Blood pressure
The blood pressure is the pressure ( force per area ) of the blood in a blood vessel . It is directly dependent on the cardiac output and the vascular resistance . It is largest in the aorta and continues to decrease as the blood moves through the bloodstream via arteries , capillaries and veins until it reaches the heart again. Usually, “blood pressure” refers to the pressure in the larger arteries. In a healthy body, blood pressure regulates itself . Elevated blood pressure has a negative effect on health and life expectancy, but is often not perceived subjectively. Blood pressure should therefore be measured from time to time. The blood pressure is usually given in mmHg (millimeters of mercury); within the EU this is also the legal unit of measurement.
General
Different pressure conditions prevail in different areas of the bloodstream . If one speaks of blood pressure without further addition, then one usually means the arterial pressure in the major arteries at heart level ( BD or BP , the Synekdoche RR for Riva-Rocci is also common ), which is usually measured on the brachial artery of the upper arm. Central venous pressure is also of medical interest.
The blood pressure readings are overpressures compared to the atmosphere and are usually not given in the correct SI unit Pascal (Pa) , but in the traditional unit mmHg (millimeter of mercury), because mercury manometers were previously used to measure pressure .
The arterial pressure is conventionally given as a pair of numbers consisting of systolic (maximum value, depends, among other things, on cardiac output) and diastolic pressure (minimum value, in the heart filling phase and therefore also dependent on the elasticity and the filling status of the large vessels). With a blood pressure of, for example, 105 mmHg during systole and 70 mmHg in diastole, one then says “105 to 70” , written “105/70 mmHg” .
Under normal conditions and without taking individual deviations into account, the blood pressure in adults is around 120/80 mmHg. At rest, the normal systolic arterial pressure is 13.3-17.4 kPa (100-130 mmHg) and the diastolic value is 8.0-11.3 kPa (60-85 mmHg). In addition, the mean arterial pressure and the pulse amplitude (difference between systolic and diastolic arterial pressure value) are important. The mean blood pressure values correspond to those when lying down. When sitting and standing, the blood pressure is higher due to gravity in the lower half of the body than when lying down, while it is lower above the hydrostatic indifference level than when lying down.
From 140/90 mmHg (previously from 160/95 mmHg) one speaks internationally as high blood pressure (arterial hypertension), which has a negative effect on health and life expectancy . This value is also recommended in the joint guidelines of the European societies for hypertension and cardiology in the 2013 version as the maximum value for almost all patients. High blood pressure, which can sometimes run for a long time without symptoms, is a risk factor for arteriosclerosis and cardiovascular diseases - especially heart attacks and strokes . With systolic values below 100 or 90, however, one speaks of blood pressure (arterial hypotension). However, low blood pressure usually only requires treatment if it is accompanied by symptomatic complaints for the person concerned.
The blood pressure of a one-year-old person is usually around 80-105 / 55-70, a newborn has values of 65–85 / 35–45 mmHg, premature babies have values of 55–75 / 35–45, children between the ages of six and twelve have values of 95– 110 / 60-75 mmHg. After the age of twelve, blood pressure values of 110–135 / 65–85 are normal.
Physiology of arterial pressure
For the sake of simplification, it is not the instantaneous value of the arterial blood pressure, which fluctuates in the frequency of the heartbeat , but the mean arterial pressure that should be considered. The difference between mean arterial blood pressure and central venous pressure is also known as the arteriovenous pressure difference; it is the drive for the blood flow through the body's circulation , just as the electrical voltage is the drive for the current . The current intensity in the blood circulation corresponds to the volume pumped by the heart per unit of time , which is referred to as cardiac output . Finally, there is also a resistance to blood flow, the total peripheral resistance . There is a relationship between these variables that corresponds to Ohm's law :
The equation also applies in principle if, instead of the cardiac output (as mean volume flow), instantaneous values of the blood flow are used. The periodic fluctuation of the arterial blood pressure around the mean pressure is explained by the inconstant blood ejection of the heart : The systolic blood pressure results from the blood flow that the heart generates during the expulsion phase. The arteries near the heart are of the elastic type ; they are stretched during systole and thus remove volume from the bloodstream, which means that the systolic pressure is lower. Driven by the wall tension, the temporarily stored blood is released again during the diastole ( Windkessel effect ), which results in the diastolic blood pressure . The extensibility is quantified by the size compliance (change in volume per change in pressure).
The parameters of arterial pressure are accordingly the systolic pressure (maximum pressure), the diastolic pressure (minimum pressure) and the pulse pressure (difference between systolic / diastolic pressure). They are influenced as follows:
- A decrease in compliance (as occurs as arteriosclerosis in almost every aging person) increases the pulse pressure: the systolic pressure increases, the diastolic pressure decreases, the mean arterial pressure remains unchanged ( ceteris paribus ).
- Systolic pressure, diastolic pressure and pulse pressure are proportional to the cardiac output, so when the pressure increases, the systolic pressure rises faster than the diastolic. The increase in cardiac output during dynamic physical work is accompanied by a decrease in peripheral resistance, so that under these circumstances an isolated increase in systolic pressure can be observed.
- An increase in the peripheral resistance increases the systolic and diastolic blood pressure by approximately the same amount, so the pulse pressure ideally remains unchanged. If a decrease in cardiac output occurs at the same time, an isolated increase in diastolic blood pressure can result; an example of this is the regulation of the circulatory system when it is cold.
Measurement of arterial pressure
A distinction is made between direct (invasive, bloody) arterial pressure measurement using a pressure sensor in a blood vessel and indirect (non-invasive, bloodless) measurement, which is carried out on an extremity using a blood pressure cuff .
The direct arterial pressure measurement is mainly used by anesthetists for monitoring during an operation and in intensive care units.
Indirect arterial pressure measurement is now the method of choice in most medical fields because it can be carried out quickly and safely. A distinction is made between manual measurement and automatic measurement using a digital device (see blood pressure monitor ). The manual measurement can be performed using auscultation , palpation or oscillation.
Systolic
The work of the heart is a wave-like pumping process: every time the left ventricle contracts, the blood is suddenly pumped into the main artery (aorta), which causes the blood pressure in the vessels to rise briefly. The maximum pressure reached is called the upper blood pressure value or systolic blood pressure ("systole" = medical term for the phase of the pumping process in which the heart contracts and ejects blood. Systole (Greek) = the contraction).
Diastolic
After the left ventricle has contracted during the pumping process, the ventricle must first be filled with blood for the next pump stroke. In return, the chamber relaxes. During this relaxation phase, in which no more blood is pumped into the main artery, the pressure in the blood vessels slowly drops (until the next burst of blood comes from the heart). The lowest pressure reached is called the lower value or diastolic blood pressure (from ancient Greek διαστολή diastolḗ “expansion”). With a blood pressure of 120 to 80 mmHg, the pressure pulsates continuously back and forth between 120 and 80 mmHg.
meaning
The arterial pressure is not a fixed value and fluctuates depending on the activity being carried out. It increases with physical exertion, stress and excitement, and decreases during physical and mental rest phases. Normally, blood pressure drops by 10–20% at night ( dipping ).
If, on the other hand, a person suffers from arterial hypertension (high blood pressure), the pressure in the blood vessels remains high even at rest: the heart has to constantly pump with increased effort. This puts a strain on the heart and blood vessels. Arterial high pressure is present if a value of over 140/90 mmHg is reached after repeated measurements.
High blood pressure is recognized as a risk factor for developing cardiovascular disease . If overweight or obesity (severe overweight) as well as another risk factor, such as diabetes , smoking or lipid metabolism disorders ( high cholesterol or LDL), are added to the risk factor, there is a significantly increased risk of heart disease over the course of life. Suffering from circulatory disease . One speaks therefore also of the cardiometabolic risk factors.
An increased intake of phosphate through food also plays a role. In test subjects, an additional daily dose of sodium phosphate increased the blood pressure by an average of 4.1 or 3.2 millimeters of mercury. Two months after weaning, the values returned to normal.
Classification of high blood pressure values according to WHO / ISH
The World Health Organization (WHO) published in 1999 together with the International Society of Hypertension (ISH) the revised 2003 WHO / ISH Hypertension guidelines ( German WHO / ISH Hypertension Guidelines ) adults with the following classification for people.
| systolic (mmHg) | diastolic (mmHg) | ||
|---|---|---|---|
| Grade 1 hypertension | 140-159 | or | 90-99 |
| Grade 2 hypertension | 160-179 | or | 100-109 |
| Grade 3 hypertension | ≥ 180 | or | ≥ 110 |
European guidelines of the ESH / ESC
In 2013 the new guidelines for the management of arterial hypertension ( ISBN 978-3-89862-948-5 ) European Society of Hypertension (ESH) / European Society of Cardiology (ESC) were published, which are also published by the German Society for Cardiology and the German Hypertension League e. V. are supported. In terms of content, the classifications coincide with the above. of the WHO (as of 11/2015). There was a change in starting medication , among other recommendations . This should only begin with hypertension grade 1 and not, as before, with values in the highly normal range.
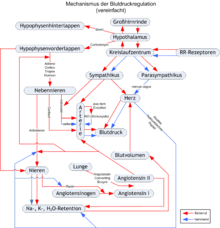
Arterial pressure regulation
The arterial pressure must move within certain ranges, because both too high and too low arterial pressure damage the organism or individual organs . At the same time, however, the arterial pressure must also be adjusted in the event of changing loads (e.g. a strenuous endurance run or rest, sleep). The blood pressure will
- short-term about vessel size and cardiac activity (→ main article: blood circulation ) and
- regulated in the long term via the blood volume (→ main article: volume balance ) .
The basic requirement for any arterial pressure regulation is that the body can measure the arterial pressure in the vessels itself. In the aorta, carotid arteries and other large arteries in the chest and neck, pressure-sensitive sensory cells, the baroreceptors , measure the expansion of the arterial wall.
Short-term arterial pressure regulation
The mechanisms of short-term arterial pressure regulation take effect within seconds. The most important mechanism is the baroreceptor reflex . Expands a higher pressure the artery wall, the baroreceptors transmit in higher-frequency pulses to the circulation center in the medulla , which then the sympathetic innervation of the heart ( cardiac output ) and vessels ( peripheral resistance ) inhibits, whereby the blood pressure is lowered and the control loop thus adversely is closed with feedback .
Conversely, reduced arterial pressure leads to reduced irritation of the baroreceptors and thus to stimulation of the sympathetic nervous system in the medulla oblongata. By decreasing the inhibition, the volume of blood ejected by the heart is increased; in addition, there may be a constriction of the vessels in the body's circulation, which increases the blood pressure again. In the right and left atrium there are stretch receptors that react in a similar way.
Medium-term arterial pressure regulation
The renin-angiotensin-aldosterone system should be mentioned here in particular . If the kidney blood flow decreases (e.g. due to a generalized drop in arterial pressure or a narrowing of the renal arteries), this leads to increased renin release in the kidneys and thus ultimately to an increase in the concentration of angiotensin II , which has an immediate vasoconstricting effect and in the long term increases the blood volume , which over the Frank-Starling mechanism also increases arterial blood pressure. The release of renin is also increased by the sympathetic nervous system, the activity of which depends on the signals from the above-mentioned receptors (especially those from the low-pressure system).
Long-term arterial pressure regulation
The kidneys are particularly involved in regulating the blood volume and thus the blood pressure. The main control circuit is the renin-angiotensin-aldosterone system , whose volume-increasing effects are not only caused by angiotensin II, but also by aldosterone . Both increase the reabsorption of sodium and (indirectly) water in the kidneys. Some authors also call the pressure diuresis , whereby the fluid excretion is said to increase directly through increased kidney blood flow.
When the blood volume puts increased pressure on the atria, hormones such as ANP are released there, which increase the excretion of fluid in the kidney.
Organ-specific pressure regulation
To ensure an even blood supply, some organs are able to react directly to fluctuations in blood pressure. This mechanism is known as the Bayliss effect or myogenic autoregulation , as the vascular muscles themselves take over the regulation.
pathology
- High arterial pressure see arterial hypertension , pulmonary hypertension , portal hypertension .
- Too low blood pressure see hypotension .
- For high venous blood pressure, see venous hypertension (peripheral) and central venous blood pressure .
Static blood pressure
Static blood pressure is understood to mean a pressure of approx. 6 to 7 mmHg, which is established in the vessels when the heart stops lying down. The static blood pressure enables a statement to be made about the filling status of the vessels. It depends on the blood volume and the vascular capacity.
Individual evidence
- ↑ Christoff Zalpour (Ed.): Anatomy and Physiology (For Physiotherapy). 3rd edition, 2010, p. 431.
- ↑ Directive 80/181 / EEC
- ↑ Susanne Hahn: Blood Pressure. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 193.
- ↑ Vera Zylka-Menhorn: Arterial Hypertension: Greater flexibility in therapy, greater involvement of the patient . In: Deutsches Ärzteblatt 2013; 110 (26): A-1316 / B-1152 / C-1139. June 28, 2013. Retrieved June 28, 2013.
- ↑ J. Kaufmann, M. Laschat, F. Wappler: Preclinical care of child emergencies. In: Anaesthesiology & Intensive Care Medicine. Volume 61, 2020, pp. 26–37, here: p. 29.
- ↑ a b German Heart Foundation
- ↑ Increased phosphate intake increases blood pressure in healthy adults. In: unibas.ch . August 23, 2018, accessed March 30, 2019 .
- ↑ Jaber Mohammad, Roberto Scanni, Lukas Bestmann, Henry N. Hulter, Reto Krapf: A Controlled Increase in Dietary Phosphate Elevates BP in Healthy Human Subjects. In: Journal of the American Society of Nephrology. 29, 2018, p. 2089, doi : 10.1681 / ASN.2017121254 .
- ↑ WHO / ISH Hypertension guidelines
- ↑ Guidelines for the Management of Arterial Hypertension