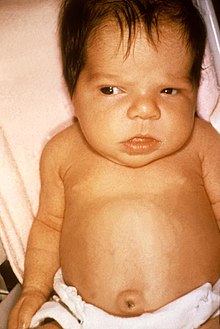
Newborn jaundice
| Classification according to ICD-10 | |
|---|---|
| P58.- | Neonatal icterus due to other increased haemolysis |
| P59.- | Neonatal icterus from other and unspecified causes |
| ICD-10 online (WHO version 2019) | |
The term neonatal jaundice ( neonatal , jaundice of the newborn ; lat. Icterus neonatorum ) describes the phenomenon of yellowing of the skin , sclera and other tissues by incorporation of bilirubin , a breakdown product of hemoglobin hemoglobin .
About 60% of all mature, healthy newborns develop a more or less pronounced jaundice ( jaundice ) in the first days of life , but in most cases this is physiological and completely harmless. Storage generally reaches its maximum around the fifth day of life and then gradually decreases.
The bilirubin concentration can, however, rise so much that bilirubin enters the brain via the blood-brain barrier and permanently damages particularly sensitive structures. One then speaks of a kernicterus . To avoid this, newborns with greatly increased bilirubin levels are treated preventively with light therapy ( phototherapy ) with short-wave light of the visible spectrum .
root cause
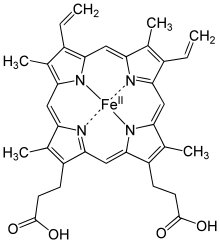
When the red blood pigment hemoglobin, more precisely its iron-binding heme group from disintegrating red blood cells, the erythrocytes , is broken down , biliverdin is first produced and from this free, so-called unconjugated bilirubin. This is not water-soluble, but fat-soluble. So that it can be transported to the liver for further metabolism and excretion , it is bound to the protein molecule albumin in the blood . In the liver cell, the free bilirubin is linked to glucuronic acid by the enzyme glucuronyl transferase ( glucuronidized ) and thereby converted into a water-soluble form (see biotransformation ). The so-called direct, conjugated bilirubin is produced. This can now be excreted with the bile . In the intestine , excreted conjugated bilirubin is at least partially deconjugated again and absorbed back into the bloodstream (so-called enterohepatic circulation ). In newborns, the lifespan of the erythrocytes is shortened to around 70 days, which means that a particularly large amount of this breakdown product is produced.
In addition, the glucuronyltransferase is not yet fully active due to the immaturity of the liver. These factors mean that more bilirubin is formed in the first few days of life than the liver can excrete. A possible biological function of increased bilirubin in the first days of life could be due to the fact that the bilirubin is able to free oxygen - radical trap. As a result, it can potentially protect the children from diseases that are favored by oxidative stress.
to form
In paediatrics, there are four types of progression:
- Physiological neonatal icterus: This begins between the 3rd and 6th day of life and regresses by the 10th day of life.
- Icterus praecox: This usually occurs on the first day of life due to blood group incompatibility .
- Icterus gravis: This is characterized by very high bilirubin concentrations of more than 20 mg / dl in mature newborns, premature babies have lower limits.
- Icterus prolongatus: This persists for more than two weeks.
Risk factors
All conditions that lead to an increased breakdown of hemoglobin can favor newborn jaundice. These include, on the one hand, bruises that can occur, for example, during childbirth (Latin sub partu ), such as the cephalic hematoma or the birth tumor ( caput succedaneum ). On the other hand, an increased breakdown of erythrocytes ( hemolysis ) in the case of blood group incompatibilities between mother and child can lead to an increased attack of bilirubin. The classic Rhesus incompatibility (mother rh-negative, child Rh-positive) has become rare due to improved preventive measures. However, an intolerance in the area of blood group characteristics AB0 (mother blood group 0, child blood group A or B) can also result in an increased breakdown of red blood cells. Finally, there are also a number of congenital diseases that are associated with haemolysis ( haemolytic anemia ), such as spherical cell , sickle cell anemia or glucose-6-phosphate dehydrogenase deficiency . The question of whether a sibling has ever had severe jaundice as a newborn is therefore of particular importance. Delayed emptying of the intestine also increases the risk of increased jaundice in the first few days of life due to increased absorption of the split bilirubin.
Complications
Neonatal icterus would not actually be a problem as it is a common phenomenon which is basically normal or physiological. However, if the amount of (unconjugated, fat-soluble) bilirubin exceeds a threshold value, it can cross the blood-brain barrier and enter the brain from the bloodstream. There it is deposited in certain structures, the so-called basal ganglia . These are eventually permanently damaged under certain circumstances, so-called kernicterus occurs . The exact level of the dangerous concentration is not known, but it is certainly well beyond a concentration of 20 mg / dl (340 µmol / l). Children whose blood-brain barrier is not (yet) fully functional for other reasons are particularly at risk for this complication. This includes all premature infants , but also term infants with acute illnesses that lead to impairment of the blood-brain barrier. These include, for example, severe oxygen deficiency during childbirth ( asphyxia ), over-acidification of the body ( acidosis ) caused by this or other causes , low blood sugar ( hypoglycemia ), lack of albumin (hypoalbuminemia), shock or bacterial infections ( sepsis ).
diagnosis
In all newborns who develop visible jaundice, the bilirubin circulating in the blood should be determined no later than 72 hours after birth. This can be done with the blood collection, which is necessary for the newborn screening anyway . Further routine bilirubin checks can also be carried out without blood with a photometric measurement of the bilirubin concentration in the skin (so-called transcutaneous measurement with a multispectral device). Especially in the case of premature jaundice ( icterus praecox ) on the first day of life, a thorough examination by a pediatrician should also be carried out to ensure that there is no underlying complicating disease.
Differential diagnosis
Even if physiological neonatal icterus is a common diagnosis, other underlying diseases must of course always be ruled out. First of all, a differentiation of the yellow blood pigment into conjugated (direct) and unconjugated (indirect) bilirubin should ensure that only the unconjugated bilirubin is affected. Otherwise, the cause of the jaundice must be sought on the one hand in diseases of the liver itself in the form of infections or congenital metabolic diseases. On the other hand, there may be a problem with the outflow of bile in the presence of congenital obstruction of the bile duct ( bile duct atresia ). Even if the indirect bilirubin alone is increased, congenital diseases that are associated with an increased blood fall must be ruled out. A distinction must be made here between the immunological causes in the presence of a blood group intolerance and hereditary diseases (see also the section on risk factors).
therapy
General measures
Supportive measures for newborns that are visibly yellow but not yet at risk can be given additional fluids and early frequent feeding. This is intended to stimulate the intestinal activity and thus prevent the enterohepatic circulation. However, there is no scientifically proven proof of effectiveness for these measures.
Phototherapy
For all newborns whose jaundice exceeds age-related thresholds set by the professional associations, treatment by irradiation with blue light with a wavelength of ideally 459 nm (practice: 450–475 nm) must be initiated in good time to prevent kernic terus. For otherwise normal newborns with a gestational age over 38 + 0 weeks and an age of at least 72 hours, the threshold value is currently 20 mg / dl (340 µmol / l). These short-wave light rays are able to destroy a double bond in the unconjugated bilirubin . The resulting water-soluble lumirubin can be excreted without glucuronidation via the bile and with the kidneys via the urine . In addition to conventional lamps or light-emitting diodes , which can be placed over the bed or the incubator , blue-light fluorescent tubes and fiber-optic light- emitting mats are available for so-called phototherapy , which illuminate the child from below. Depending on the course, the therapy is applied for one to several days, possibly with interruptions between two meals each time (intermittent therapy).
Phototherapy is also burdened with side effects, which is why it should not be used uncritically without real necessity. Firstly, the retina of the eye (which may retina ) are damaged by the very high energy light beams. Therefore, the eyes of the children to be treated must be covered with appropriate “glasses”. There is also increased water and salt loss through the skin and inflammation of the conjunctiva of the eyes ( conjunctivitis ) and the skin ( dermatitis ) as well as disturbances in heat regulation. Last but not least, phototherapy also means separating mother and child. Epidemiological studies describe a weak statistical association between phototherapy and the later occurrence of skin changes such as melanocytic nevi or café-au-lait spots as well as between phototherapy and acute myeloid leukemia
Exchange transfusion
In the case of a particularly rapid and rapidly increasing course, for example in the context of a rhesus incompatibility, phototherapy may not be sufficient to break down enough bilirubin. Blood exchange transfusions should be used if bilirubin levels are greater than 30 mg / dl . In this process, the newborn's own blood is withdrawn via a large blood vessel, usually the umbilical vein , and stored blood of blood group 0 rh is negatively transfused through another vein until the entire blood volume has been exchanged. This is to stop the accelerated breakdown of one's own blood and prevent a further increase in the bilirubin concentration in harmful areas.
forecast
The prognosis of neonatal jaundice - given therapy - can be assessed as very good overall. An American study examined 140 mature, otherwise healthy newborns with bilirubin levels of 25 to over 30 mg / dl (425 to over 510 µmol / l). Most of the children were treated with phototherapy, and in five cases also with exchange transfusions. Compared to a comparison group, the authors could not find any lasting neurological impairments.
history
Although newborn jaundice is a common phenomenon that must have been noticed by medical professionals of all ages, there is no record of it from ancient times. The first reports are probably from Morgagni in the early 18th century. At least, Hervieux quotes descriptions of 15 yellow newborns. In 1785 Jean Baptiste Thimotée Baumes received a prize from the University of Paris for his work on the treatment of jaundice in newborns. He was of the opinion that the jaundice was caused by a delayed elimination of the meconium , as the first bowel movement of the newborn is called. As a therapy, he consequently recommended breast milk , especially colostrum . In this way, he recognized a pathophysiological mechanism in his day that is in line with current knowledge.
Jacques François Édouard Hervieux, already mentioned above, defended his dissertation De l'Ictère des Nouveau-nés (German translation On the jaundice of newborns ) in 1847 , which was given the highest grade ( très satisfait , very satisfactory ) by the examiners . In it, he rejected most of the theories of his predecessors and presented his own observations on 45 children, 44 of whom had died and had been autopsied by him. Still, he must have seen a number of other surviving children. In any case, he describes newborn jaundice as a physiological condition that is not dangerous in and of itself and that disappears on its own. The typical time sequence, the progression from head to foot, the frequency of almost two thirds of all newborns and the good prognosis in the absence of complicating comorbidities were already recorded by Hervieux in a way that could still be found in a textbook today.
The German pathologist Johannes Orth is considered to be the first to describe kernicterus . In 1875 he published the results of the autopsy of a child who died two days after birth with pronounced jaundice with no other obvious symptoms. He described an intense yellowing of the entire brain with particular emphasis on the basal ganglia and pointed out that such yellowing of the nervous system is absent in adults with jaundice. The term kernikterus was first coined by Georg Schmorl in 1904 . Furthermore, it was used not only for the pathological-anatomical picture of the brain of children who died with jaundice, but also for the neurological clinical picture from which the survivors of severe neonatal jaundice suffered.
Individual evidence
- ↑ a b c M. Marcinkowski, C. Bührer: AWMF guidelines. Hyperbilirubinemia - Diagnosis and Therapy in Mature Healthy Newborns. AWMF, Düsseldorf, 2003 [1]
- ↑ DA Benaron, FWBowen, variation of initial serum bilirubin rise in newborn infants with type of illness. In: The Lancet 1991; 338: 78-81 PMID 1676469
- ↑ T. Hegyi, E. Goldie, M. Hiatt, The protective role of bilirubin in oxygen-radical diseases of the preterm infant. In: J Perinatol . 1994; 14: 296-300 PMID 7965225
- ↑ Berthold Koletzko: Paediatrics
- ↑ a b M. Berns: Hyperbilirubinemia in the mature newborn - limits of intervention. In: Monthly Pediatric Medicine 2006; 154: 835-843
- ^ J. Oláh, E. Tóth-Molnár, L. Kemény, Z. Csoma: Long-term hazards of neonatal blue-light phototherapy . In: The British Journal of Dermatology . tape 169 , no. 2 , August 2013, ISSN 1365-2133 , p. 243-249 , doi : 10.1111 / bjd.12335 , PMID 23521230 .
- ↑ Kathrin Wintermeier, Martina von Poblotzki, Orsolya Genzel-Boroviczény, Sandra Vogel, Klaus Schotten: Neonatal blue light phototherapy increases café-au-lait macules in preschool children . In: European Journal of Pediatrics . tape 173 , no. November 11 , 2014, ISSN 1432-1076 , p. 1519-1525 , doi : 10.1007 / s00431-014-2349-8 , PMID 24942237 .
- ↑ S. Cnattingius, M. Zack, A. Ekbom, J. Gunnarskog, M. Linet: Prenatal and neonatal risk factors for childhood myeloid leukemia . In: Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, Cosponsored by the American Society of Preventive Oncology . tape 4 , no. 5 , July 1995, ISSN 1055-9965 , pp. 441-445 , PMID 7549797 .
- ↑ Danise Podvin, Carrie M. Kuehn, Beth A. Mueller, Michelle Williams: Maternal and birth characteristics in relation to childhood leukaemia . In: Pediatric and Perinatal Epidemiology . tape 20 , no. 4 , July 2006, ISSN 0269-5022 , p. 312-322 , doi : 10.1111 / j.1365-3016.2006.00731.x , PMID 16879503 .
- ↑ [2]
- ↑ TB Newman et al .: Outcomes among newborns with total serum bilirubin levels of 25 mg per deciliter or more. In: New England Journal of Medicine 2006; 344: 1889-1900 PMID 16672700
- ^ TWR Hansen: Pioneers in the Scientific Study of Neonatal Jaundice and Kernicterus . In: Pediatrics 2000; 106 ISSN 0031-4005 .