Herpes simplex
| Classification according to ICD-10 | |
|---|---|
| B00 | Herpes virus infections [herpes simplex] |
| ICD-10 online (WHO version 2019) | |
As herpes simplex ( Latin simplex , simple ') refers to various by herpes simplex virus -induced viral infections . Colloquially, the shortened form of herpes is usually used for a special localization on the skin . The word comes from the ancient Greek ἕρπειν herpein ('crawl'), which means the creeping spread of the skin lesions in a herpes simplex infection (also in the form of herpes febrilis with cold sores ).
Herpes simplex is a sexually transmitted disease .
Herpes simplex infections are caused by two different virus species: herpes simplex virus 1 (HSV-1) and herpes simplex virus 2 (HSV-2). They show slight deviations with regard to their clinical pictures and the localization of the disease. According to the appearance and localization of the symptoms of the disease, clinically different HSV infections are described, of which the herpes simplex labialis (cold sores) and the herpes simplex genitalis (genital herpes) are common. In addition to these forms, there are also rare, severe HSV infections such as generalized HSV sepsis in patients with immunodeficiency, herpes simplex encephalitis and generalized HSV infection of the newborn ( herpes neonatorum ).
After a (also symptom-free) initial infection, the virus remains in a resting state (latency) for life in the organism, which is known as persistent infection. This property of persistence is found in all members of the Herpesviridae family . The therapy of HSV infections is not able to end this persistence, but tries to prevent the virus from multiplying after reactivation from the dormant stage. There are several antivirals available for HSV therapy that are highly specific.
history
The genital manifestation of herpes simplex was already mentioned by Hippocrates around 400 BC. Described as a symptom of a spreading vesicle disease. The fact that the disease is also transmissible was known at the latest in Roman antiquity, since Emperor Tiberius forbade kissing at public ceremonies, as the spread of a vesicle disease on the lips was observed. This was documented by Aulus Cornelius Celsus as the first epidemic of a possible herpes disease. Herpes labialis was also widespread in Europe in the 16th and 17th centuries and its transmission through kissing was well known. William Shakespeare writes in his famous tragedy Romeo and Juliet : "O'er ladies' lips, who straight on kisses dream, Which often the angry Mab with blisters plagues, because their breaths with sweetmeats are tainted." (Translation: "The beautiful lips that dream of kisses, Often the angry Mab plagues them with blisters, Because their breath spoiled nibbling"; erg. Explanation: The name Mab occurring in the quote refers to the fairy "Queen Mab", who occurs in a speech by Mercutio in the work).
In 1736, Jean Astruc recognized genital herpes as a disease in its own right, and not as a variant of gonorrhea or syphilis, as previously assumed . In 1883, the German dermatologist Paul Gerson Unna described the frequency of the disease and how it occurred together with other sexually transmitted diseases. He also carried out the first histological studies on herpes simplex . After Wilhelm Gürtler was able to experimentally transfer the causative agent of herpes keratitis ( herpes corneae ) to a rabbit eye in 1913 , Ernst Löwenstein found the identity of the causative agent of both diseases by transferring the contents of the herpes labialis vesicles to a rabbit eye. The HSV was finally isolated and characterized for the first time by Slavin and Gavett in 1946 from the vesicle contents of a patient. The first electron microscopic representation of herpes simplex viruses was made by Coriell in 1950. It was not until the 1960s that Andre Nahmias, and especially Karl Eduard Schneweis, discovered that herpes simplex infections are caused by two different virus species, which the researchers have different Could distinguish antigenicity .
Pathogen
Herpes simplex viruses
The two causative agents of herpes simplex infections - the herpes simplex viruses 1 and 2 - which are taxonomically and more correctly also referred to as human herpes virus 1 and 2 (HHV-1/2), belong to the genus simplex virus of the family Herpesviridae . Members of this genus related to the herpes simplex viruses can also be found in animals, where these viruses cause similar diseases, for example in cattle or spider monkeys , macaques and other vervet monkeys . Although herpes viruses are generally strictly specialized in their respective hosts , the HSV-1 similar Cercopithecine Herpesvirus 1 ( Herpesvirus simiae ) of macaques can rarely be transmitted to humans, where it can cause severe, generalized infections.
The herpes simplex viruses are large viruses with a diameter of 140 to 180 nm. In an icosahedral capsid there is a linear, double-stranded DNA as a genome . The capsid is in turn surrounded by a virus envelope , which makes the viruses sensitive to soaps , detergents or already mild disinfectants . Between the capsid and the virus envelope there is a large number of virus proteins, the so-called tegument proteins, which are responsible, among other things, for the regulation of gene expression in the host cell and the transition of the virus into a dormant latency stage. As a double-stranded DNA virus, the herpes simplex viruses are genetically stable, mutations and the development of natural variants are rather rare.
Transmission and dissemination
Herpes simplex viruses are widespread all over the world; humans are the only natural host for them as a reservoir . Since HSV-1 is acquired through saliva contact and smear infection from infancy in normal family contact, it is common in the population. The virus shows an age-dependent seroprevalence that reaches high percentages around the end of puberty and then only increases slightly. In Germany, antibodies against HSV-1 could be detected in 84 to 92% of people in an age-normalized random sample examination .
HSV-2 is transmitted through close contact with the mucous membrane when the virus in the virus carrier is just reactivating and reproducing again in epithelial cells . Virus shedding can occur even without visible lesions. The prevalence of antibodies against HSV-2 is distributed differently. It is particularly influenced by age and sexual activity; the geographical distribution is also different. For healthy blood donors or health monitors, the incidence ranged from 3% to 23% in the United States . This number is significantly higher in patients who have consulted a doctor for another sexually transmitted disease (up to 55%) or who have engaged in commercial prostitution (up to 75%).
Infection Mechanisms
In the case of a primary infection, the HS viruses penetrate through the mucous membrane cells of the oropharynx (mainly HSV-1) and the genital tract (mainly HSV-2). Areas at the transition from the mucous membrane to normal skin are preferentially infected. Here the viruses multiply in the epithelial cells. Herpes simplex viruses spread within the epithelium by destroying the host cells and releasing new virions or by fusing neighboring cells, with the unenveloped virus capsids infecting the new cell. The destruction of the epithelial cells manifests itself clinically in an inflammatory reaction , often an ulcer or an inflamed skin vesicle forms due to tissue destruction . The vesicular fluid is an exudate in which herpes simplex viruses accumulate in high concentrations (> 100,000 PFU / µl).
Through direct cell-cell contact or through virions in the intercellular fluid, the HSV reaches the nerve endings of sensitive neurons , from which it is specifically taken up and transported along the microtubules and intermediate filaments of the axon to the cell body of the nerve. This retrograde axonal transport occurs through binding of the virus (as a naked virus capsid , possibly with residual portions of tegument proteins and envelope proteins) to kinesin-like proteins and dynein . The speed of migration in the direction of the cell body is around 0.7 µm per second.
Forms of disease
Herpes labialis
With this form, sore spots with blisters ("fever blisters") usually occur around the mouth. A herpes simplex infection usually manifests itself in the form of herpes labialis (cold sores, herpes simplex labialis ) as a reactivation of an already existing HSV infection; HSV-1 is significantly more common than HSV-2 with 80 to 90% of cases. About 40% of the adult population experience a reactivation visible as vesicles at least once in their life. About 10–20%, especially of the younger adults, report multiple or occasional relapses (relapses, herpes simplex recidivans ). A preferred point of recurrence is the transition area between skin and red lips or the corners of the mouth. The reasons for this are the high density of sensory nerve endings on the lip and the exposure of those epithelial layers that are particularly favorable for the virus to multiply. Causes of herpes relapse include acute emotional stress and exposure to sunlight .
Febrile infectious diseases can be accompanied by the reactivation of a herpes labialis . Since the vesicles are already visible in the prodromal stage or in the early acute stage of an additional infectious disease and these stages are usually accompanied by a high fever, the herpes labialis recurrence is then referred to as herpes febrilis ("cold sores"). An often observed reactivation of the herpes labialis shortly before or during menstruation is sometimes also called herpes menstrualis .
The herpes labialis can develop with mild or absent symptoms with an initial infection. If vesicles form, they are - in contrast to recurrences - spread further apart over a larger area of skin. A primary HSV infection as herpes labialis can be clinically more severe in children and be associated with a general feeling of illness, fever and headache. The vesicles can flow together to form larger ulcerations and also be superinfected with bacteria (often Staphylococcus aureus ) . Occasionally the oral mucosa and the gums are also involved in the infection, where painful blisters ( aphthae ) and ulcers form. This typical onset is also called herpetic gingivostomatitis , herpetic stomatitis or mouth rot called.
Other locations
A herpes simplex infection can also occur in skin areas where the primary infection is not to be expected due to the virus being carried over. This happens after the hands come into contact with the open blisters of a herpes labialis or herpes genitalis by rubbing the pathogen into injured or susceptible skin areas ( autoinoculation ). This is followed by the formation of blisters on the nose ( herpes nasalis ), the cheek ( herpes buccalis , herpes facialis ), the eyelid or other parts of the body ( herpes corporis ). A special form is the infection of otherwise less susceptible areas of the skin through the action of force, as happens in special sports. The form of a herpes gladiatorum was first observed in wrestlers . In young wrestlers, initial infections can break out to a greater extent, e.g. B. in training camps. Similar observations have been made with rugby players.
Due to the typical blisters, the appearance of herpes simplex infections on different areas of the skin can be clinically similar to herpes zoster (shingles), i.e. reactivation of the varicella zoster virus . This is especially the case when the HSV lesions of the skin happen accidentally in the skin dermatome common for herpes zoster . One then speaks of a "zosteriform herpes simplex". Conversely, an atypical localized shingles can be misinterpreted as an HSV infection, this is the so-called "herpetiform zoster".
Special forms and generalized diseases
Eczema herpeticatum
A chronic skin disease such as atopic eczema , psoriasis or Darier's disease can lead to an additional herpes simplex infection of larger areas of the skin. This so-called eczema herpeticatum (or also eczema herpeticum ) is possible in the context of a primary infection or a reactivation of the herpes simplex virus; a common pathogen is HSV-1. The clinical picture appears as dispersed vesicles, some of which are arranged in groups, which confluent and quickly burst. The Eczema Herpeticatum often accompanied by severe malaise and harbors as generalized herpes simplex infection, the risk of herpes simplex encephalitis or in immunodeficient patients herpes sepsis. An Eczema Herpeticatum in children can also cause a very serious sepsis and should be treated urgently with medication.
Herpes simplex retinitis
A special form of infection in nerve tissue is infection of the retina of the eye (retina), known as herpes simplex retinitis. It belongs to the endogenous intraocular infections, which means that the infection always occurs through reactivation of the virus and not through progressive infection via another, external HSV infection of the eye ( herpes corneae ). In HSV retinitis, exudates are found in the retina as well as local inflammation foci, which can quickly develop into retinal tissue destruction (retinal necrosis ) and thus lead to blindness . HSV retinitis is also seen immediately or years after herpes simplex encephalitis. In these cases, the virus enters the retina via the optic nerve , both of which are anatomically considered to be parts of the brain.
Herpes simplex encephalitis
The herpes simplex encephalitis is a very dangerous disease with involvement of the central nervous system and high mortality (untreated about 70%). Antiviral drug treatment is indicated even if it is suspected. Very often persistent neurological deficits also remain after the illness.
Bell's palsy
An infection with HSV-1 is discussed as a common cause of a special form of paralysis of the facial nerve ( nervus facialis ). This so-called Bell palsy , an idiopathic peripheral facial paralysis , has not yet been fully explained. A demyelination of the HSV-infected nerve sheaths may take place, which is not caused by the replication of the virus itself, but is based on a virally induced immune response. This would also explain the ineffectiveness of antivirals despite proven HSV-1 infection, since these only suppress the virus replication, but not the misdirected immune response.
Herpes simplex esophagitis
An HSV infection of the mucous membrane of the esophagus ( esophagitis ) can occur as part of a reactivation from the neurons of the oropharynx. Typically, with this form, there are no additional lip vesicles as a sign of reactivation, in 2/3 of the cases the lower part of the esophagus is affected. Sharp, small, flat ulcers of the mucous membrane are characteristic of the endoscopic examination. The triggers for HSV esophagitis are usually severe underlying diseases or immunosuppressive therapy with corticosteroids or cytostatics . This localization is favored by damage to the esophagus, for example in the case of radiation therapy , severe reflux esophagitis , the insertion of a gastric tube or after chemical damage (burns). If there are no identifiable causes, the patient's immune status should be checked. HSV esophagitis as part of an HIV infection is considered an AIDS-defining disease.
Very rarely, HSV esophagitis can also occur as a concomitant disease to a clinically severe primary HSV infection. This form is also possible in immunocompetent, not previously ill patients, more often in men than women. In these cases of initial infection, herpetic stomatitis is always present at the same time . HSV esophagitis in immunocompetent individuals is usually self-limiting; in addition to symptomatic treatment of the symptoms, antiviral therapy is usually not necessary.
Generalized herpes simplex
The herpes simplex viruses can also cause diseases that do not arise primarily through neuronal spread, but rather through the bloodstream as temporary or permanent viraemia . A differentiation from additional symptoms of an initial infection or reactivation is not always strictly possible. The most severe form of generalized infection is "herpes simplex sepsis", or - since the term sepsis is not strictly used for viruses - disseminated herpes simplex infection.
Herpes simplex infections in pregnancy
The generalized herpes simplex infection of the newborn , the herpes neonatorum , is a very serious disease that urgently needs treatment. The cause is usually a transmission of HSV-2 (less HSV-1) from the mother to the child during the birth process . In childbearing women with a primary infection with HSV-2 and a manifestation of genital herpes in the 3rd trimester (from the 34th week of pregnancy), the risk of neonatorial herpes is particularly high. However, delivering by caesarean section can prevent the child from becoming infected. The herpes neonatorum relates to the newborn skin (localized or distributed over a large area), the mouth and throat, internal organs and in the most serious form and the central nervous system as herpes simplex encephalitis.
HSV-2 and HIV
In type 2 herpes simplex infection, which can be transmitted through sexual intercourse, the mucous membranes of the genital organs are often affected. HSV-2 infections are usually harmless in humans. In people with an already weakened immune system, such as AIDS patients , the HSV-2 infection can spread to other parts of the body and become life-threatening.
Diagnosis
In the majority of simple HSV infections, the diagnosis is made on the basis of the clinical picture; cost-intensive pathogen detection or a less informative test for anti-HSV antibodies is then not desirable. In addition to neurological and internal diagnostic procedures, each of which is useful for a specific HSV disease ( imaging procedures , magnetic resonance tomography for encephalitis, reflection of the fundus in retinitis, endoscopy for esophagitis, etc.), the detection of the specific pathogen is only important in severe diseases. In the case of immunodeficiency, for example in the context of chemotherapy or immunosuppression after organ transplantation, HSV diagnostics are of great importance, as these patients in particular are at risk of dangerous, generalized infections.
Serology and pathogen detection
The serological detection of antibodies against HSV-1 and HSV-2 is of only limited clinical importance. Antibody detection is only useful for epidemiological investigations. The problem of HSV antibody detection is based on the one hand on the very high prevalence of antibodies in clinically healthy people, an unreliable distinction between HSV-1 and HSV-2 in most available test systems and a late or non-existent antibody production in severe HSV diseases. Even with a generalized, disseminated HSV infection, anti-HSV IgG and IgM antibodies cannot be detected or can only be detected very late.
The detection of anti-HSV IgM antibodies has no clinical significance, since a first infection cannot be ruled out if IgM antibodies are not detected; on the other hand, the detection does not necessarily prove a first infection. IgM antibodies against HSV can persist for months and years, reappear when reactivated, undetectable during an initial infection or due to a relatively frequent non-specificity of the commercial test procedures. Successive infection with the two HSV species also makes it difficult to interpret the findings. The inadequate specificity of the antibody screening tests requires confirmation by means of Western blot or an indirect immunofluorescence test .
An initial infection with HSV can only be detected serologically by seroconversion of the anti-HSV IgG if a preliminary sample taken sufficiently close in time is negative and a follow-up sample becomes clearly positive after one to two weeks. It must be ensured that the antibodies have not been passively acquired, i. H. the positivity is not based on the administration of anti-HSV-positive blood products ( hyperimmunoglobulin , platelet concentrate , etc.) or maternal antibodies in newborns and infants. Fluctuating amounts of HSV-IgG or changing positive anti-HSV titers have no clinical significance. In the case of immunodeficient persons, the informative value of the antibody determination is also limited, since in these patients antibodies cannot be formed sufficiently or only after a delay.
The direct detection of pathogens in affected tissue or tissue fluids (liquor, aqueous humor, vesicle contents, etc.) offers the highest informative value for HSV infections. This is usually carried out by detecting the viral DNA using the polymerase chain reaction (PCR) or, more rarely, by detecting virus-specific antigens in the immunofluorescence test. Virus isolation in cell cultures is also possible as a highly specific, direct detection method, but this takes several days due to a subsequent differentiation of the viruses produced. Viruses can be detected by electron-optical examination of infected material, but it is not possible to differentiate morphologically between different species of the Herpesviridae virus family .
Resistance testing
In severe HSV infections that do not respond significantly within a few days to correctly performed antiviral therapy with acyclovir , the development of resistance is suspected. Diagnostically it is possible to test the resistance of the isolated virus strains. For this purpose, the virus is propagated in cell cultures and the still effective aciclovir concentration ( minimum inhibitory concentration ) is determined. The effective inhibition of virus replication in the cell culture can be determined using a plaque reduction test or a determination of the TCID 50 in dilution series. Virus strains that can only be inhibited at acyclovir concentrations of over 3 µM are considered to be resistant.
treatment
Specific therapy
Nucleoside analogs
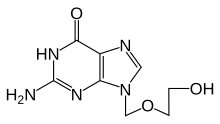
The first specifically effective active ingredient against HSV-1 and HSV-2 was acyclovir , which is still administered as an infusion for local use as well as for severe HSV infections and is considered to be the most effective specific antiviral agent for herpes simplex viruses. Only cells in which the virus actively replicates can phosphorylate acyclovir and convert it into its active form. The phosphorylated acyclovir is incorporated into the DNA strand by the viral thymidine kinase during the replication of the virus genome and thus leads to the interruption of the viral DNA synthesis. It is the first representative from the group of nucleoside analogues . As valaciclovir , which is only converted into aciclovir in the organism ( prodrug ), it has improved bioavailability in some applications such as oral therapy, but the antiviral mechanism of action is the same. Like valaciclovir, famciclovir is also an alternative to acyclovir (for example in the treatment of genital herpes).
Acyclovir-resistant mutations in the herpes simplex virus can rarely develop during therapy. In the most severe forms and proven resistance to acyclovir, Foscarnet is an alternative, but it causes significant side effects. A complete and permanent termination of the infection (i.e. the virus remaining in the body) has not yet been possible, because the action on infected areas of the skin fluorescence does not reach the viruses that persist in the nucleus of the nerve ganglia.
The nucleoside analogue penciclovir , which is structurally similar to aciclovir and which is also phosphorylated by the viral thymidine kinase and leads to chain termination during DNA synthesis, is only approved for external, local therapy .
Other specific antivirals
In addition to the specific nucloside analogs, tromantadine is occasionally used for topical application. Tromantadine is an adamantane derivative, the most common side effect of which can lead to allergic skin reactions or inflammation ( balanitis ).
An essential protein of the herpes viruses in viral DNA replication is the helicase-primase enzyme complex. Antiviral agents such as helicase-primase inhibitors show antiviral activity in animal experiments (e.g. BAY 57-1293). The first development candidates are currently being tested in clinical studies (phase I / II).
Symptomatic therapy
In the symptomatic therapy of dermal herpes simplex, attempts are made to reduce skin irritation, blistering or bacterial superinfection of the blisters and wound secretions. This is attempted through various drying or antibacterial agents added to ointments and creams. Alternatively, there are also hydrocolloid plasters ("herpes patches"). They do not contain any antiviral agents, but rather create a moist wound healing environment , which should allow the lesions to heal faster without crust formation. In addition, by covering the vesicles and absorbing the vesicle secretion, the patches are intended to prevent the herpes viruses from spreading.
In the case of frequent outbreaks, about several times a year, some people affected claim that puncturing the vesicles early accelerates the healing process and reduces the risk of infection due to the smaller volume of the leaking fluid. In fact, piercing increases the risk of contracting a bacterial infection of the area, a so-called superinfection . Since the fluid in the vesicles is only a symptom and not the cause of the disease, the puncture does not heal any faster, but the risk of infecting other people is increased by the permanent seepage of the fluid from the wound area. The fluid in the vesicles contains viruses in the highest concentration (> 1 billion per ml).
Home remedies and alternative treatment options
Various home remedies are believed to be useful in treating herpes. The effectiveness of home remedies has so far not been scientifically proven. These methods include dabbing with a freshly cut clove of garlic , toothpaste , honey, lemon balm , with hot, freshly boiled water , with alcohol or isopropanol, or rubbing in finely ground black pepper . Also, the effect and safety of coneflower , taiga root , L-lysine, zinc (as a compound), bee products and aloe vera during a herpes outbreak could not be proven with certainty. Research into the antiviral effectiveness of tea tree oil or the like has also not yet produced any indications of any effect on humans. In the case of tea tree oil, there are now indications of skin irritation after repeated use.
According to some publications, most of which date from the 1980s, the antioxidant butylated hydroxytoluene (BHT) can reduce the duration of blistering from an average of 2.4 to 2.0 days. However, the frequency and severity of the occurrence of herpes diseases were not reduced. In addition, symptoms of poisoning and pseudoallergies were observed with systemic use of BHT , so this treatment must be discouraged.
prevention
Ways to prevent a herpes simplex relapse are controversial. A variety of blank recommendations are circulating. This includes the general strengthening of the immune system through a healthy diet, exercise and adequate sleep.
Avoiding exposure to the sun (e.g. by applying sunblock to the lips) is associated with a lower recurrence rate according to the following studies.
Vaccine development
Various attempts to develop vaccines have been made, the first as early as the 1920s, but so far have not been successful. Due to the antigenic similarity of both virus species (HSV-1 and HSV-2), the development of a vaccine against one species also forms the basis for the vaccine development of the other.
The success of the chickenpox vaccine shows that an attenuated, active α-herpesvirus could in principle be used to prevent herpesviral infection in humans. The attenuation can thus be extended to HSV-1 and HSV-2, as shown in the case of an ICP0 protein-negative vaccine. In 2019, different vaccines are in different phases of clinical trials .
The following table lists vaccines against HSV. No HSV vaccine was commercially available until 2019. In addition, it is investigated to prevent virus latency and the subsequent reactivation of HSV using the CRISPR / Cas method .
| Vaccine | Company and Head of Research | Vaccine type | status | Results |
|---|---|---|---|---|
| Admedus
HSV-2 therapeutic vaccine |
Admedus | DNA vaccine | Phase II | 58% reduction in virus release, protection in 81% of those vaccinated after two vaccinations |
| dl5-29 / ACAM-529 / HSV-529 |
Sanofi Pasteur
David Knipe |
HSV-2 deficient in replication, with deletion of the genes UL5 and UL29 | Phase I. | HSV529-induced neutralizing and ADCC antibodies, but cellular immune response only in seronegative ones |
| VC2 |
Louisiana State University
Gus Kousoulas |
attenuated with small deletions in UL20 and UL53 | Preclinical | inhibits infection and virus latency in mice, guinea pigs and rhesus monkeys |
| R2 | Thyreos LLC
Gregory Smith, Gary Pickard, Ekaterina Heldwein |
attenuated with mutations in the R2 region of UL37 | Preclinical | inhibits infection in mice and rats after vaccination |
| HSV-2 ΔgD-2 | Albert Einstein College of Medicine William Jacobs Jr & Betsy Harold | attenuated HSV-2 with deletion of US6 (gD) | Preclinical | inhibits HSV-1 and HSV-2 in mice |
| HSV-2 trivalent vaccine |
Perelman School of Medicine at the University of Pennsylvania
Harvey Friedman & Sita Awasthi |
HSV-2 trivalent subunit vaccine with gC2, gD2, gE2 | Preclinical | inhibits virus release by 98.8% in mice |
| G103 | Immune design | HSV-2 trivalent subunit vaccine with gD, pUL19, pUL25 | Preclinical | Protection from lethal intravaginal HSV-2 infection in mice |
| GV2207 | GenVec | ? | Preclinical | ? |
| NE-HSV2 | NanoBio | ? | Preclinical | ? |
| TBA | Profectus BioSciences | DNA vaccine | Antigen detection phase | Not available |
| HSV-2 ICP0‾ HSV-2 0ΔNLS |
Rational Vaccines RVx
William Halford |
attenuated | Controversy over the consent of the vaccinated | Protection against disease in 65% of those vaccinated |
| Vitaherpavac & Herpovax | Russia | ? | ? | ? |
- Aborted vaccine developments
| Vaccine | organization | Vaccine type | reason | Results | |
|---|---|---|---|---|---|
| Herpevac, Simplirix | GlaxoSmithKline | Subunit vaccine gD2t with adjuvant AS04 | Failed phase III | no statistically significant results, no effect on HSV-2, partial protection against HSV-1 confirmed | |
| Unnamed | PaxVax | Vector vaccine | Termination in the preclinical phase | - | |
| ImmunoVEX HSV2 vaccine | Amgen , BioVex | attenuated | Termination in phase I. | - | |
| Gen-003 | Genocea | Subunit vaccine gD2 / ICP4 with matrix M2 | Termination after II | 58% reduction in virus release, 69% protection | |
| AuRx Herpes Vaccine | AuRx | Vector vaccine | Inactive | - | |
| DISC vaccine | Cantab Pharmaceuticals | attenuated with deletion of gH | Termination in phase I. | no use | |
| Unnamed | Mymetics | ? | Termination in the preclinical phase | - | |
| HerpV | Agenus | Peptide vaccine with adjuvant QS-21 | Termination after phase II | - | |
| VCL-HB01 | Vical | DNA vaccine from gD2 + UL46 with adjuvant Vaxfectin | Termination after phase II | no use | |
Reporting requirement
In Germany and Switzerland there is no legal obligation to report herpes simplex infections. In Austria only suspicion, illness and death from HSV-associated meningoencephalitis are notifiable.
literature
- David C. Hutfield: History of genital herpes . In: British Journal of Venereal Diseases Volume 42, No. 4, 1966, pp. 263-268. PMID 5333786 . PMC 1047831 (free full text).
- R. Marre, T. Mertens, M. Trautmann, E. Vanek (Eds.): Clinical Infectious Diseases . Munich / Jena 2000, ISBN 3-437-21740-2 , pp. 578ff, 596ff, 189f.
- H. Hahn, D. Falke, SHE Kaufmann, U. Ullmann (eds.): Medical microbiology and infectious diseases . 5th edition. Heidelberg 2005, ISBN 3-540-21971-4 , p. 610 ff.
- C. Mims, HM Dockrell, et al. (Ed.): Medical microbiology / infectiology . Elsevier, Munich 2006, ISBN 3-437-41272-8 .
- Stephan Dreyer: Herpes No thanks - handouts for people with cold sores . Böhl-Iggelheim Verlag Dr. Scriptor OHG, 2010, ISBN 978-3-9809578-7-8 .
Web links
- Herpes infections - information from the Robert Koch Institute
- Herpes in pregnancy, in babies and in children. In: Herpesfree.de. Retrieved on July 22, 2019 : "Table: The risk of transmission in pregnancy"
- Susanne Nessler: friend or foe? Herpes Viruses and the Immune System. In: br.de. Bayerischer Rundfunk, March 27, 2015, accessed on December 23, 2018 (podcast for the program IQ - Science and Research ).
- Herpes simplex. In: DermIS.net. Retrieved on December 23, 2018 : "28 images for this diagnosis"
- Dirk Manski: Genital herpes: viral infection with herpes simplex. In: Urologielehrbuch.de. March 22, 2009, accessed on December 23, 2018 (information and images).
- Katharina Kremser: Cold sores: causes, therapy, prevention. In: Apotheken-Umschau.de. Retrieved on November 28, 2019 : "Cold sores (Herpes labialis) - symptom of an infection with the herpes simplex virus type I - popularly known as fever blisters"
Individual evidence
- ^ Corpus Hippocraticum : De mulierum affectibus 1.90.
- ↑ RH Kampmeier: Herpes genitalis: a clinical puzzle for two centuries. In: sex. Trans. Dis. , Volume 11, 1984, p. 41.
- ↑ Mercutio to Romeo in Act 1, Scene 4 ( text on Wikisource )
- ^ Jean Astruc: De morbis venereis . Paris 1736 and A Treatise of Venereal Diseases . London 1754, Volume 1, Book 3, p. 365.
- ↑ PG Unna. In: J. cutan. vener. Dis. , 1883, 1, p. 321, accessible in: JK Oates: Venereal disease genital herpes . In: J. Hosp. Med. Volume 6, 1983, pp. 13-19.
- ↑ HB Slavin, E. Gavett: Primary herpetic vulvovaginitis . In: Proc. Soc. Exp. Biol. Med. Volume 63, 1946, p. 343.
- ↑ LL Coriell, G. et al .: rake Electron microscopy of herpes simplex . In: J. Bacteriol. Vol. 59, No. 1, 1950, pp. 61-68. PMID 15400321 .
- ↑ Karl Eduard Schneweis: Investigations on antigenic analysis and differentiation of types in the herpes virus hominis . Goettingen 1962.
- ↑ KE Schneweis, AJ Nahmias: Antigens of Herpes simplex virus type 1 and 2-immunodiffusion and inhibition passive hemagglutination studies . In: Z. Immunitätsforsch. Exp. Klin. Immunol. Volume 141, No. 5, 1971, pp. 471-487. PMID 4326538 .
- ↑ JF Szilágyi, J. Berriman: Herpes simplex virus L particles contain spherical membrane-enclosed inclusion vesicles . In: J. Gen. Virol. Volume 75, No. 7, 1994, pp. 1749-1753. PMID 8021604 .
- ↑ W. Hellenbrand, W. Thierfelder et al .: Seroprevalence of herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) in former East and West Germany, 1997-1998 . In: Eur. J. Clin. Microbiol. Infect. Dis. Volume 24, No. 2, 2005, pp. 131-135. PMID 15692814 .
- ↑ An overview of various epidemiological studies in B. Halioua, JE Malkin: Epidemiology of genital herpes - recent advances . In: Eur J Dermatology Volume 9, No. 3, 1999, pp. 177-184. PMID 10210781 . ( Table 2. In: . Jle.com Retrieved on December 23, 2018 (English). ).
- ^ CA Daniels, SG LeGoff: Shedding of infectious virus / antibody complexes from vesicular lesions of patients with recurrent herpes labialis . In: The Lancet Volume 20; 2, No. 7934, 1975, pp. 524-528. PMID 51344 .
- ↑ WW Liu, J. Goodhouse, NL Jeon, LW Enquist: A microfluidic chamber for analysis of neuron-to-cell spread and axonal transport of an alpha-herpesvirus . In: PLoS ONE Volume 18; 3, No. 6, 2008, p. E2382. PMID 18560518 PMC 2426917 (free full text).
- ↑ D. Malvy et al .: Epidemiology of orofacial herpes simplex virus infections in the general population in France: results of the HERPIMAX study . In: J. Eur. Acad. Dermatol. Venereol. Volume 21, No. 10, 2007, pp. 1398-1403. PMID 17958848 .
- ↑ Ronald Glaser, Janice Kiecolt-Glaser: Psychological influences on immunity: Implications for AIDS. In: American Psychologist . Volume 43, No. 11, Nov 1988, pp. 892-898. doi: 10.1037 / 0003-066X.43.11.892 .
- ↑ HE Schmidt u. a .: Stress as a pecipitating factor in subjects with recurrent herpes labialis. In: Journal of Family Practice. Vol. 20, No. 4, April 1985, pp. 359-366, PMID 3981095 .
- ↑ M. Ichihashi, H. Nagai, K. Matsunaga: Sunlight is an important causative factor of recurrent herpes simplex. In: Cutis. Volume 74, 2004, Supplement 5, pp. 14-18, PMID 15603217 .
- ↑ Vittorio Mazzarello, Marco Ferrari, Stefano Decandia and Maria Alessandra Sotgiu (December 19th 2018). Sunlight and Herpes Virus, Human Herpesvirus Infection - Biological Features, Transmission, Symptoms, Diagnosis and Treatment, Ronaldo Luis Thomasini, IntechOpen, DOI: 10.5772 / intechopen.82643
- ↑ B. Selling, S. Kibrick: An outbreak of Herpes simplex among wrestlers (Herpes gladiatorum). In: New Engl J Med Volume 7, No. 270, 1964, pp. 979-982. PMID 14122793 .
- ^ BJ Anderson: The epidemiology and clinical analysis of several outbreaks of herpes gladiatorum . In: Med. Sci. Sports Exerc. Volume 35, No. 11, 2003, pp. 1809-1814. PMID 14600542 .
- ^ WB White, JM Grant-Kels: Transmission of herpes simplex virus type 1 infection in rugby players . In: JAMA Vol. 27; 252, No. 4, 1984, pp. 533-535. PMID 6737650 .
- ↑ IR Sanderson et al .: Eczema herpeticum: a potentially fatal disease. In: Br. Med. J. Volume 294, No. 6573, 1987, pp. 693-694. PMID 3105692 , PMC 1245744 (free full text).
- ↑ M. Cordero-Coma et al .: Herpetic retinitis . (Review) In: Herpes Volume 14, No. 1, 2007, pp. 4-10. PMID 17848212 .
- ↑ J. Maertzdorf et al .: Herpes simplex virus type 1 (HSV-1) -induced retinitis following herpes simplex encephalitis: indications for brain-to-eye transmission of HSV-1 . In: Ann. Neurol. Volume 49, No. 1, 2001, pp. 104-106. PMID 11198277 .
- ^ A. Klein, P. Lefebvre: Three consecutive episodes of acute retinal necrosis due to herpes simplex-1 over twelve years following herpetic encephalitis . (Review) In: Ocul. Immunol. Inflamm. Volume 15, No. 5, 2007, pp. 411-413. PMID 17972228 .
- ^ S. Murakami et al .: Bell's palsy and herpes simplex virus: Identification of viral DNA in endoneurial fluid and muscle . In: Ann Intern Med Volume 124, No. 1, 1996, pp. 27-30. PMID 7503474 .
- ↑ H. Wakisaka et al .: Demyelination associated with HSV-1-induced facial paralysis . In: Exp. Neurol. Volume 178, No. 1, 2002, pp. 68-79. PMID 12460609 .
- ↑ An overview of HSV esophagitis in: K. Becker, HJ Lübke, F. Borchard, D. Häussinger: Inflammatory esophageal diseases caused by herpes simplex virus infections - overview and report of 15 own cases . In: Z. Gastroenterol. Volume 34, No. 5, 1996, pp. 286-295. PMID 8686361 .
- ↑ J. Ramanathan et al .: Herpes simplex virus esophagitis in the immunocompetent host: an overview . In: Am. J. Gastroenterol. Volume 95, No. 9, 2000, pp. 2171-2176. PMID 11007213 .
- ↑ Overview of the diagnostic problems in: Th. Mertens, O. Haller, H.-D. Klenk (Hrsg.): Diagnosis and therapy of viral diseases - guidelines of the society for virology . 2nd edition Munich 2004 ISBN 3-437-21971-5 pp. 126-130.
- ↑ G. Biancofiore et al .: Liver transplantation due to Herpes Simplex virus-related sepsis causing massive hepatic necrosis after thoracoscopic thymectomy. In: Minerva Anestesiol. Volume 73, No. 5, 2007, pp. 319-322. PMID 17529922 .
- ↑ NJ Schmidt, B. Forghani, EH Lennette: Type specificity of complement-requiring and immunoglobulin M neutralizing antibody in initial herpes simplex virus infections of humans. In: Infect Immun. Vol. 12, No. 4, 1975, pp. 728-732. PMID 1193713 , PMC 415348 (free full text).
- ^ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 306.
- ↑ KE Ostheimer et al .: Randomized double-blind trial of tromantadine versus aciclovir in recurrent herpes orofacialis . In: Arzneimittel-Forschung , 1989, 39 (9), pp. 1152-1155 PMID 2686658
- ↑ MR Holdiness: Contact dermatitis from topical antiviral drugs . Contact Dermatitis (2001) 44 (5), pp. 265-269 PMID 11298689
- ↑ I. Maatouk: Contact balanitis to tromantadine . In: Clin. Exp. Dermacol. , 2016, 41 (8), p. 926, PMID 27757977
- ↑ Kleymann et al .: New helicase-primase inhibitors as drug candidates for the treatment of herpes simplex disease . In: Nat. Med. . 8, No. 4, 2002, pp. 392-398. doi : 10.1038 / nm0402-392 . PMID 11927946 .
- ^ Sabine Werner: Creams, sticking or heat. In: deutsche-apotheker-zeitung.de. July 28, 2015, accessed on December 23, 2018 (No. 16, p. 62).
- ^ DJ Freeman et al .: Treatment of recurrent herpes simplex labialis with topical butylated hydroxytoluene . In: Clin Pharmacol Ther . Volume 38, No. 1, 1985, pp. 56-59. PMID 2988845 .
- ^ MW Grogan: Toxicity from BHT ingestion . In: West J Med. Volume 145, No. 2, 1986, pp. 245-246. PMC 1306899 (free full text).
- ^ V. Mazzarello, M. Ferrari, G. Piu, V. Pomponi, G. Solinas: Do sunscreen prevent recurrent Herpes labialis in summer? In: J Dermatolog Treat. Volume 30, No. 2, 2019, pp. 179-182. doi: 10.1080 / 09546634.2018.1481921
- ↑ L. Duteil, C. Queille-Roussel, C. Loesche, M. Verschoore: Assessment of the effect of a sunblock stick in the prevention of solar-simulating ultraviolet light-induced herpes labialis. In: Journal of Dermatological Treatment. Volume 9, No. 1, 1998, pp. 11-14, DOI: 10.3109 / 09546639809160682
- ↑ AA Chentoufi, E. Kritzer, DM Yu, AB Nesburn, L. Benmohamed: Towards a rational design of an asymptomatic clinical herpes vaccine: the old, the new, and the unknown . In: Clin. Dev. Immunol. . 2012, 2012, p. 187585. doi : 10.1155 / 2012/187585 . PMID 22548113 . PMC 3324142 (free full text).
- ^ WP Halford, R. Püschel, E. Gershburg, A. Wilber, S. Gershburg, B. Rakowski: A live-attenuated HSV-2 ICP0 virus elicits 10 to 100 times greater protection against genital herpes than a glycoprotein D subunit vaccine . In: PLoS ONE . 6, No. 3, 2011, p. E17748. doi : 10.1371 / journal.pone.0017748 . PMID 21412438 . PMC 3055896 (free full text).
- ^ NR Truong, JB Smith, KJ Sandgren, AL Cunningham: Mechanisms of Immune Control of Mucosal HSV Infection: A Guide to Rational Vaccine Design. In: Frontiers in immunology. Volume 10, 2019, p. 373, doi : 10.3389 / fimmu.2019.00373 , PMID 30894859 , PMC 6414784 (free full text).
- ↑ R. Whitley, J. Baines: Clinical management of herpes simplex virus infections: past, present, and future. In: F1000Research. Volume 7, 2018, S., doi : 10.12688 / f1000research.16157.1 , PMID 30443341 , PMC 6213787 (free full text).
- ^ X. Xu, Y. Zhang, Q. Li: Characteristics of herpes simplex virus infection and pathogenesis suggest a strategy for vaccine development. In: Reviews in Medical Virology. Volume 29, number 4, July 2019, p. E2054, doi : 10.1002 / rmv.2054 , PMID 31197909 , PMC 6771534 (free full text).
- ↑ J. Rajčáni, F. Bánáti, K. Szenthe, p Szathmary: The potential of currently unavailable herpesvirus vaccines. In: Expert review of vaccines. Volume 17, number 3, 03 2018, pp. 239–248, doi : 10.1080 / 14760584.2018.1425620 , PMID 29313728 .
- ↑ HS De Silva Feelixge, D. Stone, P. Roychoudhury, M. Aubert, KR Jerome: CRISPR / Cas9 and Genome Editing for Viral Disease-Is Resistance Futile? In: ACS infectious diseases. Volume 4, number 6, 06 2018, pp. 871-880, doi : 10.1021 / acsinfecdis.7b00273 , PMID 29522311 , PMC 5993632 (free full text).
- ↑ Admedus AU Immunotherapies . Retrieved January 18, 2017.
- ↑ Admedus US Research & Development - Admedus US . Retrieved August 2, 2016.
- ↑ ADMEDUS ANNOUNCES POSITIVE UNBLINDED HSV-2 PHASE II INTERIM DATA . 19th October 2016.
- ↑ Knipe Lab | Harvard Medical School .
- ^ Lee YC: Ventricular fusion beats . In: JAMA . 202, No. 10, December 2017, pp. S415 – S416. doi : 10.1093 / ofid / ofx163.1041 . PMC 5630753 (free full text).
- ↑ Stanfield BA, Stahl J, Chouljenko VN, Subramanian R, Charles AS, Saied AA, Walker JD, Kousoulas KG: A single intramuscular vaccination of mice with the HSV-1 VC2 virus with mutations in the glycoprotein K and the membrane protein UL20 confers full protection against lethal intravaginal challenge with virulent HSV-1 and HSV-2 strains . In: PLOS ONE . 9, No. 10, 2014, p. E109890. bibcode : 2014PLoSO ... 9j9890S . doi : 10.1371 / journal.pone.0109890 . PMID 25350288 . PMC 4211657 (free full text).
- ↑ Stanfield BA, Pahar B, Chouljenko VN, Veazey R, Kousoulas KG: Vaccination of rhesus macaques with the live-attenuated HSV-1 vaccine VC2 stimulates the proliferation of mucosal T cells and germinal center responses resulting in sustained production of highly neutralizing antibodies . In: Vaccine . 35, No. 4, January 2017, pp. 536-543. doi : 10.1016 / j.vaccine.2016.12.018 . PMID 28017425 .
- ↑ Stanfield BA, Rider PJ, Caskey J, Del Piero F, Kousoulas KG: Intramuscular vaccination of guinea pigs with the live-attenuated human herpes simplex vaccine VC2 stimulates a transcriptional profile of vaginal Th17 and regulatory Tr1 responses . In: Vaccine . 36, No. 20, May 2018, pp. 2842–2849. doi : 10.1016 / j.vaccine.2018.03.075 . PMID 29655629 .
- ↑ Herpes Virus Mutant Points Towards New Vaccine Strategy ( en-US ) Retrieved August 13, 2018.
- ↑ Richards AL, Sollars PJ, Pitts JD, Stults AM, Heldwein EE, Pickard GE, Smith GA: The pUL37 tegument protein guides alpha-herpesvirus retrograde axonal transport to promote neuroinvasion . In: PLoS Pathogens . 13, No. 12, December 2017, p. E1006741. doi : 10.1371 / journal.ppat.1006741 . PMID 29216315 . PMC 5749899 (free full text).
- ↑ Petro CD, Weinrick B, Khajoueinejad N, Burn C, Sellers R, Jacobs WR, Herold BC: HSV-2 ΔgD elicits FcγR-effector antibodies that protect against clinical isolates . In: JCI Insight . 1, No. 12, August 2016. doi : 10.1172 / jci.insight.88529 . PMID 27536733 . PMC 4985247 (free full text).
- ↑ New Genital Herpes Vaccine Candidate Provides Powerful Protection in Preclinical Tests . Penn Medicine News. January 19, 2017. Retrieved January 28, 2017.
- ^ Penn Institute for Immunology - The Friedman laboratory . September 3, 2018. Accessed October 1, 2018.
- ↑ Awasthi S, Hook LM, Shaw CE, Pahar B, Stagray JA, Liu D, Veazey RS, Friedman HM: An HSV-2 Trivalent Vaccine Is Immunogenic in Rhesus Macaques and Highly Efficacious in Guinea Pigs . In: PLoS Pathogens . 13, No. 1, January 2017, p. E1006141. doi : 10.1371 / journal.ppat.1006141 . PMID 28103319 . PMC 5245903 (free full text).
- ↑ Immune Design Pipeline . Immune design. Retrieved April 22, 2017.
- ↑ Odegard JM, Flynn PA, Campbell DJ, Robbins SH, Dong L, Wang K, Ter Meulen J, Cohen JI, Koelle DM: A novel HSV-2 subunit vaccine induces GLA-dependent CD4 and CD8 T cell responses and protective immunity in mice and guinea pigs . In: Vaccine . 34, No. 1, January 2016, pp. 101–9. doi : 10.1016 / j.vaccine.2015.10.137 . PMID 26571309 . PMC 6322202 (free full text).
- ↑ a b GV2207 - HSV-2 Immunotherapeutic: GenVec, Inc. (GNVC) . Retrieved August 16, 2016.
- ↑ nanobio - HSV-2 vaccine . Retrieved August 2, 2016.
- ↑ NanoBio Corporation: NanoBio's Genital Herpes Vaccine Demonstrates Efficacy In Guinea Pigs As Both A Prophylactic And A Therapeutic Vaccine . Retrieved August 2, 2016.
- ↑ PBS Vax ™ Therapeutic Vaccines . In: profectusbiosciences.com . Retrieved August 15, 2016.
- ↑ Introducing RVx ( en-US ) March 12, 2016. Accessed August 2, 2016.
- ^ Herpes Vaccine Research ( en-US ) Retrieved August 2, 2016.
- ↑ FDA Launches Criminal Investigation Into Unauthorized Herpes Vaccine Research . Retrieved May 21, 2018.
- ^ Rational Vaccines: A case study in pharma deregulation - MedCity News . March 2017. Retrieved September 26, 2017.
- ^ Status of Vaccine Research and Development of Vaccines for Herpes Simplex Virus . Retrieved August 30, 2016.
- ↑ Sandgren KJ, Bertram K, Cunningham AL: Understanding natural herpes simplex virus immunity to inform next-generation vaccine design . In: Clinical & Translational Immunology . 5, No. 7, July 2016, p. E94. doi : 10.1038 / cti.2016.44 . PMID 27525067 . PMC 4973325 (free full text).
- ↑ QUESTIONS AND ANSWERS The Herpevac Trial for Women . Retrieved August 30, 2016.
- ↑ Cohen J: Immunology. Painful failure of promising genital herpes vaccine . In: Science . 330, No. 6002, October 2010, p. 304. bibcode : 2010Sci ... 330..304C . doi : 10.1126 / science.330.6002.304 . PMID 20947733 .
- ↑ Better Neutralization of Herpes Simplex Virus Type 1 (HSV-1) Than HSV-2 by Antibody From Recipients of GlaxoSmithKline HSV-2 Glycoprotein D2 Subunit Vaccine . In: The Journal of Infectious Diseases . August 15, 2014. Retrieved July 10, 2019.
- ↑ PaxVax Signs R & D Collaboration with UC San Diego to Develop a Vaccine to Prevent Herpes Simplex Virus Infections . In: paxvax.com . June 10, 2014. Retrieved August 15, 2016.
- ↑ About . Retrieved January 4, 2017.
- ↑ The PaxVax Platform - Product Pipeline . Retrieved September 5, 2016.
- ↑ Awasthi S, Zumbrun EE, Si H, Wang F, Shaw CE, Cai M, Lubinski JM, Barrett SM, Balliet JW, Flynn JA, Casimiro DR, Bryan JT, Friedman HM: Live attenuated herpes simplex virus 2 glycoprotein E deletion mutant as a vaccine candidate defective in neuronal spread . In: Journal of Virology . 86, No. 8, April 2012, pp. 4586-98. doi : 10.1128 / JVI.07203-11 . PMID 22318147 . PMC 3318599 (free full text).
- ↑ Amgen Pipeline . Retrieved August 2, 2016.
- ↑ Genocea Announces Strategic Shift to Immuno-oncology and the Development of Neoantigen Cancer Vaccines . 25th September 2017.
- ↑ AuRx, Inc . AuRx. Retrieved January 4, 2017.
- ↑ AuRx, Inc . AuRx. Retrieved January 4, 2017.
- ↑ McAllister SC, Schleiss MR: Prospects and perspectives for development of a vaccine against herpes simplex virus infections . In: Expert Review of Vaccines . 13, No. 11, November 2014, pp. 1349-60. doi : 10.1586 / 14760584.2014.932694 . PMID 25077372 . PMC 4385587 (free full text).
- ↑ Mymetics HSV Vaccine Candidate . Mymetics. Retrieved April 22, 2016.
- ↑ Biological Efficacy Study of HerpV Vaccine With QS-21 to Treat Subjects With Recurrent Genital Herpes . Retrieved August 31, 2016.
- ↑ Vical HSV-2 Therapeutic Vaccine VCL-HB01 . Retrieved January 18, 2016.
- ↑ Vical Reports Phase 2 Trial of HSV-2 Therapeutic Vaccine Did Not Meet Primary Endpoint . Retrieved June 16, 2018.