral mucosa. Long-standing genital lesions may only show a focal and sparse infiltrate.
Complications
Healing of the lesions associated with scarring can lead to adhesions and stenoses in the affected locations.
The development of squamous cell carcinoma (white skin cancer) of the oral or esophageal mucosa or the anogenital area is discussed as a further complication .
treatment
Since the course of the disease is often chronic, the therapy mainly serves to control symptoms and reduce complications.
Oral lichen planus
As a first line treatment are topical recommended cortisone preparations as a paste, lozenges, solution Pellett or spray. Local cortisone injections can be considered, especially in ulcerative lesions, but these are painful. Another option is topical retinoids . The recommended options for systemic therapy include orally administered cortisone preparations, alternatively retinoids or ciclosporin .
Calcineurin inhibitors ( tacrolimus and pimecrolimus , topical), sulfasalazine , azathioprine , hydroxychloroquine , methotrexate , mycophenolate mofetil and TNF-α inhibitors are suggested as second-line therapy .
In third-line therapy, cyclophosphamide , thalidomide , antibiotics , itraconazole , griseofulvin , dapsone , low molecular weight heparin , interferon (with simultaneous hepatitis C), PUV-A and a YAG laser treatment can be tried.
Supportive measures consist of replacing dental fillings made of amalgam and gold with other materials, professional teeth cleaning, good oral hygiene, avoiding nicotine, avoiding injuries to the oral mucosa, spicy foods, alcohol and stress and excitement. If necessary, psychological support can be a useful addition to symptomatic therapy.
Genital lichen planus
The main aim of treatment is to reduce or prevent scarring of the lesions that restricts their function.
The papulosquamous form of the lichen planus is usually self-limiting, so that local treatment with cortisone and skin care cream is usually sufficient for a few weeks.
In addition, the recommended first line therapy consists in the application of topical cortisone preparations, e.g. B. as a suppository. These are initially used in high doses, followed by maintenance therapy in lower doses or application frequency. Alternatively, low-dose tricyclic antidepressants can be used.
Calcineurin inhibitors (tacrolimus or pimecrilimus), local anesthetic gel or antihistamines are suggested as second-line therapy .
Because of the increased risk of genital squamous cell carcinoma, follow-up examinations and sensitization of the patient to the corresponding symptoms should be carried out.
literature
- Konrad Bork, Walter Burgdorf, Nikolaus Hoede: Oral mucous membrane and lip diseases: Clinic, diagnostics and therapy. Atlas and manual. Schattauer, 2008, ISBN 978-3-7945-2486-0 , Chapter 22: Lichen ruber planus, pp. 74-83, google.book
- SK. Edwards: European guideline for the management of balanoposthitis . In: Int JSTD AIDS , 2001, 12 (Suppl. 3), pp. 68-72.
- Rajani Katta: Diagnosis and Treatment of Lichen Planus . In: Am Fam Physician. , June 1, 2000, 61 (11), pp. 3319-3324, aafp.org
- G Kirtschig, SH Wakelin, F. Wojnarowska: Mucosal vulval lichen planus: outcome, clinical and laboratory features . In: Journal of the European Academy of Dermatology and Venereology , 2005, 19 (3), pp. 301-307.
- Laurence Le Cleach, Olivier Chosidow: Clinical practice: Lichen Planus . In: New England Journal of Medicine , 366: 8, February 23, 2012, pp. 723-732.
- G. Wagner, C. Rose, MM Sachse: Clinical variants of lichen planus . In: Journal of the German Dermatological Society , 2013, doi: 10.1111 / ddg.12031
- Alberto Rosenblatt, Homero Gustavo Campos Guidi, Walter Belda: Male Genital Lesions: The Urological Perspective . Springer-Verlag, 2013, ISBN 3-642-29016-7 Google Books pp. 93–95
- Hywel Williams, Michael Bigby, Thomas Diepgen, Andrew Herxheimer, Luigi Naldi, Berthold Rzany: Evidence-Based Dermatology . John Wiley & Sons, Chapter 22: Lichen planus, pp. 189 ff., 744 pages.
- S. Regauer: Vulvar and penile carcinogenesis: transforming HPV high-risk infections and dermatoses (lichen sclerosus and lichen planus) . In: Journal für Urologie und Urogynäkologie , 2012, 19 (2), pp. 22-25
- Libby Edwards, Peter J. Lynch: Genital Dermatology Atlas . Lippincott Williams and Wilkins, 2010, ISBN 978-1-60831-079-1 , 384 pp.
- Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. Volume 1 . Elsevier, no location 2020, ISBN 978-0-7020-7552-0 , p. 241-251, 433-435, 483-85 .
- D. Ioannides, E. Vakirlis et al .: EDF S1 Guidelines on the management of Lichen Planus. (PDF) In: European Dermatology Forum. Retrieved March 14, 2020 .
Web links
- Skin lexicon: Lichen planus (lichen planus). In: Online Dermatologist AppDoc. Retrieved March 9, 2020 .
- Dr. Angela Unholzer: Lichen planus (lichen planus). In: www.apotheken-umschau.de. Wort & Bild Verlag, October 10, 2018, accessed on March 9, 2020 .
Individual evidence
- ↑ Changchang Li, Xiaoqiong Tang, Xiaoyan Zheng, Shuqi Ge, Hao Wen: Global Prevalence and Incidence Estimates of Oral Lichen Planus: A Systematic Review and Meta-analysis . In: JAMA Dermatology . January 2, 2020, ISSN 2168-6068 , doi : 10.1001 / jamadermatol.2019.3797 ( jamanetwork.com [accessed February 8, 2020]).
- ^ BE McCartan, CM Healy: The reported prevalence of oral lichen planus: a review and critique: Prevalence of oral lichen planus . In: Journal of Oral Pathology & Medicine . tape 37 , no. 8 , July 9, 2008, p. 447-453 , doi : 10.1111 / j.1600-0714.2008.00662.x .
- ↑ Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. Volume 1 . Elsevier, no location 2020, ISBN 978-0-7020-7552-0 , p. 241 .
- ↑ Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. Volume 1 . Elsevier, no location 2020, ISBN 978-0-7020-7552-0 , p. 483 .
- ^ FM Lewis, M. Shah, CI Harrington: Vulval involvement in lichen planus: a study of 37 women . In: The British Journal of Dermatology . tape 135 , no. 1 , July 1996, ISSN 0007-0963 , pp. 89-91 , PMID 8776366 .
- ↑ P. Koch, FA Bahmer: Oral lesions and symptoms related to metals used in dental restorations: a clinical, allergological, and histologic study . In: Journal of the American Academy of Dermatology . tape 41 , 3 Pt 1, September 1999, ISSN 0190-9622 , p. 422-430 , doi : 10.1016 / s0190-9622 (99) 70116-7 , PMID 10459117 .
- ↑ Yun Sik Choi, Yunji Kim, Hye-Jung Yoon, Keum Jin Baek, Jehan Alam: The presence of bacteria within tissue provides insights into the pathogenesis of oral lichen planus . In: Scientific Reports . tape 6 , no. 1 , July 2016, ISSN 2045-2322 , doi : 10.1038 / srep29186 , PMID 27383402 , PMC 4935860 (free full text).
- ↑ Junxian Ma, Jinshan Zhang, Yan Zhang, Tingting Lv, Jie Liu: The Magnitude of the Association between Human Papillomavirus and Oral Lichen Planus: A Meta-Analysis . In: PLOS ONE . tape 11 , no. 8 , 29 August 2016, ISSN 1932-6203 , doi : 10.1371 / journal.pone.0161339 , PMID 27571417 , PMC 5003373 (free full text).
- ↑ Na Alaizari, Sa Al-Maweri, Hm Al-Shamiri, B Tarakji, B Shugaa-Addin: Hepatitis C virus infections in oral lichen planus: a systematic review and meta-analysis . In: Australian Dental Journal . tape 61 , no. 3 , September 2016, p. 282-287 , doi : 10.1111 / adj.12382 .
- ↑ C. Scully, M. Beyli, MC Ferreiro, G. Ficarra, Y. Gill: Update on oral lichen planus: etiopathogenesis and management . In: Critical Reviews in Oral Biology and Medicine: An Official Publication of the American Association of Oral Biologists . tape 9 , no. 1 , 1998, ISSN 1045-4411 , p. 86-122 , doi : 10.1177 / 10454411980090010501 , PMID 9488249 .
- ^ LR Eversole: Immunopathogenesis of oral lichen planus and recurrent aphthous stomatitis . In: Seminars in Cutaneous Medicine and Surgery . tape 16 , no. 4 , December 1997, ISSN 1085-5629 , pp. 284-294 , doi : 10.1016 / s1085-5629 (97) 80018-1 , PMID 9421220 .
- ↑ Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. Volume 1 . Elsevier, no location 2020, ISBN 978-0-7020-7552-0 , p. 483 f .
- ^ Vishal S. Chandan, Joseph A. Murray, Susan C. Abraham: Esophageal lichen planus . In: Archives of Pathology & Laboratory Medicine . tape 132 , no. 6 , June 2008, ISSN 1543-2165 , p. 1026-1029 , doi : 10.1043 / 1543-2165 (2008) 132 [1026: ELP] 2.0.CO; 2 , PMID 18517264 .
- ↑ a b c D. Ioannides, E. Vakirlis et al .: EDF S1 Guidelines on the management of Lichen Planus. (PDF) In: European Dermatology Forum. Retrieved March 14, 2020 .
- ^ Yi-Shing Lisa Cheng, Alan Gould, Zoya Kurago, John Fantasia, Susan Muller: Diagnosis of oral lichen planus: a position paper of the American Academy of Oral and Maxillofacial Pathology . In: Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology . tape 122 , no. 3 , September 2016, ISSN 2212-4411 , p. 332-354 , doi : 10.1016 / j.oooo.2016.05.004 , PMID 27401683 .
- ^ LR Eversole: Immunopathogenesis of oral lichen planus and recurrent aphthous stomatitis . In: Seminars in Cutaneous Medicine and Surgery . tape 16 , no. 4 , December 1997, ISSN 1085-5629 , pp. 284-294 , doi : 10.1016 / s1085-5629 (97) 80018-1 , PMID 9421220 .
- ↑ Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. Without place, ISBN 978-0-7020-7552-0 , p. 434 .
- ↑ Eduardo Calonje, Thomas Brenn, Alexander Lazar, Steven D. Billings: McKee's pathology of the skin with clinical correlations . Fifth ed. Without place, ISBN 978-0-7020-7552-0 , p. 485 .
- ↑ Majdy Idrees, Omar Kujan, Kate Shearston, Camile S. Farah: Oral lichen planus has a very low malignant transformation rate: A systematic review and meta-analysis using strict diagnostic and inclusion criteria . In: Journal of Oral Pathology & Medicine: Official Publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology . January 25, 2020, ISSN 1600-0714 , doi : 10.1111 / jop.12996 , PMID 31981238 .
- ↑ Karthik Ravi, D. Chamil Codipilly, Dharma Sunjaya, Hongfei Fang, Amindra S. Arora: Esophageal Lichen Planus Is Associated With a Significant Increase in Risk of Squamous Cell Carcinoma . In: Clinical Gastroenterology and Hepatology: The Official Clinical Practice Journal of the American Gastroenterological Association . tape 17 , no. 9 , August 2019, ISSN 1542-7714 , p. 1902–1903.e1 , doi : 10.1016 / j.cgh.2018.10.018 , PMID 30342260 .
- ^ FM Lewis, CI Harrington: Squamous cell carcinoma arising in vulval lichen planus . In: The British Journal of Dermatology . tape 131 , no. 5 , November 1994, ISSN 0007-0963 , pp. 703-705 , doi : 10.1111 / j.1365-2133.1994.tb04987.x , PMID 7999604 .
- ↑ S. Fundarò, A. Spallanzani, E. Ricchi, A. Carriero, S. Perrone: squamous cell carcinoma developing within anal lichen planus: report of a case . In: Diseases of the Colon and Rectum . tape 41 , no. 1 , January 1998, ISSN 0012-3706 , pp. 111-114 , doi : 10.1007 / bf02236905 , PMID 9510320 .
- ^ S. Leal-Khouri, GJ Hruza: Squamous cell carcinoma developing within lichen planus of the penis. Treatment with Mohs micrographic surgery . In: The Journal of Dermatologic Surgery and Oncology . tape 20 , no. 4 , April 1994, ISSN 0148-0812 , pp. 272-276 , doi : 10.1111 / j.1524-4725.1994.tb01624.x , PMID 8163749 .