Thyroid cancer
| Classification according to ICD-10 | |
|---|---|
| C73 | Malignant growth of the thyroid gland |
| ICD-10 online (WHO version 2019) | |
When thyroid cancer ( thyroid cancer , lat. Struma maligna ) is a malignant neoplasm of the thyroid gland called. Thyroid cancer is divided into several types, the most common of which often occurs in young adulthood. Disruptive thyroid nodules are usually the first symptom. In addition to ultrasound , scintigraphy is also used for the examination . Treatment in most cases consists of surgery ( thyroidectomy ) and radioiodine therapy .
frequency
Thyroid cancer is the most common tumor of the endocrine organs . In Germany (2012) 1820 men and 4390 women fell ill per year, 330 men and 490 women died. In Austria, a total of diseased annual average (2008/2010) 952 (261 men, 691 women), for the United States, the annual incidence rate (is incidence ) given as 34,000.
In Germany, thyroid carcinoma ranks 14th among the incidence of malignant tumors among women and 15th among men. The age peak is on average 52 years for women and 55 years for men. However, the maximum age varies depending on the type of cancer:
- papillary type: between 35 and 60 years of age
- follicular type: between 40 and 50 years of age
- anaplastic type: approx. 60 years of age
- Medullary type: approx. 40. – 50. age
In the last few decades the incidence of thyroid cancer has increased worldwide. There are clear differences depending on the region and ethnic group. The increase is mainly due to small (<2 cm) papillary carcinomas and younger patients, which results in a shift to patient groups with a more favorable prognosis.
Based on autopsies and operations, it is assumed that, depending on the size considered, 2 to 36% of the population have hidden micro-carcinomas less than 10 mm in diameter in the thyroid gland. Of these, a maximum of 0.5% becomes clinically relevant.
causes
The individual causes are not fully understood. There is a causal connection with iodine deficiency (about 2.3 times higher risk). Also radiation (especially in childhood and adolescence) plays - as with many cancers - a crucial role: by the atomic bombing of Hiroshima and Nagasaki rose in the affected areas, the risk of thyroid cancer by a multiple of. The same applies to the territories after the Chernobyl disaster of a massive fallout (fallout) were affected.
In Germany, the authorities have large quantities of tablets with potassium iodide ready, which should be distributed to people under 45 years of age in the event of a reactor accident in order to achieve an iodine blockade of the thyroid gland.
Symptoms
Typically, a lump is noticed in the thyroid area. The thyroid gland can be enlarged ( goiter ) or remain normal. Enlarged cervical lymph nodes can also appear in front of a palpable thyroid nodule. Swallowing disorders, hoarseness as an expression of vocal cord nerve paralysis, inability to swallow the thyroid gland, coarse consistency and overgrown lymph nodes are late symptoms of advanced cancer.
Investigations
- When palpating the thyroid gland, rough and non-swallowable nodes and accompanying swelling of the cervical lymph nodes are suspicious of a malignant change.
- On ultrasound , thyroid carcinomas usually appear hypoechoic, rarely hyperechoic. Inflammation or calcifications can also be hypoechoic; cysts are usually anechoic. Medullary thyroid carcinoma often shows small calcifications on sonography.
- On thyroid scintigraphy , cold nodules are carcinoma in 3% of cases (single cold nodule: 15%), otherwise inflammation, fibrosis, calcifications, cysts, bleeding or adenomas.
- In the case of cold nodules, a fine needle puncture with puncture cytology may be indicated (assessment of the removed cells under the microscope ).
- Blood tests:
- The thyroid hormone levels ( TSH , fT3 , fT4 ) do not provide any information about a possibly existing thyroid carcinoma.
- The tumor marker thyroglobulin is used to assess the course of differentiated, non-medullary thyroid carcinomas after surgery. Elevated values also occur with inflammation of the thyroid gland or goiter and are only of diagnostic importance after at least an almost complete removal of the thyroid gland.
- The tumor marker calcitonin , on the other hand, indicates medullary thyroid carcinoma or C-cell hyperplasia even before a possible thyroid operation.
- A laryngoscopy is usually done before and after a thyroid operation to determine whether the vocal cord nerves ( recurrent nerve ) may be damaged .
- The exclusion of the diagnosis of thyroid carcinoma is only possible with absolute certainty by surgical removal of the suspicious parts of the thyroid and subsequent assessment of the cell tissue ( histology ).
Types of thyroid cancer
Depending on the starting tissue, a distinction is made between the following types:
Differentiated carcinomas
- Papillary thyroid carcinoma (PTC) 60–80%
These carcinomas originate in the thyrocytes and form finger-like (papillary) structures. They are the most common malignant neoplasms of the thyroid gland, accounting for 50–80% of all thyroid carcinomas. They metastasize mainly via the lymph vessels (lymphogenic metastasis) into the lymph nodes of the neck. These can then increase in size and can be felt. Papillary carcinomas often affect women in their 3rd to 4th grade. Decade of life. Radiation exposure (for example, in the context of therapeutic radiation to the head and neck region or the Chernobyl reactor disaster ), Hashimoto's thyroiditis and various genetic syndromes ( FAP syndrome and Cowden syndrome ) are considered to be favorable factors for its development . Pathohistologically, eosinophilic calcium accumulations ( psammoma bodies ) can be detected here.
The incidence of thyroid cancer has increased in the United States. A SEER analysis (Surveillance, Epidemiology, and End Results) of several American states showed an incidence of 4.9 per 100,000 inhabitants in 1975 , compared with 14.3 in 2009. The increase is almost entirely due to a greater incidence of papillary carcinomas. Their annual incidence has increased from 3.4 to 12.5 per 100,000 inhabitants. There is also a gender difference: women from 6.5 to 21.4; Men from 3.1 to 6.9. Since at the same time the mortality from thyroid carcinomas remained constant at 0.5 per 100,000, it is assumed that the increase is due to a better diagnosis of small papillary thyroid carcinomas.
- Follicular thyroid carcinoma (FTC) 10-30%
In this carcinoma, the tissue structure is largely similar to that of a mature or developing thyroid gland. The cancer cells start from the thyrocytes and form settlements (hematogenous metastasis) in the lungs, skeleton and brain , mainly via the bloodstream . Follicular carcinoma accounts for 20–50% of all thyroid carcinomas. It often affects women in their 4th and 5th decades of life. An immunohistochemically detectable expression of thyroglobulin is typical for follicular carcinomas of the thyroid gland .
Undifferentiated or anaplastic cancers
This carcinoma (around 5% of all cases) no longer shows any similarities in its fine structure with the original thyroid tissue and is therefore also referred to as undifferentiated carcinoma. It grows aggressively into the surrounding tissue and metastasizes both lymphogenically and hematogenously. This type accounts for around 5–10% of thyroid carcinomas. It rarely develops before the age of 60; a gender preference does not show it. Since the undifferentiated carcinoma cells no longer participate in iodine metabolism in this type of tumor, radioiodine therapy does not make sense.
Medullary carcinoma
Medullary thyroid carcinoma (also known as "C-cell carcinoma") does not originate from the thyrocytes (the iodine-storing thyroid cells), but from the parafollicular , calcitonin- producing cells (so-called C-cells), which due to developmental relationships in the Thyroid gland, but not related to the actual thyroid function (thyrocytes) . About 5–10% of all thyroid cancers belong to this type.
First described in 1959 as a separate entity alongside the differentiated and undifferentiated thyroid carcinomas, the medullary carcinoma occurs familial (approx. 15%) or sporadic (approx. 85% of medullary thyroid carcinomas; peak between 50 and 60 years of age). In the familial type, a distinction is made between the familial occurrence of medullary thyroid carcinoma (FMTC) and the syndrome of multiple endocrine neoplasia types 2A and 2B . The familial (ie hereditary) form is caused by mutations in the RET gene. When diagnosing medullary thyroid carcinoma, a genetic analysis should always be carried out (after the patient has been informed and given his consent), since other family members may have inherited the genetic defect. If other family members also have the corresponding RET mutation, prophylactic thyroid surgery (thyroidectomy) may be recommended, depending on the type of mutation.
The most sensitive tumor marker of medullary carcinoma is the calcitonin produced by the C cells . When the calcitonin level was elevated, a pentagastrin test was previously carried out to further differentiate between benign hyperplasia of the C cells and a malignant event . Since the pentragastrin test is no longer available, calcium is used today for stimulation or basic gender-specific limit values are used, which lead to the same results.
In tumor follow-up, increased calcitonin levels in the blood serve as an indicator of a relapse. Since the C cells do not take part in iodine metabolism, radioiodine therapy is also not useful in medullary thyroid carcinoma.
Treatment of localized thyroid cancer
The following describes the principles of treatment of thyroid cancer localized to the thyroid gland or metastatic to the regional lymph nodes.
Surgical thyroid removal
In principle, the thyroid gland must be completely removed in the case of thyroid cancer ( thyroidectomy ). This also applies to ectopic thyroid tissue (see Thyroid # disorders of the organ system ).
The exception is the so-called micro carcinoma. The papillary thyroid carcinoma with the staging pT1a N0 M0 is called microcarcinoma . Here, pT1a denotes a single tumor with a tumor diameter of <1 cm, measured in pathology , N0 the lack of evidence of tumor involvement in the local lymph nodes and M0 the absence of distant metastases. In addition, the tumor should not be found in the peripheral area of the thyroid tissue and should not exceed the thyroid capsule. In this case, the therapeutic approach is adapted to the low risk assessment: only the affected thyroid lobe is surgically removed and a subsequent radioiodine therapy (ablation) is dispensed with.
In addition to the removal of the thyroid gland, the lymph nodes of the thyroid area are occasionally removed (so-called lymphadenectomy , also known as neck dissection ), since the lymph nodes can be affected by cancer. This is recommended, at least for papillary and follicular thyroid carcinoma, only if there is clinical evidence or suspicion of regional lymph node metastasis, i.e. not prophylactically. For medullary thyroid cancer, the relevant guidelines recommend unilateral or even bilateral cervical lymphadenectomy.
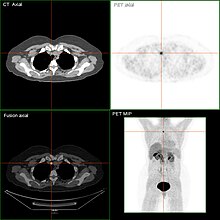
Radioiodine therapy
After thyroid surgery, in certain cases of iodine- storing carcinomas, radioiodine therapy is carried out to remove the thyroid tissue that has remained postoperatively ( ablation ). In this case, radioactive iodine-131 administered, which concentrates exclusively in the thyroid tissue. Due to the physical properties of iodine-131 (predominantly β-emitters ), neighboring structures are only slightly affected by the radiation. Certain other organs (salivary glands, sweat glands, stomach lining, kidneys, bladder) are only involved in the excretion of iodine and also receive a low dose of radiation.
An effective ablation can only be performed if TSH has been adequately stimulated beforehand . This is achieved either by withdrawing thyroid hormones or by administering rhTSH. In the case of thyroid hormone withdrawal, the missing hormones are initially not replaced after the operation, which leads to marked hypothyroidism with z. T. leads to considerable physical and psychological stress for the patient. Alternatively, since 2005, the TSH level in Europe can also be brought to the desired level for ablation ( radioiodine therapy ) by administering genetically engineered TSH ( rhTSH , recombinant human TSH) . From 2007 there will be special DRGs ( Diagnosis Related Groups ) in Germany for the use of the very expensive rhTSH, so that patients of the statutory health insurance funds are increasingly being pretreated with rhTSH for radioiodine therapy. The rhTSH is injected intramuscularly (im) on two consecutive days . In the following days the TSH level rises for a short time and then falls again quickly. For optimal absorption of radioactive iodine, it is of crucial importance that the TSH value is as high as possible. Precise time management is therefore essential when administering rhTSH. Certain constellations, such as the use of anticoagulant substances (e.g. Marcumar ) as a contraindication for i. Administration of m. or a lack of certainty as to whether and when the ablation should be carried out can speak against the use of the rhTSH and in favor of therapy in hypothyroidism.
Subsequent thyroid hormone therapy
After the operation, replacement of the thyroid function with artificial thyroid hormones will begin . For this purpose, L-thyroxine (free T4) is usually given. For the first dose of L-thyroxine, the rule of thumb is that a person needs 2 micrograms of L-thyroxine per kilogram of body weight when there is no more thyroid gland. The TSH value is used to control the correct dosage. At this point in treatment, the target value for TSH is 0.05–0.1 mU / l (the even more extensive suppression of TSH that was previously propagated is no longer recommended as a risk factor for heart attacks and strokes due to the stress on the cardiovascular system ). L- carnitine can also be used to reduce symptoms of overactive thyroid . However, there is still no experience with long-term use of L-carnitine.
Check-ups
After six to twelve months (after three months at the earliest), in certain cases the result of radioiodine therapy should be documented with so-called radioiodine diagnostics . During hormone withdrawal (four weeks before the examination, no intake of L- thyroxine), a small amount of iodine-131 is administered and the distribution in the body is determined after 48 hours with a scintigraphy . For this radioiodine diagnosis, hormone withdrawal is no longer necessary - here since 2001 (see above). When using rhTSH to prepare for radioiodine diagnostics, however, it must be borne in mind that the rhTSH must also be administered again for a possibly necessary new radioiodine therapy.
Another parameter is the Tg value ( thyroglobulin ) in the blood as a measure of the number of thyroid cells in the organism. If there are still thyroid remnants in the neck area or iodine-storing metastases (foci), another radioiodine therapy is connected. In this case, another radioiodi diagnosis is carried out after three months. If both test results are negative (low to no longer detectable Tg and no noticeable iodine storage in the body), radioiodine diagnostics are considered normal. Then another radioiodine test will be done to confirm the results in another nine months. Thereafter, regular checks of the tumor marker thyroglobulin are usually carried out for life, for example once a year. Depending on the risk assessment of the individual tumor ( low , intermediate or high risk ) and the response to therapy ( excellent, indeterminable, biochemically incomplete or structurally incomplete response), different target ranges for the TSH value apply throughout life (from 0.05-0.1 mU / l to <2.0 mU / l) with the dosage of thyroid hormones.
For control and follow-up care, there are now newer guidelines in which the ultrasound examination of the neck and the determination of the tumor marker thyroglobulin under stimulation (rhTSH) are of greater importance, while radioiodine diagnostics play a much smaller role than in the procedure described above.
Treatment of advanced thyroid cancer
In the following, advanced carcinoma is understood to be thyroid carcinoma with distant metastases (e.g. lung metastases) or inoperable thyroid carcinoma. A complete cure is usually no longer possible here. The aim of the therapy is to extend life with the highest possible quality of life and to reduce tumor-related symptoms. Even if distant metastases are present, the prognosis can still be relatively favorable. Some patients with medullary thyroid cancer and distant metastases live with it for decades.
The therapy should be discussed in an interdisciplinary manner, i. H. in collaboration with endocrinologists, nuclear medicine specialists, oncologists, surgeons and radiation therapists. Since 2015 there has also been a study group that maintains a nationwide registry of rare thyroid tumors .
Several tyrosine kinase inhibitors (TKIs) have been approved for advanced thyroid cancer for a number of years : for metastatic differentiated thyroid cancer that no longer responds to radioiodine therapy , lenvatinib and sorafenib ; for advanced medullary thyroid cancer cabozantinib and vandetanib . The first use of tyrosine kinase inhibitors should be done by a tumor board , which consists of doctors who have experience with advanced thyroid carcinoma, as these thyroid carcinomas can often only be observed over several years with a good quality of life.
A tyrosine kinase inhibitor has not yet been approved for anaplastic thyroid carcinoma . A combination of surgery, percutaneous radiation and chemotherapy as well as inclusion in studies is recommended here as the first therapy.
forecast
Differentiated carcinomas
The chances of recovery from differentiated thyroid carcinomas are generally very good. Usually, average 10- year survival rates of over 90% for the papillary and approx. 80% for the follicular variant (for treatment) are given. The prognostic factors include the patient's age and the size, extent and histological differentiation of the tumor; Lymph node metastases do not seem to have a major impact on the prognosis. Consistent follow-up care is extremely important because of the increased risk of recurrence.
Medullary and anaplastic carcinoma
The following 5-year survival rates apply on average (with treatment):
- Medullary carcinoma: 60–70%
- Anaplastic carcinoma: approx. 5%
Similar diseases
The following diseases can cause symptoms similar to thyroid cancer:
- cyst
- Struma nodosa ( cold lump / hot lump )
- Adenoma
- Metastases (e.g. from a breast cancer )
Self help
Due to the rarity of thyroid cancer, it is extremely difficult for patients to find those affected to exchange experiences, so there are only a few local self-help groups . At the German federal level, there are three self-help organizations (the Thyroid League Germany, the Association of the Federal Association of Thyroid Cancer and the C-Cell Carcinoma self-help group) that advocate the interests of thyroid cancer patients and provide practical information (for example, the correct intake of thyroid hormones, Depending on the type of tumor, possibly a low-iodine diet before radioiodine therapy) and provide critical information about new studies and current guidelines .
literature
- S2k guidelines for the operative therapy of malignant thyroid diseases of the German Society for General and Visceral Surgery eV (DGAV). In: AWMF online (as of 2012)
- Bryan R. Haugen et al .: 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer, THYROID Volume 26, Number 1, 2016
- Christian Hubold, Hendrik Lehnert : Classification and Clinical Diagnosis of Thyroid Carcinoma - Benign Nodules or Treatment-Relevant Carcinoma? In: The clinic doctor. 41, 2012, pp. 458-463, doi: 10.1055 / s-0032-1330946 .
- Oliver Gimm: Medullary thyroid carcinoma - special features, diagnostics, therapy and aftercare. In: The clinic doctor. 41, 2012, pp. 476-480, doi: 10.1055 / s-0032-1330949 .
- Alexander Iwen, Hendrik Lehnert, Georg Brabant: Non-medullary thyroid carcinoma - New strategies and current drug therapy concepts. In: The clinic doctor. 41, 2012, pp. 482-285, doi: 10.1055 / s-0032-1330950 .
Web links
Individual evidence
- ^ Robert Koch Institute : Thyroid Cancer , accessed on December 2, 2016
- ↑ Thyroid (C73) - cancer incidence, annual average (2008/2010). Statistics Austria, accessed on March 23, 2013 .
- ^ R Michael Tuttle et al .: Overview of the management of differentiated thyroid cancer . UpToDate 2008, version 16.2
- ↑ a b M. Luster: What is the consequence of the increasing incidence of thyroid carcinomas? In: H. Dralle (Hrsg.): Thyroid 2009. Quality standards in thyroid medicine. Berlin 2010, ISBN 978-3-86541-386-4 .
- ^ Doctors newspaper (ed.): Papillary carcinoma most often . April 25, 2018.
- ↑ C. Reiners et al. a .: Struma maligna - thyroid carcinoma. In: German Medical Weekly . 2008; 133, No. 43, pp. 2215-2228.
- ↑ Christoph Reiners: Diagnosis, therapy and follow-up care of thyroid carcinoma. 3rd edition . Bremen 2010, ISBN 978-3-8374-2112-5 , pp. 12 .
- ↑ H. Bertelsmann, M. Blettner: Epidemiology and risk factors for thyroid cancer. ( Memento from September 19, 2011 in the Internet Archive ) WG Epidemiology and Medical Statistics of the University of Bielefeld, page 16ff
- ↑ a b c U.-N. Riede, M. Werner, H.-E. Schäfer (Ed.): General and special pathology. Thieme, Stuttgart 2004, ISBN 3-13-683305-8 .
- ^ Louise Davies, H. Gilbert Welch: Current thyroid cancer trends in the United States . In: JAMA Otolaryngology-- head & neck surgery . tape 140 , no. 4 , 2014, ISSN 2168-619X , p. 317-322 , doi : 10.1001 / jamaoto.2014.1 , PMID 24557566 .
- ^ A b P. E. Goretzki, K. Schwarz, B. Lammers: Surgery of the thyroid malignancies. In: ENT. 2013, 61, pp. 71-82. doi: 10.1007 / s00106-012-2639-2 , also published in: Der Onkologe . 2013, 8, pp. 673-684.
- ↑ Caterina Mian, et al: Refining Calcium Test for the Diagnosis of Medullary Thyroid Cancer: Cutoffs, Procedures, and Safety . In: The Journal of Clinical Endocrinology & Metabolism, Volume 99, Issue 5, 1 May 2014, Pages 1656-1664, . doi : 10.1210 / jc.2013-4088 .
- ↑ DGN recommendation for action (S1 guideline) Iodine-131 whole-body scintigraphy in differentiated thyroid carcinoma . In: AWMF . Status: 7/2017 edition. Register number: 031-013.
- ↑ a b Bryan R. Haugen, et al: 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer . In: THYROID . Volume 26, Number 1, 2016, doi : 10.1089 / thy.2015.0020 .
- ^ LJ Wirth, DS Ross, GW Randolph, ME Cunnane, PM Sadow: Case records of the Massachusetts General Hospital. Case 5-2013. A 52-year-old woman with a mass in the thyroid. In: N Engl J Med. 2013 Feb 14; 368 (7), pp. 664-673. doi: 10.1056 / NEJMcpc1210080 . PMID 23406032
- ↑ a b Julia Wendler, et al .: Clinical presentation, treatment and outcome of anaplastic thyroid carcinoma: results of a multicenter study in Germany . In: European Journal of Endocrinology . 2016, doi : 10.1530 / EJE-16-0574 .
- ↑ Austrian Society for Surgical Oncology: prognosis of differentiated (papillary, follicular) thyroid carcinoma ( Memento of March 5, 2009 in the Internet Archive )
- ↑ Medical University of Vienna ( Memento of the original from October 8, 2012 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. : Prognosis of differentiated (papillary, follicular) thyroid carcinoma.


