Vulvar cancer
| Classification according to ICD-10 | |
|---|---|
| C51.- | Malignant neoplasm of the vulva |
| ICD-10 online (WHO version 2019) | |
Vulvar cancer and vulvar cancer ( vulva : female external genital organs) are rare malignant tumor diseases of the outer part of the female. While the term vulvar cancer includes all malignant tumors of the vulva, vulvar cancer only refers to those malignant tumors of the vulva that are epithelial in origin. However, these make up by far the main part. Mostly the labia majora are affected , less often the labia minora and the area of the clitoris . Over 90% of tumors are squamous cell carcinomas . The remaining 10% are basal cell carcinomas , adenocarcinomas , melanomas , and carcinomas of the Bartholin's glands . But sarcomas , i.e. malignant tumors that originate from mesenchymal tissue, can also be found. The latter originate from the connective tissue of the vulva and are therefore not part of the vulvar carcinoma, but they do fall under the term vulvar cancer.
etiology
The causes and risk factors for developing vulvar cancer are largely unknown. Infections with human papilloma viruses 16 and 18 are known as risk factors ; they are the main cause of cell changes and cancers in the genitals. But they cannot cause vulvar cancer on their own. Chronic inflammatory diseases such as B. vulvitis , leukoplakia (white callus disease ) or lichen sclerosus of the vulva and vagina increase the risk of getting sick. Immunocompromised patients ( HIV , medication) and smokers are also at increased risk. Other diseases, which are accompanied by cornification, inflammation and dehydration in the area of the external genital organs, favor the development of vulvar cancer. Under certain circumstances, condylomas (genital warts) can also degenerate. Other risk factors can include other anogenital intraepithelial neoplasms or carcinomas, genital herpes , and syphilis . There are two forms of squamous cell carcinoma of the vulva: One HPV-positive carcinoma, which occurs mainly in younger women, and a second, which does not have HPV and mostly occurs in older women.

Incidence
Vulvar cancers make up about 5% of genital cancers in women. In Germany about 2 out of 100,000 women fall ill every year. Often the patients are older than 60 years. The incidence increases from 0.4 in 30-year-olds to 20 in women over 70 years of age. Vulvar intraepithelial neoplasias (VIN) are more commonly diagnosed today, especially in women aged 35 to 40. According to a prognosis by the cancer registry (GEKID - March 2011), 3,400 to 4,000 women fall ill in Germany every year.
Symptoms and diagnosis
Early symptoms of vulvar cancer and its precursors ( vulvar intraepithelial neoplasia (VIN)) are often atypical, inconclusive or completely absent. Persistent symptoms require a precise clinical diagnosis that goes into detail. The patient is first asked ( anamnesis ), then a physical examination takes place: a gynecological examination by palpation and a vulvoscopy . An ultrasound examination or other imaging methods such as X-rays or computed tomography can sometimes detect abnormalities. A tissue removal ( punch biopsy ) with a subsequent fine tissue examination ( histology ) is carried out especially if there are ambiguous findings to confirm the diagnosis. The result of this examination indicates which stage is present. The procedure for treatment depends on this.
In the early stages of the disease, white, less often brown, spots or warts appear. However, vulvar cancer usually only becomes noticeable at a more advanced stage (bloody discharge, recurrent itching or noticeable lumps and ulcers). Often the diagnosis is also a chance finding during the gynecological examination, because the inspection of the external genitalia is part of the cancer screening test (KFU). Chronic itching usually occurs with precancerous changes ( VIN ).
Common symptoms
- itching
- white skin coverings ( leukoplakia )
- dark, brownish spots
- Genital warts ( condylomas )
- Elevations (elevations), tumors
- red, non-healing, oozing spots / cracks
Proof / First Steps
- Test with vinegar solution (3–5%)
- Colposcopy / Vulvoscopy
- Biopsy of the injury ( lesion ) under local anesthesia for tissue clarification
- If necessary, referral to the dysplasia consultation
Staging
Stages according to TNM classification and FIGO (Fédération Internationale de Gynécologie et d'Obstétrique):
| TNM | FIGO | criteria |
|---|---|---|
| T | - | Primary tumor |
| TX | - | Primary tumor cannot be assessed |
| T0 | - | No evidence of primary tumor |
| Tis | 0 | Carcinoma in situ ( VIN 3) |
| T1 | I. | Tumor confined to the vulva or vulva and perineum , with no lymph node metastases |
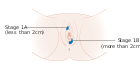
| T1a | IA | < 2 cm, stromal invasion < 1.0 mm |
| T1b | IB | > 2 cm or stromal invasion> 1.0 mm |
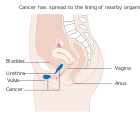
| T2 | II | Tumors of any size limited to the lower parts of the urethra , vagina and / or anus , without lymph node metastases |
| T3 | IVA | Tumor affects the upper part of the urethra and / or vagina, the bladder / rectal mucosa, or the tumor is attached to bone |
| N | - | Regional lymph nodes (inguinal lymph nodes) |
| NX | - | Regional lymph nodes cannot be assessed |
| N0 | - | No regional lymph node metastases |
| N1a | IIIA (ii) | one or two affected lymph nodes <5 mm in size |
| N1b | IIIA (i) | an affected lymph node ≥5 mm in size |
| N2a | IIIB (ii) | three or more affected lymph nodes <5 mm in size |
| N2b | IIIB (i) | two or more affected lymph nodes ≥5 mm in size |
| N2c | IIIC | Spread outside the lymph node capsule |
| N3 | IVA (ii) | caked, ulcerated lymph nodes |
| M. | - | Distant metastases |
| M0 | - | No distant metastases detectable. |
| M1 | IVB | The tumor has formed distant metastases (including pelvic lymph node metastases). |
therapy
There are different treatments for vulvar cancer, depending on the location, size, and stage. The preferred therapy is currently the surgical removal of the tumor with a healthy margin. In any case, this operation is necessary, the aim is to remove the tumor tissue as completely as possible. The extent to which the tissue is removed depends on the stage of the disease. Laser vaporization is only permitted for histologically proven dysplasias (VIN, AIN, CIN, VaIN). In the case of larger tumors, parts or, if necessary (in the case of very large tumors) the entire vulva, must be removed (vulvectomy). But there are different radical forms of therapy .
Vulvectomy forms
- Laser or skinning vulvectomy - superficially limited ablation. The affected skin of the vulva is removed while protecting deeper layers of tissue - suitable for dysplasia / VIN.
- Partial Vulvectomy - Partial vulvectomy involves removing only part of the vulva. An example of this is hemivulvectomy (half-vulvectomy), in which the part of the vulva where the tumor is located is removed.
- Simple vulvectomy - complete removal of the vulva, the lymph nodes are not removed.
- Radical vulvectomy - removal of the entire vulva and inguinal lymph nodes.
The so-called "en bloc resection" (Butterfly) in radical vulvectomy is completely out of date ( obsolete ) and full of complications. Another step in the reduction of radicality was the "three-cut technique" (triple excision), which reduced postoperative complications, but this surgical technique also meant the complete loss of the vulva . That is why vulvectomy is now in many cases replaced by “radical local excision” (wide excision) as a safe alternative. In advanced stages of vulvar cancer, in which the tumor has spread to neighboring tissue, a more radical surgical technique is necessary. The entire vulva with inguinal lymph nodes ( lymphadenectomy ) and (depending on the spread of the tumor) other organs such as B. Urinary bladder , rectum (rectum), uterus ( uterus ) and vagina ( vagina ). This extensive operation could also be necessary in the event of a relapse . In the case of well-demarcated tumors, the tumor is cut out in healthy tissue with a safety margin. The lymph nodes and pathways in the groin, which are the first stage in a possible tumor settlement, are removed with a deep infiltration of 1 mm (from stage T1b). The removal of the lymph nodes ( lymphadenectomy ) can be limited to a single sentinel lymph node removal under special quality and structural requirements, which significantly reduces the risk of lymphedema .
Plastic reconstructive types of operations
The goals of reconstructive operations in all women are
- Avoidance of side effects and complications
- Preservation of the female appearance
- Individual risk-adapted approach
- Tension-free defect coverage for large defects (wounds)
- Reconstruction of the vulva
- Avoidance of mutilating operations
- Preservation of sexual function through a sufficiently wide vaginal entrance
- Optimal aftercare (avoidance of pocket formation)
This is achieved with relatively simple methods of plastic-reconstructive surgery, such as B. Skin flaps. R0 resection (complete removal of the tumor) is a prerequisite for optimal therapy in patients with vulvar cancer. In addition to the necessary radicalism, functionality and aesthetics and thus an intact external appearance should also be the goal of the operation for every patient.
In exceptional cases, the operation can be supplemented with radiation therapy . A chemotherapy is only secondary tumors ( metastases used).
Radio- and radiochemotherapy of vulvar cancer
Irradiation ( radiation ) of the genital region should not be carried out "as a precaution". Unfortunately, the usual vulvar cancers are not very sensitive to radiation and the sensitive genital region tends to react very strongly. However, in certain cases it is necessary to carry out this therapy. If the tumor is in a very unfavorable location (e.g. on the sphincter muscle), this could reduce the size of the tumor before an operation and possibly preserve the sphincter muscle. The guidelines of the German Society for Gynecology and Obstetrics (DGGG) differentiate:
- Primary radiation therapy: Radiation therapy alone for vulvar carcinomas is limited to patients with far advanced tumors when a cure is no longer possible with surgical means ( palliative therapy ).
- Primary chemoradiotherapy: Primary (before surgery) chemoradiotherapy reduces tumor size and improves the operability of large primary tumors.
- Adjuvant radiation therapy: The adjuvant (after the operation, supplementary or supportive) radiation should also include the small pelvis in addition to the groin, since this is where the nearest lymph node station is located.
Surgical removal of lymph nodes in the small pelvis, either in addition or alone, only makes sense in individual cases (e.g. very large tumors). An American study (GOG 117) was able to show that the prognosis of patients in whom the pelvis was irradiated was better than in those patients in whom the pelvic lymph nodes were surgically removed. There may be indications for adjuvant, inguinal radiotherapy, i.e. in the area of the groin and not in the area of the external female genitals
- two or more affected lymph nodes
- Capsule overrun
- Metastasis> 10 mm
literature
- Heinrich Schmidt-Matthiesen , Gunther Bastert , Diethelm Wallwiener : Gynecological Oncology: Diagnostics, Therapy and Follow-up Care - on the basis of the AGO guidelines . Schattauer, 2002, ISBN 3-7945-2182-X ( full text in the Google book search).
- Jörg Baltzer , Hans-Gerd Meerpohl, Jens Bahnsen: Practice of gynecological oncology. Concepts for the differentiated approach in diagnostics, therapy and aftercare. Volume 3 of the practice of gynecology . Georg Thieme, 2000, ISBN 3-13-109912-7 ( full text in the Google book search).
- Carlos Thomas: Special Pathology . Schattauer, 1996, ISBN 3-7945-1713-X ( full text in the Google book search).
- EJ Crosbie, RJ Slade, AS Ahmed: The management of vulval cancer. In: Cancer Treat Rev . , 35, 2009, pp. 533-539, PMID 19699036
- JA de Hullu et al. a .: Management of vulvar cancers. In: Eur J Surg Oncol , 32, 2006, pp. 825-831. PMID 16690244 (Review)
- JA de Hullu et al. a .: Modern management of vulvar cancer. In: Curr Opin Obstet Gynecol 16, 2004, pp. 65-72. PMID 15128010 (Review)
Web links
- Information about vulvar cancer from the German Cancer Society e. V. (PDF; 110 kB)
- Vulvar cancer gynecologists online
- S2 guideline : Diagnosis and therapy of vulvar cancer and its precursors , AWMF register number 015/059 (online: full text ), as of June 2008
- Vulvar carcinoma self-help group e. V.
- Adviser to vulvar cancer
- Information on vulvar cancer (PDF) patient brochure
Individual evidence
- ↑ Munoz et al. In: New England Journal of Medicine , 2003, 348, p. 6
- ↑ Cogliano et al. In: The Lancet , 2005, Vol. 6
- ↑ A. Ansink: Vulvar squamous cell carcinoma . In: Semin Dermatol , 2, 1996, 15, pp. 51-59, PMID 8723825 .
- ↑ MM Madeleine, JR Daling, JJ Carter, GC Wipf, SM Schwartz, B McKnight, RJ Kurman, AM Beckmann, ME Hagensee, DA. Galloway: Cofactors with human papillomavirus in a population-based study of vulvar cancer . In: J Natl Cancer Inst , 1997, 89, pp. 1516-1523.
- ^ AB Maclean: Vulvar cancer and the need for awareness of precursor lesions. In: J Low Genit Tract Dis , 13, 2009, pp. 115-117. PMID 19387133 (Review)
- ↑ A. Katalinic, U.Gerdemann: Current figures for vulvar cancer in Germany . (PDF) March 2011.
- ↑ LH Sobin, MK Gospodarowicz, Ch. Wittekind: UICC: TNM classification of malignant tumors. 7th edition, Wiley-Blackwell, Oxford 2009, ISBN 978-1-4443-3241-4 Changes to the 6th edition ( page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice. (PDF; 1.9 MB)
- ↑ Ch. Wittekind, H.-J. Meyer: TNM classification of malignant tumors. 7th edition. Wiley-VCH, Weinheim 2010, ISBN 978-3-527-32759-1
- ↑ A Ansink, J. van der Velden: Surgical interventions for early squamous cell carcinoma of the vulva . Cochrane Database Syst Rev 1999, 4, CD002036, PMID 10796849 .
- ^ S2 guideline: Diagnosis and therapy of vulvar cancer and its precursors . ( Memento of the original from July 18, 2013 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice. (PDF; 1.6 MB) AWMF registration number 015/059, as of June 2008
- ↑ AG Van der Zee u. a .: Sentinel node dissection is safe in the treatment of early-stage vulvar cancer. In: J Clin Oncol , 26, 2008, pp. 884-889, PMID 18281661 .
- ↑ JA de Hullu, AG van der Zee: Surgery and radiotherapy in vulvar cancer. In: Crit Rev Oncol Hematol 60, 2006, pp. 38-58. PMID 16829120 (Review)