De Quervain's subacute thyroiditis
| Classification according to ICD-10 | |
|---|---|
| E06.1 | Subacute thyroiditis |
| ICD-10 online (WHO version 2019) | |
The subacute thyroiditis de Quervain is a disease of the thyroid gland named after Fritz de Quervain who first described it .
The cause of de Quervain's subacute thyroiditis is still largely unclear. The disease usually begins subacute , i.e. within a few days. This leads to an inflammation of the thyroid gland, a thyroiditis , which is histologically characterized by typical giant cells . It is usually associated with a slightly enlarged thyroid gland (goiter) , pronounced local symptoms such as severe pain in the throat, ear and jaw region and difficulty swallowing, as well as general complaints such as a general feeling of illness and body aches. The inflammation of the thyroid gland, which lasts for several months, typically runs in several phases. First, there is an overactive thyroid gland (hyperthyroidism) , followed by a brief normal thyroid function ( euthyroidism ). This turns into a phase of underactive thyroid (hypothyroidism) . During a recovery phase, the thyroid function finally normalizes again and there is usually complete healing.
The diagnosis is made clinically as part of the anamnesis , during clinical examinations and with the help of laboratory parameters. If in doubt, the diagnosis can be confirmed with the help of a tissue removal ( biopsy ). De Quervain's subacute thyroiditis is usually a self-limiting condition, meaning it heals within a year without treatment. The course of the disease and the symptoms can be alleviated through therapy with pain reliever and anti-inflammatory drugs.
A disease also named after Fritz de Quervain, which is sometimes referred to as Quervain's disease or more often as de Quervain's stenoscopic tendovaginitis , has nothing in common with subacute thyroiditis.
Synonyms
The disease is also known for short as de Quervain's thyroiditis or Quervain's thyroiditis . There are also other synonyms for the disease. The term subacute non-purulent thyroiditis is used to distinguish it from purulent or acute thyroiditis . Due to typical histological changes, the synonyms giant cell thyroiditis (occurrence of giant cells) and subacute granulomatous thyroiditis (occurrence of granulomas ) can be found. Since virus infection is being discussed as the cause, some doctors refer to the disease as viral thyroiditis .
The alternative term subacute thyroiditis (SAT) is very common . However, since a subacute course also occurs in other thyroid inflammations, especially in subacute lymphocytic thyroiditis ( silent thyroiditis and postpartum thyroiditis ), confusion may occur. In addition, the disease can also be acute, so it was suggested to avoid the term “subacute”.
distribution
De Quervain's subacute thyroiditis is the most common pain-related thyroid disease. Quervain's thyroiditis accounts for up to 5 percent of all thyroid diseases in adults. Women are 4 to 7 times more likely to be affected than men.
There are only a few extensive studies on epidemiology , especially on the frequency of the disease. According to one of the largest cohort studies , the incidence in Olmsted County , Minnesota , from 1960 to 1997 was 4.9 cases per 100,000 population per year. The age of the patients was between 14 and 87 years, the frequency peak in the 4th and 5th decades of life. Independently of this cohort study, there are isolated case reports of Quervain's thyroiditis in children whose age in these publications was between 1.7 and 10 years.
A seasonal accumulation in spring or summer was observed in some studies.
causes
The cause of de Quervain's subacute thyroiditis is unknown. It is considered likely that the inflammation is the result of a viral infection, as previous studies showed that most patients had a recent upper respiratory infection . A connection with the classic respiratory virus infections, for example by enteroviruses and Coxsackie viruses , could not be shown, however.
Furthermore, genetic predispositions for carriers of the human leukocyte antigens HLA-B35 and HLA-B67 are known. Individuals who have one of these haplotypes have a - in the case of HLA-B35 up to 50 times - increased risk of developing subacute thyroiditis de Quervain. The HLA-B35 haplotype has been demonstrated in more than half of the patients suffering from subacute thyroiditis de Quervain in several studies. A familial accumulation could so far only be proven in a few cases. A common assumption is that both a viral infection and an autoimmune reaction play a role in the development of thyroiditis, i.e. a reaction of the immune system against the body's own thyroid tissue. A molecular mimicry is assumed to be the underlying mechanism . However, the fact that de Quervain's subacute thyroiditis, unlike other autoimmune diseases, is self-limiting, speaks against this hypothesis.
Symptoms and course of the disease
The disease begins subacute. De Quervain's thyroiditis is characterized by a multi-phase course of the disease. The symptoms can vary widely and not every patient shows symptoms in every phase described here.
A prodromal stage with a general feeling of illness, difficulty swallowing , inflammation of the throat (pharyngitis), muscle and joint pain and a slight fever is typical . As a result of an inflammatory reaction of the thyroid gland, severe pain usually develops over time. These can radiate to the ear and the lower jaw, among other things. If pressure is exerted on the thyroid bed, the pain may increase. In addition, the pain on pressure can change its location as the disease progresses.
The inflammation leads to destruction of the thyroid follicles , which is accompanied by a breakdown of the thyroglobulin stored in them . The thyroid hormones triiodothyronine (T 3 ) and thyroxine (T 4 ) are released into the blood in an uncontrolled manner. The increased blood concentration of thyroid hormones inhibits the formation of thyrotropin (TSH) in the pituitary gland (pituitary gland), so that the formation of new thyroid hormones is reduced. The clinical picture of an overactive thyroid gland and in up to 50 percent of the patients a picture of a thyrotoxicosis (poisoning symptom due to the excess of thyroid hormones). Typical symptoms of hyperthyroidism are excessive sweat production , accelerated heartbeat , weight loss , nervousness and tremors .
This condition lasts until the supplies of thyroid hormones are exhausted and ultimately, after a short period of normal thyroid function, hypothyroidism occurs. If you have hypothyroidism, typical symptoms are decreased performance, lack of drive, weight gain, slow heartbeat and low blood pressure . Depending on the severity and phase of the disease, there may be overall signs of an over- or underactive thyroid, which is why the symptoms of this disease are very variable in the course.
The disease lasts for several months. As a rule, complete and spontaneous healing (self-limitation) occurs within twelve months even without the use of medication. In 5 to 15 percent of those affected, a permanent hypothyroidism persists, so that long-term therapy with thyroid hormones must take place. A recurrence ( relapse ) of subacute thyroiditis occurs in only 2 percent of cases .
histology
The histological picture of subacute thyroiditis is characterized by granulomatous inflammation and the presence of giant cells. In addition to giant cells, granulomas consist of dead cells ( cell necrosis ) and macrophages . As part of the inflammatory reaction, the follicular epithelial cells of the thyroid gland are destroyed and colloid escapes , which is phagocytosed by the giant cells . The granulomas only appear in a few places in the thyroid tissue. The remaining thyroid tissue appears intact.
diagnosis
On clinical examination, a tender thyroid gland is typical, which can be asymmetrically enlarged.
A suspected or existing enlargement of the thyroid gland can be confirmed with the help of a thyroid ultrasound scan. This shows an inhomogeneous pattern that does not occur in “healthy” thyroid tissue, in which hypoechoic and hypoechoic regions alternate. The hypoechoic regions are the foci of inflammation in the disease. They appear dark on the monitor because they reflect the sound less well than normal thyroid tissue (see examination of the thyroid gland ). The extent of the thyroid vessel supply, the vascularization, can also be shown. In de Quervain's subacute thyroiditis it is reduced to normal. This distinguishes de Quervain 's thyroiditis, for example, from Graves' disease , in which the vascularization is much more pronounced.
The diagnosis can be supported by the determination of various laboratory parameters in the blood. As a sign of the inflammatory reaction , the inflammation parameters C-reactive protein (CRP) and the sedimentation rate (ESR) are almost always significantly increased. The number of white blood cells is normal or slightly increased ( leukocytosis ). The latter is also a sign of an active inflammatory reaction. The thyroid function parameters are changed depending on the phase of the disease. In the hyperthyroid phase TSH are decreased and the thyroid hormones are increased, in the euthyroid phase the parameters are in the normal range and in the hypothyroid phase TSH are increased and the thyroid hormones are decreased. The determination of thyroid-specific antibodies plays an important role in differential diagnosis .
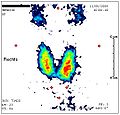
If there are any doubts about the diagnosis, a thyroid scintigraphy and sampling by fine needle aspiration with a subsequent histological examination can be used for differential diagnosis . Both procedures are not part of routine diagnostics for this clinical picture and are only required in individual cases, especially in the case of atypical courses. The iodine uptake , which can be measured quantitatively with thyroid scintigraphy, is usually greatly reduced due to the inflammation-related iodine transport disorder and the reduced TSH level. In a thyrotoxic phase in particular, iodine uptake is massively reduced (24-hour uptake of 123 iodine below 5 percent), which is helpful in differential diagnostic considerations, for example to differentiate Graves' disease . In fine needle biopsy (fine needle aspiration), thyroid tissue is removed with a thin needle (biopsy), which is then examined histologically in the pathology department .
Thyroid scintigraphy in subacute thyroiditis: decreased uptake .
Differential diagnosis
De Quervain's subacute thyroiditis is the most common cause of a painful thyroid. However, there are other conditions that can cause thyroid pain.
In terms of differential diagnosis , acute purulent thyroiditis , which is usually caused by bacteria, must be considered. As in de Quervain's subacute thyroiditis, the thyroid is tender on pressure. The lymph nodes in the neck area are enlarged and also painful. The skin over the thyroid gland is often red. The laboratory usually shows signs of severe bacterial infection or sepsis . Abscesses may be detected in thyroid ultrasound .
Like symptoms such as subacute thyroiditis causes Palpationsthyreoiditis , characterized by scanning ( palpation may develop) the thyroid, for example, prior to surgery. A slightly painful swelling of the thyroid gland can also be observed in Hashimoto's thyroiditis . However, the rate of sedimentation is not increased in this disease and the thyroid sonogram usually shows a continuously hypoechoic thyroid.
In addition, other granulomatous diseases should be considered as causes. These include tuberculosis , sarcoid and diseases from the rheumatoid group .
therapy
Therapy is usually symptomatic. Above all, pain relievers and anti-inflammatory substances from the group of non-steroidal anti-inflammatory drugs (NSAIDs) , such as acetylsalicylic acid (ASA) and ibuprofen, are used . When these drugs are insufficient to provide symptomatic treatment, glucocorticoids , primarily prednisolone , are used to reduce inflammation. If neither NSAID nor glucocorticoid therapy can bring about pain relief, the diagnosis must be questioned. If there are clear signs of hyperthyroidism such as an increase in heart rate , these can also be treated symptomatically.
The anti-thyroid drugs used for many overactive thyroid glands play no role in the treatment of subacute thyroiditis de Quervain, as there is no increased production of thyroid hormones, but only an increased release of hormones that have already been formed. Even in the mostly mild hypothyroid phase, specific therapy is only necessary in rare cases. There is an exception if the hypothyroid phase is significantly longer. In this case, the substitution of thyroid hormones is indicated. L-thyroxine preparations are mostly used for this.
Medical history
The first detailed publication on subacute granulomatous thyroiditis with a total of 18 case reports was written by Holger Mygind . In 1895 he referred to the disease as "Thyroiditis Acuta Simplex". The name commonly used today, "Subacute Thyreoiditis de Quervain", goes back to Fritz de Quervain , who histopathologically characterized the disease in 1904 and differentiated it from other thyroid infections. De Quervain's publication was based on six of his own research preparations and a literature search with a total of 57 case studies dating back to 1814. Why the disease was named after de Quervain and not after Mygind is unknown.
literature
- Alan P. Farwell: Subacute Thyroiditis. In: Lewis E. Braverman, David S. Cooper (Eds.): Werner & Ingbar's The Thyroid. A Fundamental and Clinical Text . 10th edition. Wolters Kluwer, Philadelphia 2013, ISBN 978-1-4511-2063-9 (English). Pp. 418-422.
- P. Engkakul, P. Mahachoklertwattana, P. Poomthavorn: Eponym: de Quervain thyroiditis. In: European Journal of Pediatrics. Volume 170, Number 4, April 2011, ISSN 1432-1076 , pp. 427-431, doi: 10.1007 / s00431-010-1306-4 , PMID 20886353 (review).
- R. Hörmann: Thyroid Diseases . ABW-Wissenschaftsverlag, 4th edition, 2005, ISBN 3-936072-27-2 , p. 106 ff.
- W. Böcker et al. a .: pathology . 3rd edition, Urban and Fischer Verlag, 2004, ISBN 3-437-42381-9 , p. 388 ff.
Individual evidence
- ↑ H. Schatz: On the thyroiditis de Quervain. In: DMW - German Medical Weekly. 100, 1975, pp. 2377-2380, doi: 10.1055 / s-0028-1106551 .
- ↑ a b H. Mönig, B. Harbeck: Thyreoiditis. In: DMW - German Medical Weekly. 133, 2008, doi: 10.1055 / s-2008-1046710 , p. 301.
- ↑ a b c P. Engkakul, P. Mahachoklertwattana, P. Poomthavorn: Eponym: de Quervain thyroiditis. In: European Journal of Pediatrics. Volume 170, number 4, April 2011, ISSN 1432-1076 , doi: 10.1007 / s00431-010-1306-4 , PMID 20886353 , p. 428.
- ↑ a b V. Fatourechi et al .: Clinical features and outcome of subacute thyroiditis in of incidence cohort: Olmsted County, Minnesota, study. J Clin Endocrinol Metab . May 2003; 88 (5), PMID 12727961 , p. 2100.
- ↑ a b R. Gärtner: Inflammatory thyroid diseases, pathophysiology, diagnostics and therapy . Der Internist, Volume 43, Number 5, doi: 10.1007 / s00108-002-0550-8 , p. 647
- ↑ K. Luotola et al .: Evaluation of infectious etiology in subacute thyroiditis - lack of association with coxsackievirus infection . APMIS (1998) 106 (4): pp. 500-504 PMID 9637274
- ↑ N. Ohsako et al .: Clinical characteristics of subacute thyroiditis classified according to human leukocyte antigen typing. J Clin Endocrinol Metab. 1995 Dec; 80 (12): 3653-6. PMID 8530615
- ↑ EF Zein et al .: Familial occurrence of painful subacute thyroiditis associated with human leukocyte antigen-B35. Presse Med. 2007 May; 36 (5 Pt 1): 808-9. Epub 2007 Mar 23. PMID 17383147
- ↑ a b K. D. Burman: Subacute granulomatous thyroiditis . UpToDate v15.3, August 2007
- ↑ a b A. E. Heufelder et al .: The thyroiditis: Current status of pathogenesis, diagnosis and therapy. Dtsch Arztebl 1998; 95 (9): A-466 / B-394 / C-368. Online version
- ↑ a b c d A. Bindra, GD Braunstein: Thyroiditis. In: American family physician. Volume 73, Number 10, May 2006, ISSN 0002-838X . PMID 16734054 , p. 1769
- ↑ a b c d e f g E. N. Pearce, AP Farwell, LE Braverman: Thyroiditis. In: The New England Journal of Medicine . Volume 348, Number 26, June 2003, pp. 2646-2655, ISSN 1533-4406 . doi: 10.1056 / NEJMra021194 . PMID 12826640 . (Review).
- ↑ S.-Y. Sheu, KW Schmid: Inflammatory Thyroid Diseases Epidemiology, Clinic and Morphology. Der Pathologe, Volume 24, Number 5 doi: 10.1007 / s00292-003-0628-7 , p. 343
- ↑ S.-Y. Sheu, KW Schmid: Inflammatory thyroid diseases. In: The Pathologist. 24, 2003, doi: 10.1007 / s00292-003-0628-7 , p. 344.
- ↑ a b P. Engkakul, P. Mahachoklertwattana, P. Poomthavorn: eponym: de Quervain thyroiditis. In: European Journal of Pediatrics. Volume 170, Number 4, April 2011, p. 427, ISSN 1432-1076 . doi: 10.1007 / s00431-010-1306-4 . PMID 20886353 . (Review).
- ↑ Holger Mygind: Thyroiditis Acuta Simplex. In: The Journal of Laryngology, Rhinology, and Otology. 9, 1895, pp. 181-193, doi: 10.1017 / S1755146300152771 .
- ^ F. de Quervain: The acute non-purulent thyroiditis. In: Messages from the border areas of medicine and surgery . 1904 (Suppl. 1), p. 165.
- ↑ Franz U. Steinberg: Subacute Granulomatous thyroiditis: A Review. In: Annals of Internal Medicine. 52, 1960, p. 1014, doi: 10.7326 / 0003-4819-52-5-1014 .
- ↑ Highlights of Thyreology: A Historical Vignette. In: Journal of Clinical Endocrinology and Metabolism. 2014, 7 (1), p. 24 PDF version