clitoris

The inset is seen foreskin (1) and glans of the clitoris (2) and including the two front ends of the labia minora (small Vulval lips).
The largest part of the clitoris, namely the clitoral legs and their erectile tissue, are not visible from the outside.
The clitoris or clitoris ( Latin clitoris , genitive: clitoridis ; from ancient Greek κλειτορίς kleitorís , 'little hill') is a part of the female genitals made of cavernous tissue . It consists of two legs ( crus clitoridis ) that unite towards the front of the body. Only a small part of the clitoris is visible on the outside. This glans of the clitoris ( glans clitoridis ), which is enclosed by the clitoral hood ( praeputium clitoridis ), is the most sensitive part of this organ. The entire clitoris plays for sexual arousal and orgasm the woman an important role.
The clitoris forms, together with the opening of the urethra ( urethral ), the atrium of the vagina ( vaginal ), and the major and minor lips ( labia majora et minora ) (small Vulvalippen) the vulva ( vulva ).
Anatomy and function
embryology
Historically , the clitoris and penis emerge from the genital hump .
The development of the external genitalia begins in a sexually indifferent phase, so that the tissue differentiation of the two sexes is not complete until the twelfth week. In both sexes, in the indifferent phase, there are initially:
- Genital tuberosity, genital tuberosity ; ventral to the cloacal membrane ( urogenital sinus )
- Genital or urethral folds; on both sides of the cloacal membrane
- Genital ridges or labioscrotal ridges; lateral to the genital folds
The differentiation to the female genital is characterized by the regression of the ductus mesonephricus ("Wolffian duct") and the retention of the ductus paramesonephricus ("Müllerian duct"), from which the tuba uterina , the uterus and part of the ( distal ) vagina arise. The urogenital sinus, together with the genital ridges and the genital hump, forms the external genitalia (lowest ( proximal ) part of the vagina, vestibulum vaginae , labia majora et minora ) and the clitoris. The genital hump initially grows in length in both sexes and thus becomes the clitoris or penis. The clitoris is formed from the genital hump. The urogenital sinus remains as vaginal vestibule open and the two genital folds form the labia minora (small Vulvalippen), labia minora . The genital bulges enlarge and form the large labia (large vulval lips), labia majora . The urogenital membrane lies between the genital folds and closes the later urogenital ostium . This tears about a week after the urorectal septum has grown together with the cloacal membrane, exposing the ostium.
anatomy
The clitoris consists of two erectile tissue, crura clitoridis (singular: crus clitoridis ) , attached to the ischial bone section, arcus ischiadicus , which unite under the arcus pubis to form the shaft, corpus clitoridis .

1: clitoral hood , praeputium clitoridis
2: clitoris glans , glans clitoridis , which merges into the clitoris shaft, corpus clitoridis , before it branches into the two cavernous bodies , corpora cavernosa clitoridis

1) glans, glans , together with the clitoral shaft, Corpus clitoridis in the foreskin , prepuce of the clitoris surrounded lying from the musculus ischiocavernosus
2) cavernosum, corpus cavernosum clitoridis which paired initial part united to form the corpus clitoridis
3) clitoris thighs, crus clitoridis
4) urethral orifice , ostium urethrae externum
5) atrial erectile tissue, bulbus vestibuli surrounded by the musculus bulbospongiosus
6) vaginal opening , vestibulum vaginae
The free end is widened to form the glans clitoridis , which is covered by the clitoral hood ( praeputium clitoridis ) . The clitoris is attached to the lower edge of the symphysis by a ligament, the ligamentum suspensorium clitoridis . The corpus cavernosum in the shaft area, corpus cavernosum clitoridis , is a paired organ of spongy, cavernous nature, which unites in the direction of the symphysis to the corpus clitoridis up to the clitoral glans. The two parallel cavernous bodies of the shaft are surrounded by a fibrous collagenous sheath, the tunica albuginea ; this sheath joins the clitoral hood in the direction of the glans clitoridis .
The two expiring labia minora (small vulval lips) form the paired frenula clitoridis and form a medial soft tissue fold on the underside of the clitoris. It runs from the cranial junction of the two labia minora (small vulval lips) to the glans clitoridis .
The glans clitoridis is more like the glans penis , i.e. not strictly homologous . When looking closely, it is important to know that the glans clitoridis is the anterior end of the corpus clitoridis , which corresponds to the corpora cavernosa penis , while the glans penis , corpus spongiosum (penis) , is located at the upper end of the urethral erectile tissue , corpus cavernosum urethrae , is located.
The glans and crura both contain cavernous tissue and are surrounded by a solid tunica albuginea. The male corpus spongiosum corresponds to the atrial cavernous bodies, bulbi vestibuli , which are divided into two parts on each side of the urethral and vaginal exit. These erectile tissue systems have very different dimensions in women.
The arterial supply takes place via branches of the internal pudendal artery : the deep clitoral artery extends to the thighs of the clitoris and the dorsal clitoral artery to the glans of the clitoris. The dorsal clitoral vein drains blood from the entire clitoris into the venous plexus around the urinary bladder .
The lymph drains through the lymph nodes in the groin . While the lymph of the vulva enters the Nodi lymphatici Nll. inguinales superficiales drain, the lymph of the anterior clitoral parts with the corpus and glans clitoridis ind Nll. inguinales profundi and Nll. internal iliac drains.
Cavernous system of the clitoris

|

|
|
|
Left: Projection of the clitoral glans , glans clitoridis , the clitoris shaft or root, corpus clitoridis , and the two cavernous bodies or clitoral limbs , crura clitoridis , onto the body surface.
Right: Schematic 3-D representation of the cavernous body systems; in the foreground the glans and corpus clitoridis with the two attached, slimmer crura clitoridis behind them the two thicker bulbi vestibuli |
||
The cavernous clitoris ( corpora cavernosa ) are erectile tissue, which consists of smooth muscle cells and connective tissue . The two legs of the clitoris ( crura clitoridis ) each contain an erectile tissue (the corpus cavernosum clitoridis dextrum (right side) or sinistrum (left)). These cavernous bodies fill with blood during clitoral erection. Furthermore, under the mucous membrane of the vaginal vestibule ( vestibulum vaginae ) are the atrial cavernous bodies ( bulbi vestibuli ). This dense plexus of veins is connected to the cavernous tissue of the clitoris. The clitoris is suspended from the lower edge of the symphysis by the ligamentum suspensorium clitoridis .
The two paired corpora cavernosa clitoridis unite on their way to the symphysis to the corpus clitoridis and finally to the glans clitoridis . The tunica albuginea surrounds the two corpus cavernosum limbs to maintain and stabilize their shape; it is a layer of connective tissue made of fiber-rich connective tissue, which runs over the corpora cavernosum clitoridis to the glans clitoridis in the preputium clitoridis .
The parasympathetic nervous system as the efferent part of the vegetative reflex arc leads to vasocongestion of the erectile tissue through sensitive afferents such as the mechanoreceptors in the erogenous genital zones of the clitoris or in the anterior vaginal area. The sympathetic nervous system as efference increases the tone of the smooth muscles or causes them to contract .
Cavernous body system of the vaginal vestibule
The bulbi vestibuli lie on the vestibulum vaginae as dense venous plexuses in a horseshoe shape and are connected to the cavernous tissue of the clitoris. While the clitoris is entirely derived from the corpora cavernosa , unlike the male penis , the female corpora spongiosum forms the atrial erectile tissue , the bulbus vestibularis and the erectile tissue around the urethra, the urethra . When man evolved from the corpus spongiosum of Harnröhrenschwellkörper, for a corpus spongiosum and the glans of the man who Eichelschwellkörper, but corpus spongiosum glandis of a continuation of the Corpus spongiosum is.
The female erectile tissue, which develops from the corpus spongiosum , continues, some anatomical-histological investigations suggest, between the anterior wall of the vagina and the bladder as an intermediate layer, it is the so-called half-angled fascia . It is divided into two parts, the proximal septum vesicovaginale , a connective tissue space that extends between the trigonum vesica of the urinary bladder dorsally and the anterior, ventral part of the vagina. After ventral or distally , coming from the bladder and the vagina, it will come as a septum uretrovaginale between the female urethra and vagina or in the vestibule, vaginal vestibule , continued.
Historically, the erectile tissue systems in the hemi-fascia are homologous to the urethral erectile tissue, corpus spongiosum penis , which envelops the urethra in the male penis . The cavernous body systems in the half-angled fascia are supposed to make up two of the female intravaginal erogenous zones , but these are not so much exactly localizable points, but rather zones of the embryonic derivatives of the corpus spongiosum :
- G-spot or Graefenberg zone in the front third of the vagina
- A point in the area of the anterior cervical vault, fornix cervicalis anterior (English anterior fornix zone, abbreviated to AFE zone )
Cavernous body systems and topographical relationship to the pelvic floor muscles

The musculofascial connective tissue system of the female pelvic floor has passages for the rectum , urinary and sexual organs and is topographically closely related to the above-mentioned cavernous body systems. From the inside out, the pelvic floor is divided into:
- Pelvis diaphragm : posterior part of the pelvic floor, coccygeus muscle and the levator ani muscle on both sides(with its three parts puborectalis muscle , pubococcygeus muscle and iliococcygeus muscle ), broken through by the rectum
- Urogenital diaphragm : anterior part of the pelvic floor, formed by the transversus perinei profundus and superficialis muscles(and their fasciae), passage of the urethra, in women also the vagina
- Cavernous and sphincter layer : muscle ischiocavernosus , muscle bulbospongiosus ; External ani sphincter muscle
The strongest and most extensive of these three muscle and fascia layers is the pelvic diaphragm , it is the innermost, funnel-shaped layer of the pelvic floor. The pelvic diaphragm has a longitudinal gap running from dorsal to ventral, the levator slit, for the mouths or entrances to the urinary and genital organs. The urogenital diaphragm extends from the pubic symphysis, the symphysis and the two pubic branches to the ischial tuberosities and partially covers the levator slit incompletely from below. The urogenital diaphragm also has an opening for the urethra and the vagina. The fibers around the point of passage for the urethra form the outer urethral sphincter , urethralis muscle, some muscle fibers from this also radiate into the vaginal wall. The outer sphincter layer, i.e. the outer pelvic floor muscles, consists of several individual muscles and their associated fasciae. Mention should be made of the paired erectile tissue muscle, the bulbospongiosus muscle, and the ring-shaped external anal sphincter muscle , the external sphincter ani muscle . In women, these two form an eight-shaped muscle loop around the vagina and anal canal.
The muscles of the M. sphincter ani , M. bulbospongiosus, and M. transversus perinei superficialis form the lowest, most caudal layer of the pelvic floor. In contrast, the external ani sphincter and fibers of the bulbospongiosus muscle are a form of a recumbent figure eight around the rectum and the vaginal introitus ; they are connected to the erectile tissue of the vaginal vestibule , the vestibulum vaginae . Thus, the swelling tissue surrounding the urethra in the anterior third of the vagina, the paraurethral venous plexus, is also embedded in the Skene gland , the paraurethral gland , and the erectile tissue of the small labia, the bulbi vestibuli , under the bulbospongiosus muscle and the urogenital diaphragm . The actual erectile tissue of the clitoris, the corpus clitoridis and the crura clitoridis lying on both sides lie under the ischiocavernosus muscle .
Clitoral hypertrophy
| Classification according to ICD-10 | |
|---|---|
| Q52.6 | Malformations of the clitoris |
| ICD-10 online (WHO version 2019) | |

|

|
|
|
Vulva with enlarged glans clitoridis ( clitoral hypertrophy ) in two different women (age: 19 and 22 years)
|
||
Under the influence of male sex hormones (androgens), the penis forms in male fetuses . Excessive androgen production also leads to increased growth of the genital cusps in female fetuses, so that the clitoris itself protrudes like a penis (a clitoral hypertrophy ). Also associated with Fraser syndrome , the clitoris can be abnormally enlarged. However, this disorder is extremely rare.
Clitoral enlargement can also occur later in life. The main cause of this is hormonal disorders such as polycystic ovarian syndrome .
An exact diagnosis by a doctor based on objective criteria is often not made. Instead, the subjective impression of a clitoris that is perceived as too big is often more decisive. If a significantly enlarged clitoris represents a physical and / or primarily aesthetic problem for the person concerned, a surgical reduction can be performed today, comparable to labioplasty , if the level of suffering is demonstrably independently felt and expressed . However, there is usually no medical need for this procedure.
Surgical correction may also be appropriate in cases of intersex under the same conditions. Intersex activists therefore demand that such an operation should only be carried out if the intersex person wants the operation of his own volition and can consent to it.
Clitoris and intercourse
During sexual intercourse and the associated sexual excitement, congestion occurs in the vaginal vestibule , as the bulbi vestibuli around the vaginal vestibule constrict and the small labia (small vulval lips), labia minora, approach the inserted penis. The muscles bulbospongiosi also have a synergistic effect on this constriction .
Furthermore, the bulbi vestibuli are connected to the (cavernous) tissue of the clitoris, through which there are many cavities. Your venous outflow is hindered by the pressure in the arterial system and an increase in pressure in the erectile tissue is the result. Nevertheless, even with congestive blood filling of the corpus cavernosum clitoridis, the kink between the two crura clitoridis and the corpus clitoridis is retained. Biomechanically it is believed in the penetration through the penis that the train to the small, inner lips (inner Vulvalippen) to the withdrawing of them to the clitoris frenula clitoridis transfers. This is intended to bring the glans of the clitoris, glans clitoridis, closer to the penetrating penis and to increase the joint sexual arousal during copulation through frictional movement .
Innervation
The entire clitoris is heavily endowed with nerve endings. The whole system is particularly sensitive to touch and receptive to sexual stimuli. Most women orgasm by stimulating the clitoris . The glans of the clitoris, where the nerve cords of the two legs meet, is particularly sensitive. Winkelmann (1959) found in his histological investigations that the clitoris is, next to the fingertips, the most densely innervated part of the human body surface. This also applies to other mammals , as shown in the animal model that the dorsal clitoral nerve contains twice as many nerve fibers as the dorsal penis nerve .
The clitoris has up to 8000 nerves and sensory cells, such as the mechanoreceptors of the Vater-Pacini corpuscles (also corpusculum lamellosum or genital nerve corpuscles) for the sensation of vibration and the Meissner corpuscles for the sensation of touch. The clitoral hood protects the sensitive glans of the clitoris.
But not only is the number of innervating nerves on the glans clitoridis higher than in the male penis, the vibratory perception threshold of the clitoris is also lower than that on the glans penis . This makes the clitoris one of the most sensitive areas of the body to external, tactile stimuli. The sensory thresholds increase somewhat with increasing age of the woman.

Sensitive information history
The sensitive, mostly tactile nerve information (surface sensitivity) of the clitoris is transmitted from an extensive network around the tunica albuginea of the clitoris body, corpus clitoridis , with a nerve-free zone in the "12 o'clock position". Most of the sensory information from the clitoris is carried by the bilateral dorsal clitoral nerve , the dorsal clitoral nerve . The dorsal clitoral nerve is a terminal branch of the pudendal nerve from the sacral plexus (S 1 –S 4 ); it takes care of the female clitoris in a sensitive manner. The nerves come as part of the pudendal nerve in Alcock's canal on a protected path through the urogenital diaphragm on the lower clitoris.
The pudendal nerve in general - in particular the dorsal clitoral nerve - has an important function in the area of clitoral-vulvar afferents as well as for the sphincteric and circumvaginal-muscular efferents.
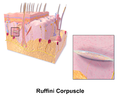
Ruffini bodies , especially in the area of the labia minora and the clitoral hood (hood), Praeputium clitoridis ; Stretch receptor, d. H. respond to pressure and horizontal stretching.
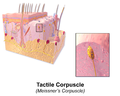
Meissner corpuscles ; d. H. react to pressure changes, rapidly adapting (RA) mechanoreceptors, only activated by changing the stimulus strength, tactile receptor
Vater-Pacini corpuscles were identified in the ligamentum suspensorium clitoridis and in the corpus clitoridis , but not in the glans clitoridis itself; react to accelerations, quickly adapting receptors, vibration receptors
Four forms of free nerve endings shown schematically
There are three types of exteroceptive nerve endings, so-called sensory cells, in the clitoral region . They are not only located in the actual clitoris, but also in the labia minora (small vulval lips), labia minora and in the periurethral connective tissue of the urethral orifice, meatus urethrae . The top layer of skin contains so-called free nerve endings . Above all, they transmit pain perceptions. The impulses picked up by them are transmitted through very thin nerve fibers via peripheral somatic nerves and via the sacral spinal cord at the low speed of 1–2 m / sec. transfer.
The so-called genital nerve corpuscles or mucocutaneous nerve endings (according to Winkelmann 1959), mostly Meissner corpuscles and Vater-Pacini corpuscles or the smaller variant of the Krause corpuscles, are located under the skin layer. These Meissen corpuscles are located near the skin surface, in the area of the skin papillae , they detect touch and vibration on a narrowly defined area with high precision; They react immediately, but block out the flow of information if the stimulus persists for a longer period of time. Vater-Pacini corpuscles, on the other hand, are located deep in the connective tissue of the papillary bodies and detect touch and vibration over a larger area without making them precisely localizable; they adapt quickly, i.e. H. they only respond at the beginning and at the end of the stimulus.
The glans of the clitoris, glans clitoridis , showed in various histological examinations a thick layer of cutaneous corpuscular receptors. On the other hand, the Father Pacini corpuscles are completely absent there. This immunohistochemical and histological study by Cheryl Shih (2013) showed masses of corpuscular receptors with a variable arrangement in the subepithelial layer in the tissue samples of the clitoral organ. A second type of receptor, the Vater-Pacini corpuscles, was found in the ligamentum suspensorium clitoridis, but not in the glans itself.
physiology
The sympathetic and parasympathetic nervous systems act synergistically; H. Both systems are active and complement each other for the optimal regulation of the innervated target organs. While the sympathetic nervous system tends to prevent a clitoral erection, the parasympathetic part of the autonomic nervous system forms one of several important excitatory circuits that lead to vasocongestion of the clitoral (and other) cavernous bodies. Whether the sexual arousal is triggered by direct physical stimulation of the sexual organs or psychological ideas from other sensory organs ( pheromones , tactile stimuli, visual impressions, etc.) or by thinking about a person - the exciting nerve fibers in the clitoris react in such a way that they do so release called pro-erectile neural neurotransmitters . They include nitric oxide (NO), acetylcholine and the like. a. m.
It is assumed that the increasing blood flow to the vulva and vagina in the course of sexual arousal is primarily mediated by the gasotransmitter nitric oxide , "NO" or (in combination) with the vasoactive intestinal peptide (VIP) . The importance of “NO” for vasocongestion of the vulvar, bulbar and clitoral erectile tissue is confirmed, among other things, by the discovery of NO synthase in human erectile tissue.
Adrenergic and cholinergic nerve pathways lead to the vaginal wall and the clitoris, which they innervate. According to immunohistochemical examinations, the latter is additionally determined by numerous non-cholinergic, non-adrenergic neurotransmitters (“NANC”) (“non-adrenergic noncholinergic neurotransmitters”) such as B. the vasoactive intestinal polypeptide (VIP) , peptide histidine methionineamide (PHM) neuropeptide Y (NPY) , calcitonin gene-related peptide (CGRP) , substance P and nitric oxide (NO).
In the erection of the clitoris, in addition to corresponding sensory perceptions, i.e. activation of corresponding nerve areas ( afferents to areas in the cerebrum, hypothalamus and sacral spinal cord ( parasympathetic )) through sensory stimuli, the activation of the endothelial cells in the blood vessels of the clitoris also plays a role important role. When the endothelial nitric oxide synthase is activated , the messenger substance nitric oxide (“NO”) is released in the corresponding vascular section. This nitrogen monoxide (NO) then activates the guanylyl cyclase and leads to the increased formation of cyclic guanosine monophosphate (“cGMP”). The smooth muscles of the arterioles relax . As the blood vessels expand in the arterioles, the clitoral cavernous bodies fill with blood (vasocongestion).
Oil glands, smegma and pheromones
The clitoris is equipped with various glands, especially in the area of the frenulae clitoridis on the lower part of the clitoral glans. These are the sebum glands and apocrine sweat glands (see also vomeronasal organ (VNO) and vertebrate pheromones ) that form the smegma clitoridis .
Around the clitoris (periclitoral) at the level of the vestibulum vaginae there are numerous orifices of the glandulae vestibulares minores , which give off a slimy, alkaline secretion and resemble the glandulae vestibulares majores in their structure . The smegma clitoridis is a mixture of sebum glands, more precisely from the Tyson glands (ectopic sebum glands, i.e. sebum glands that do not open into hair follicles or a hair follicle ), a form of free sebum glands that are located in the folds of skin between the outer and inner labia (inner vulval lips) as well around the Praeputium clitoridis. It is precisely because of these skin folds, which lie close together, that the release of heat, evaporation of fluid and the removal of the flaked epithelium are hindered; in this way a warm, moist, predominantly anaerobic environment with a neutral to slightly alkaline pH value can arise.
It is composed of cell debris from the dead and flaked surface epithelium , fatty acids , steroid derivatives (e.g. cholesterol esters ), proteins and bacteria. As everywhere in and on the human organism, there is a specific and typical microbial site flora , e.g. As the yeasts of Malassezia and the mycobacteria scoring Mycobacterium smegmatis , also called "Smegmabakterium".
The role of the clitoris in sexual arousal
In women, the complex sexual response in the pelvic organs ultimately manifests itself as vasocongestion , which then leads to lubrication in the vagina in preparation for the introduction, penetration of the penis. This lubrication is based on the secretion of an exudate which, together with general genital congestion, leads to the plateau phase which precedes the actual orgasm . Vaginal vasocongestion and the consequent lubrication as well as clitoral erection depend on increased blood flow in the female pelvic organs. Play here u. a. the α1-adrenoceptor subtypes , as they can be found in almost all cavernous tissues of vertebrates, also play a major role.
"Clitoral" and "vaginal" orgasm
In the past, a distinction was made in women between the "vaginal" orgasm , which is achieved exclusively through vaginal stimulation, i.e. by penetrating the vagina with the penis, with an inserted finger or with a vibrator (or other objects), and the "clitoral" Orgasm that can only be achieved by stimulating the glans of the clitoris, the glans clitoridis . Many studies, such as that of Kinsey , indicate that a considerable proportion of women can only reach orgasm if the clitoris is (co-) stimulated. ( See also the current state of research )
The importance of the distance between the clitoris and the urethral meatus ( clitoral-urinary meatus distance, CUMD)
The psychoanalyst Marie Bonaparte , also known under the pseudonym AE Narjani, examined the distance between the clitoris and the urethral meatus , also known as the clitoral-urinary meatus distance (CUMD), in a study from 1924 in a total of 43 women , and then questioned the test subjects about their sexual experiences. The point of reference for their measurements was the junction of the paired frenula clitoridis with the meatus urethrae externus located in the introitus vaginae . It was shown for the examiner in her evaluations that there was a correlation between the CUMD and the ability to orgasm.
In other words, the closer the clitoris was to the urethral orifice, the more often the affected women experienced orgasm. It is hypothesized that women with a clitoris closer to the urethral orifice have more orgasms than women with a greater distance. According to studies by K. Warren and EA Lloyd (2011), these results are interpreted more functionally. Accordingly, it would be important in vaginal intercourse that there should be a cohabitational approach between the introitus vaginae and the clitoris.
sensitivity
The sensitivity of the clitoral glans to direct stimulation varies greatly from person to person . Some women are so sensitive that they only endure direct stimulation after prolonged foreplay and then only very gentle stroking, or even not at all, or only when using lubricant . With other women, on the other hand, the sexual encounter only becomes complete enjoyment through the intense rubbing touch of the clitoris . What is “good” at the moment can also differ from situation to situation and change several times during a sexual encounter. Since the clitoris is closely connected to the surrounding tissue , as described above, various forms of indirect stimulation are common practice.
In very rare cases, too little sensitivity of the clitoris can be attributed to a too large clitoral hood. In contrast, a comparable phenomenon can be traced back far more often to ignorance of the anatomy or the existence of shame boundaries that prevent self-determined sexuality.
During penetration , the pull is transferred to the labia minora (small vulval lips) and via these to the clitoris ligaments ( frenulae clitoridis ) and the clitoris. This brings the glans of the clitoris closer to the penetrating penis. Through rubbing movements, special sensory cells, the mechanoreceptors , increase sexual arousal.
Comparative functional anatomy of mammals
Mammals exhibit two main forms of ovulation , so coitus-induced ovulation probably evolved first. From this, as an adaptation to new factors, later the derived property of cyclical or spontaneous ovulation emerged. In mammals that show coitus-induced ovulation , neuroendocrine systems also play a role in addition to the effect of neuronal olfactory ( vertebrate pheromones ) and emotional stimuli. They are involved in spontaneous and reflex-induced ovulation, including the hypothalamic - pituitary - gonadokinetic system and the neurohormonal pathways for coitomimetic stimuli. The translation of vaginal-clitoral stimulation into gonadomimetic humoral messages that lead from the hypothalamus or the posterior pituitary to the release of luteinizing hormone (LH) and prolactin is complex and has not yet been adequately described. The female orgasm plays a direct reproductive role in coitus-induced ovulation. As a supportive reflex, it helps to induce ovulation. Comparative anatomical studies of the female genitals showed that with the development of spontaneous ovulation, the clitoris also changed its anatomical position. Because in mammals that need an orgasm for their reproduction, the sexual organ is located near or even far in the female sexual channel.
Significance in the history of science
The first scientific description of the clitoris by the anatomist Realdo Colombo from Padua in 1559 is a frequently studied example in the history of medicine and sex research. In his anatomical work de re anatomica , Colombo claimed to have discovered the clitoris as the “place of female pleasure”. You will, “when you touch it, notice that it becomes a bit harder and elongated, so much so that it turns out to be a kind of male member”. Colombo's description later turned into a priority dispute , as Gabriele Falloppio - Colombo's successor in Padua - claimed to be the real discoverer of the clitoris.
The “discovery” of the clitoris in the Renaissance is an interesting phenomenon in many ways from a scientific historical perspective. Of course, women had already discovered the clitoris before Colombo, and of course men before Colombo were made aware of the clitoris and its sexual function. The fact that the clitoris did not appear in the anatomical description of humans before Colombo is an illustration of the fact that the anatomical description of humans was usually an anatomical description of the male body.
At the end of the 18th century, male anatomists devoted themselves primarily orally to the physiological function of the clitoris. Sometimes it was assumed that only Denis Diderot had openly and in writing presented the pleasure-giving function of the clitoris in Die indiskreten Kleinode 1748 or in the article Jouissance of the Encyclopedia 1765. The role of the clitoris in female desire was described as early as 1724 in popular writings by, among others, the doctor and social reformer Bernard de Mandeville .
However, the historian of science Thomas Laqueur points out that the clitoris contradicted the common ancient anatomical theory about sexual organs. Under the influence of Galenos , the vagina and penis were not perceived as two fundamentally different organs. Rather, it was assumed that the vagina is an inwardly turned penis and that the structure of the female and male genital organs is analogous. The clitoris, which Colombo also described as a kind of penis, did not fit into this theory.
In 1844 Georg Ludwig Kobelt published a very detailed anatomical description of the clitoris, including its underlying structure, such as the “Kobelt's venous plexus” and its function.
In 1887 the clitoris appears in " Gray's Anatomy ", a standard anatomy work. Here the clitoris is still shown in its original size. As early as 1901 it was only shown as a small bulge. In 1913 it disappears completely from "Gray's Anatomy".
In 1998, the Australian urologist Helen O'Connell published the results of her research on the widespread structure of the clitoris
In 2004, the TV broadcaster Arte published a highly acclaimed report on the research of Kobelt and his successors with the title Clitoris, the beautiful unknown .
Clitoridectomy
A clitoridectomy is the partial or complete surgical removal of the clitoris. For cultural reasons, carried out this engagement is outside the practicing communities today often under the term "female genital mutilation" (English. Female genital mutilation summarized FGM). There is also a medical indication for clitoral cancer .
See also
- Clitoria ternatea , a plant whose flower resembles a clitoris
- Clitoral adhesion
- Clitoral piercing
- Clitoral plastic
- Vaginal self-exam
literature
- Milou D. Bekker, Cornelis RC Hogewoning, Chris Wallner, Henk W. Elzevier, Marco C. De Ruiter: The somatic and autonomic innervation of the clitoris; preliminary evidence of sexual dysfunction after minimally invasive slings. University Medical Center, Leiden, pp. 23-41, full text. (PDF).
- Vincent Di Marino, Hubert Lepidi: Anatomic study of the clitoris and the bulbo-clitoral organ. Springer, Heidelberg 2014, ISBN 978-3-319-04893-2 ( restricted view on Google books).
- Vincenzo Puppo: Anatomy of the Clitoris: Revision and Clarifications about the Anatomical Terms for the Clitoris Proposed (without Scientific Bases) by Helen O'Connell, Emmanuele Jannini, and Odile Buisson. In: ISRN Obstetrics and Gynecology. Volume 2011, 2011, pp. 1–5, doi: 10.5402 / 2011/261464 .
- Kim Wallen, Elisabeth A. Lloyd: Clitoral variability compared with penile variability supports nonadaptation of female orgasm. In: Evolution & Development , 2008, Volume 10, No. 1, pp. 1-2, full text. (PDF).
- Vincent Di Marino, Hubert Lepidi: Anatomic Study of the Clitoris and the Bulbo-Clitoral Organ. Berlin / Heidelberg / New York 2014, ISBN 978-3-319-04894-9 .
- K. Wallen, EA Lloyd: Female sexual arousal: genital anatomy and orgasm in intercourse. In: Hormones and behavior. Volume 59, number 5, May 2011, pp. 780-792, doi: 10.1016 / j.yhbeh.2010.12.004 , PMID 21195073 , PMC 3894744 (free full text).
- Rebecca Chalker: The Clitoral Truth. Seven Stories Press, New York 2000, archive.org
- Roy J. Levin: The Clitoris — An Appraisal of its Reproductive Function During the Fertile Years: Why Was It, and Still Is, Overlooked in Accounts of Female Sexual Arousal. In: Clinical Anatomy. Wiley Periodicals, November 5, 2019, doi: /10.1002/ca.23498 ( full text as PDF file ).
Movies
- Clitoris - The beautiful stranger. Complete Media (September 2007), ISBN 978-3-8312-9488-6 , © ARTE France 2002. A film by Stefan Firmin and Michele Dominici on behalf of ARTE.
- Clitoris - The beautiful stranger. Arte documentation on youtube: Part 1 , Part 2 , Part 3 , Part 4 , Part 5 , Part 6 , Part 7 , accessed on December 28, 2011
Web links
- Anatomy of the clitoris . On: the-clitoris.com ; Retrieved July 9, 2015.
- View of the dam, “perineum” with vascular supply . Illustration of an anatomical preparation on: ect.downstate.edu ; Retrieved July 9, 2015.
- Anatomy of the clitoris. Illustration of an anatomical preparation on: ect.downstate.edu ; Retrieved July 9, 2015.
- Barbara Maier, Luci Wohlfart: Clitoris, the unknown beauty. Unknown - unnamed female anatomy and female pleasure life. Salzburg State Hospital, full text. (PDF; 3.3 MB)
- Elia Bragagnada: The Physiology of Female Sexual Arousal. Full text. (PDF; 8.8 MB).
- Sharon Mascall: Time for rethink on the clitoris . on Helen O'Connell's discovery At: news.bbc.co.uk , last update June 11, 2006; Retrieved July 9, 2015.
- Anne Fawcett: Anatomy of a revolution - Helen O'Connell has changed the way students learn about the female body. smh.com.au, September 8, 2005 (English). Retrieved July 9, 2015.
- Petra Stute: The female orgasm. Physiology and pathophysiology, hormonal influences, and female orgasm disorder . (PDF) University Hospital Bern, accessed on July 31, 2018.
- Daniel Haag-Wackernagel : The female excitation system from the perspective of evolutionary biology. (PDF) Department of Biomedicine, University of Basel, 2017.
Individual evidence
- ↑ https://www.duden.de/rechtschreibung/Klitoris
- ↑ Comparison of the analogous anatomical structures between the clitoris and penis. On: emory.edu ; accessed on September 20, 2016.
- ^ Alfred Sigel, RH Ringert: Pediatric urology. 2nd, completely revised edition, Springer, Berlin / Heidelberg a. a. 2001, ISBN 978-3-540-64764-5 , Chapter 1: Embryology of the urogenital tract ( full text (PDF)).
- ^ Raimund Stein, Rolf Beetz, Joachim W. Thüroff: Pediatric urology in clinic and practice. 3rd edition, Thieme, Stuttgart / New York 2012, ISBN 978-3-13-674803-9 , p. 440 ff. → Section 37, Urogenital sinus and anomalies of the female genitalia. ( Full text (PDF)).
- ↑ Walther Graumann: Compact textbook anatomy: in 4 volumes. Schattauer, Stuttgart 2004, ISBN 3-7945-2063-7 , p. 322.
- ↑ Vincenzo Puppo: Anatomy and Physiology of the Clitoris, Vestibular Bulbs, and Labia Minora With a Review of the Female Orgasm and the Prevention of Female Sexual Dysfunction. In: Clinical Anatomy. Volume 26, 2013, pp. 134-152 ( researchgate.net ).
-
↑ Erik Schulte: Female Genital . In: Gerhard Aumüller u. a .: anatomy . 3. Edition. Thieme, Stuttgart 2014, p. 808.
B. Fischer, G. Rune: Female sexual organs . In: Detlev Drenckhahn (Ed.): Anatomie. Volume 1 . 17th edition. Urban & Fischer, Munich 2008, p. 841. - ↑ Helen E. O'Connell, John OL DeLanceyo: Clitoral Anatomy in Nullipardous, Healthy, Premenopausal Volunteers using unenhanced Magnetic Resonance Imaging. In: The Journal of Urology . June 2005, Volume 173, No. 6, pp. 2060-2063.
- ↑ In the fiber-rich connective tissue, in addition to parts of collagen fibers, elastic fibers are predominant.
- ↑ Claire C. Yang, Christopher J. Cold, Ugur Yilmaz, Kenneth R. Maravilla: Sexually responsive vascular tissue of the vulva. In: BJU International. Volume 97, pp. 766-772, doi: 10.1111 / j.1464-410X.2005.05961.x
- ↑ Michael Gekle, Erhard Wischmeyer, Stefan founder, Marlen Petersen, Albrecht Schwab: Pocket textbook physiology. Thieme, Stuttgart 2010, ISBN 978-3-13-154031-7 , p. 507 f.
- ↑ H. Ümit Sayin: Doors of Female Orgasmic Consciousness: New Theories on the Peak Experience and Mechanisms of Female Orgasm and Expanded Sexual Response. In: NeuroQuantology. November 2012, Volume 10, No. 4, pp. 692-714, doi: 10.14704 / nq.2012.10.4.627 ; see p. 697 ( researchgate.net full text ).
- ^ Hans Frick, Helmut Leonhardt , Dietrich Starck : Special anatomy . Volume 2. Thieme, Stuttgart 1992, ISBN 978-3-13-356904-0 , p. 251.
- ^ Anton Waldeyer , Anton Mayet: General anatomy, back, abdomen, pelvis, leg. Part 1. de Gruyter, Berlin 1953, p. 263.
- ↑ Daniel Haag-Wackernagel: The female excitation system from the perspective of evolutionary biology . (PDF) Department of Biomedicine, University of Basel, 2017.
- ↑ Smadja A Minh, JPH de Sigalony, JF Aetherr: Role du fascia de Halban dans la physiologie orgasmique feminime. In: Cahiers de Sexuol Clin. 1981, Volume 7, p. 169.
- ↑ Wolf Eicher: Orgasm and orgasm disorders in women. Edition Medicine VCH, Weinheim / Basel 1991, pp. 36–37.
- ^ Wall Nathan Hoag, Janet R. Keast, Helen E. O'Connell: The "G-Spot" Is Not a Structure Evident on Macroscopic Anatomic Dissection of the Vaginal. In: J Sex Med. 2017, Volume 14, pp. 1524-1532 ( researchgate.net ).
- ↑ Adam Ostrzenski: Anatomic documentation of the G-spot complex role in the genesis of anterior vaginal wall ballooning. European Journal of Obstetrics & Gynecology and Reproductive Biology, (2014), pp. 1–6 cosmetic-gyn.com (PDF)
- ↑ Chua Chee Ann: A proposal for a radical new sex therapy technique for the management of vasocongestive and orgasmic dysfunction in women: The AFE Zone Stimulation Technique. In: Sexual and Marital Therapy. Volume 12, 1997, p. 357, doi: 10.1080 / 02674659708408179 .
- ↑ Pelvic floor anatomy bagliodelmarchese.com
- ↑ Frontal section through a woman's pelvis; Anterior view from the abdomen. eref.thieme.de
- ↑ Superficial muscle layers (first picture: "surface / external opening muscles opening" with the laterally lying M. ischocavernosus and the annular Mm. Bulbosponigosus et sphincter ani externus ) and deep muscle layers of the female pelvic floor (second picture: "deep / internal muscles dropping" with the pelvis diaphragm, like the levator ani) pelvicguru.files.wordpress.com
- ↑ connective tissue spaces, fascia layers and pelvic floor muscles; Frontal section eref.thieme.de
- ^ Thomas Weyerstahl: Dual series of gynecology and obstetrics. Thieme, Stuttgart 2013, ISBN 978-3-13-152604-5 , p. 24.
- ↑ K. Fleischhauer, J. Stabesand, W. Zenker (Ed.): Benninghoff - Anatomie. 2nd volume, Urban & Schwarzenberg, Munich 1985, ISBN 3-541-00254-9 , p. 516.
- ↑ K. Karkazis: Looking at and talking about genitalia: understanding where physicians and patients get their ideas about what's normal and what isn't. In: Medical Humanities. Volume 36, No. 2, 2010, pp. 68-69, doi: 10.1136 / jmh.2010.006288 .
- ^ Paula Briggs, Gabor Kovacs, John Guillebaud: Contraception: A Casebook from Menarche to Menopause. Cambridge University Press, Cambridge 2013, ISBN 978-1-107-61466-6 , pp. 15-16.
- ↑ Willibrord Weijmar Schultz, Pek van Andel, Ida Sabelis, Eduard Mooyaart: Magnetic resonance imaging of male and female genitals during coitus and female sexual arousal. In: BMJ. Volume 319, Number 7225, December 1999, pp. 1596-1600, PMID 10600954 , PMC 28302 (free full text).
- ^ Z. Hoch: Vaginal erotic sensitivity by sexological examination. In: Acta Obstet Gynecol Scand. 1986, Vol. 65, No. 7, pp. 767-773.
- ^ V. Puppo, G. Puppo: Anatomy of sex: Revision of the new anatomical terms used for the clitoris and the female orgasm by sexologists. In: Clin Anat. April 2015, Volume 28, No. 33, pp. 293-304.
- ^ Richard K. Winkelmann: The erogenous zones: their nerve supply and its significance. In: Staff Meetings of the Mayo Clinic. 1959, Volume 34, pp. 39-47.
- ^ B. Campbell: Neurophysiology of the clitoris. In: TP Lowry, TS Lowry (eds.): The Clitoris. Green, St Louis 1976, pp. 35-74.
- ^ Theodor H. Schiebler, Horst-W. Korf: Anatomy: histology, history of development, macroscopic and microscopic anatomy, topography. 10th edition, Steinkopff, Darmstadt 2007, ISBN 3-7985-1770-3 , p. 434.
- ↑ Four Nerve Six Pathway Theory of Female Orgasm. In the development of female orgasms, at least six neural pathways operate in the orgasmic reflex arc system. Pudental, pelvic , hypogastric , intercostal and vagus (Nervi splanchnici pelvici) nerves form the main innervation system. There are also at least two oxytocin signaling pathways, while oxytocin acts separately as a neurotransmitter and a hormone. In extended orgasms and ESR orgasms, more than one "orgasm reflex arc path" is activated and triggers an extended orgasm, while many others contribute to the formation of EO or ESR orgasms. researchgate.net
- ↑ One can differentiate between two forms of surface sensitivity, which are part of exteroception: - Protopathic sensitivity for pain and temperature, - Epicritical sensitivity for touch, pressure and vibration
- ↑ LS Baskin, A. Erol, Y. Li, E. Kurzrock, GR Cunha: Anatomical studies of the human clitoris. In: Journal of Urology. (J Urol) Vol. 162, 1999, pp. 1015-1020.
- ↑ Per Olov Lundberg: The peripheral innervation of the female genital organs. In: Sexology. Volume 9, No. 3, 2002, pp. 98-106, full text. (PDF).
- ^ Van Anh T. Ginger, Claire C. Yang: Functional Anatomy of the Female Sex Organs. In: JP Mulhall et al. (Ed.): Cancer and Sexual Health. In: Current Clinical Urology. Volume 13, March 14, 2011, pp. 13-23, doi : 10.1007 / 978-1-60761-916-1_2 , full text. ( Memento of December 22, 2015 in the Internet Archive ) (PDF).
- ↑ Vincent Di Marino, Hubert Lepidi: Anatomic study of the clitoris and the bulbo-clitoral organ. Springer, Heidelberg 2014, ISBN 978-3-319-04893-2 , p. 83.
- ↑ Cheryl Shih, Christopher J. Cold, Claire C. Yang: Cutaneous Corpuscular Receptors of the Human Glans Clitoris: Descriptive Characteristics and Comparison with the Glans Penis. In Journal of Sexual Medicine. Volume 10. No. 7, May 2013.
- ↑ H. Hinghofer-Szalkay: Physiology of the sensory organs. Somatosensory. ( physiologie.cc ).
- ↑ LC Junqueira, J. Carneiro: Histology: Textbook of cytology, histology and microscopic human anatomy. Taking into account the histophysiology. Springer-Verlag, Berlin / Heidelberg / New York 2013, ISBN 978-3-662-07782-5 , p. 537.
- ↑ Cheryl Shih, Christopher J. Cold, Claire C. Yang: Cutaneous Corpuscular Receptors of the Human Glans Clitoris: Descriptive Characteristics and Comparison with the Glans Penis. In: Journal of Sexual Medicine. Volume 10, No. 7, May 2013, pp. 1783–1789.
- ↑ Ferrante S. Gragasin, Evangelos D. Michelakis u. a .: The neurovascular mechanism of clitoral erection: Nitric oxide and cGMP-stimulated activation of BKCa channels. researchgate.net [accessed Nov 18 2018].
- ↑ Burnett AL, Calvin DC, RI Silver, DS Pepas, SG Docimo: Immunohistochemical description of nitric oxide synthase isoforms in human clitoris. In: Journal of Urology. (J Urol) 1997, Volume 158, p. 75.
- ^ RJ Levin: The impact of the menopause on the physiology of genital function. In: menopause. Rev 4, 1999, p. 23.
- ↑ Rosemary Basson, Rosemary McInnes, Mike D. Smith, Gemma Hodgson, Nandan Koppiker: The efficacy and tolerability of sildenafil in women with sexual dysfunction in relation to a sexual excitability disorder. In: Sexology '. Volume 9, No. 3, 2002, pp. 116-124 ( sexuologie-info.de (PDF)).
- ^ A. Goldstein, A. Giraldi, A. Kodigliu, HW van Lunsen, L. Marson, R. Nappi, J. Pfaus, A. Salonia, AM Traish, Y. Vardi: Physiology of female sexual function and pathophysiology of female sexual dysfunction. 2nd international consultation on sexual dysfunction. Paris 2003, chapter 19.
- ↑ A. Hermann et al .: Gases as cellular signal substances. Gas transmitter. In: Biology in Our Time. 2010, No. 40, pp. 185–193, doi: 10.1002 / biuz.201010422 , sbg.ac.at ( Memento from December 3, 2013 in the Internet Archive ) (PDF; 1.3 MB).
- ↑ Th. Boyd: About clitoral and preputial glands, especially in humans and in some animals. In: Archives for Gynecology. Vol. 89, No. 3, 1909, pp. 581-595, doi: 10.1007 / BF01929547 .
- ^ Theodor Heinrich Schiebler: Textbook of the entire human anatomy: cytology, histology, history of development, macroscopic and microscopic anatomy. Springer-Verlag, Heidelberg / Berlin / New York 2013, ISBN 3-662-12240-5 , p. 524.
- ↑ European Patent Office: EP 1 177 190 B1 - European Patent Specification - Use of selective alpha-adrenergic receptor antagonists for the treatment of sexual disorders. Full text. (PDF).
- ↑ Jan Zrzavý, Hynek Burda, David Storch, Sabine Begall, Stanislav Mihulka: Evolution: A reading textbook. Springer-Verlag, Heidelberg / Berlin / New York 2013, ISBN 978-3-642-39696-0 , p. 332 f.
- ↑ Nerve coordination of the sexual reflexes in women, scheme, physiologie.cc/XIII.3a.htm, H. Hinghofer-Szalkay, accessed on August 3, 2018 physiologie.cc
- ^ AE Narjani : Considérations sur les causes anatomique de la frigidité chez la femme. In: Journal Médicale de Bruxelles. Volume April 27, 1924, pp. 776 f.
- ↑ Kim Wallen, Elisabeth A. Lloyd: Female sexual arousal: genital anatomy and orgasm in intercourse. In: Hormones and behavior. Volume 59, number 5, May 2011, pp. 780-792, doi: 10.1016 / j.yhbeh.2010.12.004 , PMID 21195073 , PMC 3894744 (free full text).
- ↑ Filomena de Sousa, Gonzalo Munévar: Sex, Reproduction and Darwinism. Routledge, London / New York 2015, ISBN 978-1-317-32164-4 , p. 114 f.
- ↑ Vincent Di Marino, Hubert Lepidi: Anatomic study of the clitoris and the bulbo-clitoral organ. Springer-Verlag, Heidelberg 2014, ISBN 978-3-319-04893-2 , p. 118 f.
- ↑ Claudia Haarmann: "Downstairs ..." - The shame is not over. Innenwelt-Verlag, Cologne 2005, ISBN 3-936360-15-4 .
- ↑ Mihaela Pavličev, Günter Wagner: Evolutionary Origin of Female Orgasm. In: Journal of Experimental Zoology Part B Molecular and Developmental Evolution. (J Exp Zool B Mol Dev Evol.) September 2016, Volume 326, No. 6, pp. 326-337, doi: 10.1002 / jez.b.22690 .
- ↑ Realdo Colombo: de re anatomica. Quoted from Thomas Laqueur: written on the body. Staging of the sexes from antiquity to Freud . Campus-Verlag, Frankfurt am Main / New York 1992, ISBN 3-593-34623-0 , p. 81.
- ↑ a b c Bernard de Mandeville, Ursula Pia Jauch: A Modest Pamphlet for Public Whorehouses Or An Approach to Fornication as it is now practiced in the UK. Hanser, Munich 2001, ISBN 978-3-446-19989-7 , p. 60, note 55, also p. 140.
- ↑ Thomas Laqueur: On the body: Staging of the sexes from antiquity to Freud. Frankfurt am Main / New York 1992, p. 82.
- ↑ The clitoris and the male penis; Sketch with Kobelt's venous plexus. hindawi.com
- ↑ Sketch of some anatomical structures, such as the Kobelt vein plexus, the uretrovaginal septum or half-ankle fascia between the female urethra and vagina or in the vaginal vestibule , vestibulum vaginae in a sagittal sectional plane hindawi.com
- ^ Georg Ludwig Kobelt: The male and female voluptuous organs of humans and some mammals in anatomical-physiological relationship. Freiburg 1844.
- ↑ Süddeutsche Zeitung: The forgotten lust of women. Retrieved August 20, 2020 .
- ^ Susan Williamson, Rachel Nowak: The truth about women. In: New Scientist . August 1, 1998, pp. 34-35, full text .
- ↑ Helen E. O'Connell, John M. Hutson, Colin R. Anderson, Robert J. Plenter: Anatomical relationship between urethra and clitoris. In: Journal of Urology. (J Urol) June 1998, Vol. 159, No. 6, pp. 1892-7.
- ↑ Sensitive onion . In: Der Spiegel . No. 33 , 1998 ( online ).
- ↑ Clitoris, the beautiful unknown. ( Memento from September 11, 2011 in the Internet Archive ) - Theme evening: The lust of women. On: Arte on January 1st, 2004, 10:15 p.m.
- ^ Nancy Scheper-Hughes: Virgin territory. The male discovery of the clitoris. In: Medical Anthropology Quarterly. 1991, No. 5, pp. 25-28.
- ↑ Thomas Gohla: Surgical reconstruction of the clitoris after genital mutilation (FGM). In: MÄC magazine for aesthetic surgery. Volume 3, No. 12, Volume 6, 2012, full text. (PDF).
- ↑ Vulva Vagina Commission in the Gynecological Oncology Working Group (AGO): Interdisciplinary S2k guidelines for the diagnosis and treatment of vulvar cancer and its preliminary stages. Zuckschwert, Munich / Vienna / New York 2009, ISBN 978-3-88603-947-0 , full text. (PDF).
- ↑ Willibald Pschyrembel: Pschyrembel, medical dictionary. 259th, revised edition. De Gruyter, Berlin / New York 2002, ISBN 978-3-11-016523-4 , p. 863: Clitoridectomy .
- ↑ G. Bastert, SD Costapp: Vulvar carcinoma. In: Siegfried Seeber: Therapy Concepts Oncology. Springer-Verlag, Berlin (inter alia) 1993, ISBN 978-3-540-56872-8 , pp. 501-508.