triage
Triage ([ triːˈɑːʒ ]), from French trier , “sort”, “select”, “read out” (German term also sifting or classifying ), describes a procedure that is not legally codified or methodically specified for the prioritization of medical assistance , especially in the case of unexpectedly high volumes Patient and objectively insufficient resources. In this case, the postponed or waiting medical help is inevitable. Without a structured triage (classification) there is a risk of politically or ideologically motivated unethical selection.
Triage is a term derived from military medicine for the - ethically difficult - task of deciding how to divide up the scarce human and material resources , for example in the event of a mass casualty or otherwise sick . It is a stratification procedure prior to a full diagnosis . Theoretical models that address the distribution of scarce resources are also grouped under the term allocation .
Structured triage instruments are also used in emergency rooms and are also referred to as initial assessments there .
history

At the beginning of the 16th century, Emperor Maximilian I (1459–1519) introduced his Army Sanitary Constitution , which for the first time documented orderly medical units whose task, among other things, consisted of rescuing and treating wounded survivors. Detailed information on the classification of the various degrees of severity of wounds can be found for the first time in the Royal Prussian Field Hospital Regulations of 1787.
A rethink in the military medical system required the extensive campaigns of the French revolutionary armies during the coalition wars of 1792-1815. The result was new approaches to medical care on site and transport to treatment facilities further away. The French doctor Dominique Jean Larrey achieved successes with his rapid classification methods for amputations (75-80% of those who operated on him survived, a significantly higher rate than with other doctors), but was not yet able to incorporate them into a formal procedure that could also be used by other doctors implement.
It was not until the Russian surgeon Nikolai Ivanovich Pirogov (1810–1881) developed graduated surgical treatment methods and the principle of "spreading the sick" (distributed treatment of the injured and sick) to order the overcrowded dressing stations with classifications of the wounded from his experience in the Caucasian War and the Crimean War in five stages ( Pirogov's principle of sighting ). The Prussian army adopted the Russian principle in 1866, later it was also applied to the other medical services of allied armies in Europe. In the further development, numerous advances in medicine and surgical methods were also transferred to the organization of the military medical service. However, the Pirogow principle of "dispersing the sick" remained in place during the First World War .
When a ship went down , the rule “ women and children first! “(So-called Birkenhead Drill from 1852) or“ The captain is always the last to disembark ”. Rules of thumb also applied, such as in war: "Provide our soldiers before civilians, these from enemy soldiers!" Attempts have also been made to avoid the decision-making problems by applying the order in which the injured person was noticed or whoever was known to be rescued first.
The French medical service introduced the principle of "triage - transport - traitement" (French for selection - transport - treatment) and thus coined the term triage . The French doctors Spire and Lombardy defined triage in 1934 as
- the diagnosis of the present injury and
- the assessment of the urgency of the intervention ( categorization ) and
- the assessment of the degree of fitness for transport and
- the destination of the wounded man.
The medical services of the German Reichswehr and later the Wehrmacht basically stuck to the experience of "dispersing the sick" from the First World War, but could hardly train their doctors sufficiently in effective use due to the rapid rearmament. It was not until 1942 that a structured procedure for triage in the German military medical service was laid down in the guidelines for the care of the wounded in the front medical facilities , which also included the military situation and transport options.
With the establishment of NATO , a uniform system of "classification categories " was created, which was established in the member states and beyond. War with the current threat from powerful conventional, but also from nuclear, biological and chemical weapons influenced the further development of the systematization of injuries among soldiers.
These procedural principles were also used in the provision of assistance in civil disasters, beginning with the planning for coping with radiation damage , which z. B. occur in accidents in the context of the use of nuclear energy . The sighting system is also used in civil mass casualties , e.g. B. in terrorist attacks .
The STaRT scheme ( Simple Triage and Rapid Treatment ), which was developed by the Hoag Hospital and Newport Beach Fire Department ( Newport Beach , California / USA) in the early 1980s, pioneered the modern ambulance service .
In March 2020, the term and the procedure in connection with the spread of the COVID-19 pandemic gained new, global relevance; in Europe initially with the development in Italy , shortly afterwards also in Spain, Alsace , Germany and the USA.
The procedure is standard in modern hospital and patient management, e.g. B. in acute patient distribution or emergency rooms .
Necessity and problems of triage
Triage can be triggered by mass casualties in major accidents, as well as catastrophes , pandemics and wars . Only a limited number of doctors and paramedics then have to care for numerous life-threatening, seriously and slightly injured people.
Overall, triage can be an extremely difficult task when making decisions that are likely to result in the death of some. Feelings of guilt or post-traumatic stress disorders often occur among those involved, especially among decision-makers.
The rules for triage in the event of mass casualties, which are generally communicated in training today, are aimed at ensuring that as many people as possible survive the event with as little damage as possible. In this way one tries to achieve the best possible result for the collective of injured parties, whereby the interests of the individual have to take second place. If nobody is disadvantaged, there is no triage.
Intensive care measures for a few seriously injured people may tie up capacities that could be used to care for many less injured people. Therefore, those whose situation seems hopeless from the outset will be treated with pain relievers rather than intensive care until others whose prognosis is more favorable on site are treated. This temporary abandonment of the principle of equality in individual medicine, which is established in the health system of a modern society, as well as any lasting division into treatment priorities or viewing categories is an ethically difficult task and challenge. In order to avoid the ethically questionable prioritization, viewing schemes were developed to help decision-makers, which, based on medical assumptions, facilitate the most appropriate procedure possible.
The triage process
Salvage sighting
The rescue inspection (also pre-triage or precautionary inspection ) is used in the immediate damage area and is intended to provide a quick overview of the patients to be treated. The rescue sighting is carried out by the helpers who arrive first, the so-called "classifiers". A decision has to be made as to which victim is to be rescued first, who must be taken immediate medical measures and who must wait first. An examination time of 20–60 seconds per patient is a guideline. This decision serves to instruct the following helpers and as a point of reference for the technical rescue, which is then carried out in the order determined.
Initial measures are delegated to bystanders or slightly injured persons. After the patient has been categorized and marked, the classifier immediately moves on to the next patient. Complex documentation should be avoided. All that is required is a tally sheet or a sketch of the location. The inspection result is marked on the patient, with color coding or identification with abbreviations or numbers being attached to the patient.
Treatment viewing
The rescue sighting described serves as an initial overview in the immediate damage area. As the time elapses after the triggering event, a treatment structure can be created that enables a more differentiated examination. But here, too, the specific allocation to certain treatment options is important in order to enable care as required and to be able to allocate helpers and equipment. The treatment inspection preferably takes place on an established treatment station .
An experienced helper, usually an emergency doctor specially trained for the inspection , determines the treatment priorities according to emergency medical criteria and with regard to the available options. He is supported as far as possible by helpers who help him with the preparation, such as undressing the patient and identifying the injured person with the help of the injured person's card. The inspection will be repeated in accordance with the transport and treatment capacities that may have changed over time due to the arrival of further rescue workers and adapted to the updated options.
Transport inspection
The aim of the transport inspection is to assess the transport stability of the patient in order to be able to transport him to a suitable hospital with a suitable rescue equipment .
Sighting schemes
overview
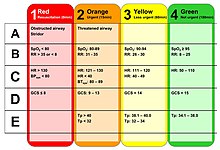
The system used in the civilian sector in German-speaking countries in the event of a major loss (e.g. a bus accident) has four levels: The victims receive attachment cards that are color-coded according to the sighting.
| category | Patient condition | consequence | colour |
|---|---|---|---|
| I. | acute, vital threat | Immediate treatment | red |
| II * | seriously injured / ill | Deferred urgency, surveillance | yellow |
| III | slightly injured / ill | later (possibly outpatient) treatment | green |
| IV | no chance of survival, dying | Caring (waiting) treatment, terminal care | blue |
| Ex | dead | Labelling | black |
| * Additional labeling: a = high transport priority, b = low transport priority | |||
In Austria and Switzerland , orange cards, which are hung around the patient in the event of a mass casualty for unambiguous identification and to support the care, are referred to as the patient guidance system (PLS), in Germany as the injured person attachment card . Electronic systems have also existed since 2011.
STaRT scheme: "Simple Triage and Rapid Treatment"
The ability to walk, respiration (breathing), perfusion (blood circulation) and the mental status according to the STaRT system are tested without special aids:
- First, all ambulatory patients are asked to go to a collection point. The patients who can save themselves from the danger zone ("walking wounded", English for "ambulatory injured"), are divided into the sighting category T3 ("MINOR"). Some of these, which the helper considers suitable, will be instructed to help in the further course.
- A patient with respiratory arrest, even after the airway has been cleared, is considered to have died ("DECEASED").
- Checking the respiration (breathing): A breathing rate above 30 / min. is assessed as urgent, the patient is assigned to the assessment category T1 ("IMMEDIATE").
- Checking the perfusion (blood flow): In the event of heavy bleeding, an assistant will be instructed to stop the bleeding ( pressure bandage ). The capillarization time is measured with the nail bed sample. If it is more than 2 seconds, this is an indication of insufficient blood flow ( blood pressure <90 mm Hg), the patient is classified in the viewing category T1 ("IMMEDIATE").
- Checking the mental status: In the event of unconsciousness or an inadequate reaction when spoken to, the patient is assigned to the viewing category T1 ("IMMEDIATE").
- All other patients are in the killed or seriously injured divided T2 ( "DELAYED").
The rescue from the danger area then takes place in the following order
- T3 / MINOR (since they can go away themselves)
- T1 / IMMEDIATE
- T2 / DELAYED
- DEAD / DECEASED
This structured approach should take a maximum of 60 seconds per patient and still enable a comprehensive and relatively precise evaluation. The STaRT scheme is suitable for use by trained rescue workers and medical personnel of all skill levels. Since it is designed for adults, it ignores special features in children.
JumpSTaRT: START for children
A child who has stopped breathing, unlike an adult, is more likely to have a problem with obstructed airways (rather than injury-related disorders). A breathing rate of over 30 / min is still normal in children. The blood flow in children is very difficult to assess using the fingernail sample, because children cool down very easily and the capillary blood flow is then no longer meaningful. In addition, a delayed or inadequate reaction to being spoken to can be assumed in children, especially from small children or in dangerous situations, reliable answers can hardly be expected.
Therefore, the STaRT scheme for one to eight year old children at Miami Children's Hospital was modified in collaboration with the Miami-Dade Fire Rescue Department ( USA ) as follows:
- Children are only classified as deceased when they neither breathe nor have a pulse ("DECEASED").
- Children who have stopped breathing but have a palpable pulse are ventilated for 15 seconds (approx. 5 ventilations). Only when the respiratory arrest persists is the child classified as deceased ("DECEASED").
- If the respiratory rate is less than 15 / min or higher than 40 / min, the child is classified in the viewing category T1 ("IMMEDIATE").
- The palpability of a peripheral pulse (wrist, foot) is rated as a benchmark for blood circulation. If this cannot be felt while breathing, then the child is classified in the viewing category T1 ("IMMEDIATE").
- The mental status is not only checked by speaking, but also by responding to a pain stimulus in case of doubt. If the child does not respond appropriately, it is classified in the viewing category T1 ("IMMEDIATE").
mSTaRT: modified START
The modified STaRT scheme combines the findings from the JumpSTaRT and the original STaRT scheme into a comprehensive process that is suitable for both adults and children.
In Germany, it was adapted for German rating categories in 2004 by the Munich fire brigade in cooperation with the Ludwig Maximilians University in Munich and presented at a congress. A corresponding service instruction "Operational standard mass casualty - sighting" has been in force since 2005 for the rescue service of all organizations in the entire rescue service area of Munich (state capital and district of Munich). The professional fire brigade Munich trains its paramedics and emergency paramedics accordingly and ensures that it is spread in and around Munich. This concept was disseminated by the Bavarian aid organizations as part of the preparations for the 2006 World Cup .
BASIC scheme: bleeding, respiratory tract, shock, immobilization according to the classification
The New England Council for Emergency Medical Service (NECEMS) introduced the BASIC ( Bleeding, Airway, Shock, Immobilization after Classification ) scheme for the US states of Vermont , Maine , New Hampshire and Rhode Island in the 1980s .
It follows the sequence given in the acronym BASIC for checking vital functions and immediate initial measures:
- Bleeding: in the event of uncontrolled bleeding, a helper will be instructed to stop the bleeding by applying pressure. The patient is divided into the viewing category T1.
- Airway: the airways of an unconscious patient are checked and kept open by a helper. The patient is divided into the viewing category T1.
- Shock (shock): A patient in a volume deficiency shock is in the killed or seriously injured divided T1 and supported by a helper in the shock position.
- All other patients are classified as T2 and T3 depending on their condition.
- Immobilization after classification: If all patients have been classified, they are immobilized in the order T1, T2, T3 (cervical splints, whole-body splints).
The advantage of this scheme is that it is easy to remember even for inexperienced users - the order of the examination is already included in the acronym. It can be used very quickly, the time required per patient is between 10 and 30 seconds to recognize the respective condition. The disadvantage is that it does not offer a differentiated approach, does not make any more complex specifications and thus leaves a lot to the instinct of the helper. It is assumed that the minor injuries cannot be classified too incorrectly. It is therefore particularly suitable for inexperienced first aiders or non-medical rescue workers who are present in the very first phase of help and have to make do with simple means. The structure created in this way must then be further refined by trained rescue workers, who then use more suitable procedures (and can orientate themselves, for example, on the STaRT scheme).
Reverse triage
The concept of reverse triage (reverse viewing) follows the principle that the uninjured or slightly injured affected persons are first transported away or channeled through the decontamination / treatment stations. The logic behind this is that
- these patients then no longer hinder the treatment of the seriously injured on site;
- these patients should anyway be moved to treatment facilities further away so as not to block the closer ones for the seriously injured;
- those patients have already been saved who have the highest chance of survival and / or
- These patients are easiest to get out of the danger zone, especially in accidents involving dangerous goods (or in other dangerous zones, such as under fire in war or assassinations) and are then no longer at risk.
Triage and initial assessment in the emergency room
In addition to a disaster, structured triage instruments are also used in regular medicine in emergency rooms , and in mobile emergency medicine they are also referred to as initial assessments. Although the initial assessment could actually be viewed as a special case of triage, it differs from it in one essential point: In the out-of-hospital area, it is important to use the locally or temporally limited resources as efficiently as possible, i. H. to achieve the goal of as many survivors as possible. In the clinical area, however, the basic assumption is that sufficient resources are available to optimally treat all patients. This means that there is no conflict between individual and overall benefit.
In the international literature, five-level triage systems are named as valid and reliable instruments to identify patients in the emergency room who have a life-threatening or urgent illness. The Rapid Acute Physiology Score (RAPS) classification system presented by Rhee and co-workers in 1987 was also considered suitable for triage (this scoring system , originally used in the rescue service to assess helicopter transports and injured children, evaluates heart rate, mean arterial pressure, respiratory rate and GCS with 0 to 4 points). The Manchester Triage System and the Emergency Severity Index have so far been used successfully in German-speaking emergency rooms . Due to the structured approach, it can be expected that seriously ill emergency patients will be recognized promptly and receive the necessary diagnostics and therapy immediately.
For triage, a separation of clinical care from decision-making is recommended in the event of a pandemic. This separation is intended to reduce the moral burden on the treating physicians, for example when patients are excluded from necessary medical treatment or when the decision is made in favor of palliative care for the terminally ill .
Decon sighting
The decontamination (detoxification) of those affected requires a special form of rescue sighting. An early identification of the hazardous substance is necessary so that efficient decontamination and appropriate medical treatment can be carried out. In addition to the classification into one of the viewing categories, the status "lying down" or "walking" (able to walk) is explicitly specified. The allocation to the decontamination area depends on this. For the decontamination itself, the following classifications are essential:
| Injury spectrum | Necessary measures |
|---|---|
| ambulatory, contaminated, but not visibly injured, or does not require assistance with decontamination | Personal decontamination, panic prevention, if necessary targeted removal |
| ambulatory, contaminated and injured, or in need of assistance with decontamination | If necessary, spot decontamination and emergency care, decontamination of the injured, if necessary transport for further treatment |
| lying down, contaminated and injured | Rescue, possibly spot decontamination and emergency first aid, decontamination of injured persons, transport for further treatment |
Even victims whose treatment is urgent may only be released for further treatment at the treatment center that is being formed or for transport to the hospital only after full body decontamination, in order to protect these areas from the spread of contamination.
See also
- Civil protection , fast-Group , Organizational leader emergency service , local helpers
- Disaster sociology
- Triage - 2009 drama film with Colin Farrell, Paz Vega and Christopher Lee
- Heinz Rudolf Kunze : We are now in the triage room , text from 1984, accessed on August 23, 2020
literature
- Bettina Schöne-Seifert : Who should you let die? (FAZ.net March 31, 2020)
- Disaster Medicine - Guide to Disaster Medical Care . (PDF) Protection Commission at the Federal Ministry of the Interior, Federal Office for Civil Protection and Disaster Aid , Bonn 2010, ISBN 978-3-939347-25-5 .
- Michael Christ et al: Triage in the emergency room , in: Deutsches Ärzteblatt Int 2010; 107 (50): 892-8; DOI: 10.3238 / arztebl.2010.0892 ( online )
- Nils Ellebrecht: Triage. Characteristics and presence of a process that creates order. In: Sociologia Internationalis. 47/2, 2009 pp. 229-257.
- Alexander Brech: Triage and law: patient selection in the event of a mass attack of those in need of help in disaster medicine. A contribution to the equity debate in the healthcare sector. Duncker & Humblot 2008, ISBN 978-3428126460 (doctoral thesis, University of Leipzig)
- Kevin Mackway-Jones, Janet Marsden, Jill Windle (Eds.): Emergency Triage: Manchester Triage Group . 3rd edition 2013, ISBN 9781118299067 . German translation of the 1st edition: First assessment in the emergency room. The Manchester Triage System . Huber, Bern 2006, ISBN 3-456-84317-8 (edited by Jörg Krey and Heinzpeter Moecke).
- Wolfgang U. Eckart : Triage. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1419 f.
- Udo B. Crespin, Gisela Neff (Hrsg.): Handbook of sighting . Stumpf & Kossendey-Verlag, Edewecht 2000, ISBN 3-932750-20-9 .
- Johanna Bleker : From “large-scale sorting business” to “triage”. The problem of sighting sick people in war. In: Johanna Bleker, Heinz-Peter Schmiedebach (ed.): Medicine and War. Frankfurt am Main 1987, pp. 211-231.
- R. Kirchhoff (Ed.): Triage in the event of a disaster . primed-Fachbuch-Verlag, Erlangen 1984, ISBN 3-88429-115-7 .
- T. Duke: New WHO guidelines on emergency triage assessment and treatment. In: Lancet. Volume 387, 2016, pp. 721-724.
Web links
- Disaster medicine: compulsion to select . In: Deutsches Ärzteblatt , August 13, 2004
- German Society for Disaster Medicine V. (DGKM e.V.)
- UF Lang: Oktoberfest Triage Evaluation Study 1998 - Prospective observational study on the quality of sighting of emergency patients from a disaster medicine perspective. (PDF; 367 kB) Passau 2002 (dissertation on the acquisition of a doctorate in medicine).
- eTriage - EU project WISECOM
- Till Zimmermann : Who will die first? , Legal Tribune Online , Wolters Kluwer Germany (on the legal situation in Germany, 2020)
Individual evidence
- ↑ Timo Blöß, Disaster Medicine : Compulsion for Selection , Deutsches Arzteblatt 2004; 101 p. 33, A-2216 / B-1854 / C-1786 (PDF). Retrieved May 7, 2017.
- ^ Sergio Stocker: Triage in Swiss children's emergency wards . (PDF) In: Paediatrika , Volume 17, No. 1, 2006, pp. 35–37; accessed on May 8, 2017.
- ↑ Counter Terrorism - When simulating a bomb attack. Retrieved on March 21, 2020 (German).
- ^ Corona triage. In: Verfassungsblog. Retrieved March 21, 2020 .
- ↑ FAZ.net March 26, 2020: "Anyone who is over 75 years old is no longer intubated"
- ↑ Jan Petter, DER SPIEGEL: Corona risk on Sylt: "Unfortunately there are guests who refuse to leave" - DER SPIEGEL - travel. Retrieved March 21, 2020 .
- ↑ Julia Merlot, DER SPIEGEL: Head of the Robert Koch Institute: "We assume that it will be a stress test for our country" - DER SPIEGEL - Wissenschaft. Retrieved March 21, 2020 .
- ↑ Hospitals in Germany - "We are driving towards the wall at full throttle". Retrieved on March 21, 2020 (German).
- ↑ Testing, Triage and Tragedy: The Trump Pandemic (March 26, 2020)
- ^ Badische Zeitung: Helios-Klinik Müllheim sets up tents to protect patients and employees - Müllheim - Badische Zeitung. Retrieved March 21, 2020 .
- ^ Badische Zeitung: Stress and lack of beds: A shift in the Loerrach emergency room - Loerrach - Badische Zeitung. Retrieved March 21, 2020 .
- ^ Triage in NATO and the federal government , Consensus Conference of the BMI. Retrieved May 13, 2017.
- ↑ The patient guidance system (PLS) . ( Memento from December 8th, 2015 in the Internet Archive ) Viennese professional rescue; Retrieved December 4, 2015
- ↑ Guidelines for the patient guidance system in rescue services (PLS) . ( Memento of December 8, 2015 in the Internet Archive ) (PDF) Interverband für Rettungswesen; Retrieved December 5, 2015
- ↑ a b M. Christ, F. Grossmann, D. Winter, R. Bingisser, E. Platz: Triage in the emergency room: Modern, evidence-based initial assessment of the urgency of treatment . In: Dtsch Arztebl Int. , 2010 Dec, 107 (50), pp. 892-898. PMID 21246025
- ↑ Walied Abdulla: Interdisciplinary Intensive Care Medicine. Urban & Fischer, Munich a. a. 1999, ISBN 3-437-41410-0 , p. 468.
- ↑ Max M. Feinstein, Joshua D. Niforatos, Insoo Hyun et al .: Considerations for ventilator triage during the COVID-19 pandemic The Lancet Respiratory Medicine, April 2020
- ↑ Swiss Academy of Medical Sciences: COVID-19 pandemic: triage for intensive-care treatment under resource scarcity Swiss Medical Weekly, March 2020
- ↑ Framework for the decontamination of injured people. (PDF) Federal Office for Civil Protection and Disaster Assistance, September 2006.
- ↑ Table of Contents