Warthin tumor
| Classification according to ICD-10 | |
|---|---|
| D11 | Benign neoplasm of the parotid gland |
| ICD-10 online (WHO version 2019) | |
| Classification according to ICD-O-3 | |
|---|---|
| 8561/0 | Warthin tumor |
| ICD-O-3 first revision online | |
The Warthin tumor ( Aldred Scott Warthin , American pathologist, Ann Arbor, 1866-1931) is a benign neoplasm or tumor-like lesion that manifests itself almost exclusively in the area of the parotid gland , rarely in neighboring cervical lymph nodes or other locations. After pleomorphic adenoma , Warthin's tumor is the second most common benign salivary gland tumor.
Clinically, the tumor is characterized by slow growth; a malignant degeneration is observed in a few individual cases. A recurrence after surgical removal is rare.
Synonyms
Terms such as adenolymphoma , cystadenolymphoma , papillary cystadenoma lymphomatosum , cystadenoma lymphomatosum papilliferum or cystadenolymphoma papilliferum are sometimes used synonymously . In order to avoid confusion with malignant lymphoma or lymphadenoma , however, it is recommended to use the term Warthin tumor . The terms Albrecht-Arzt-Tumor or Albrecht-Arzt-Warthin-Tumor have only historical significance .
history
The Warthin tumor was first mentioned in 1895 by the German surgeon Otto Hildebrand (1858–1927) under the name adenolymphoma . After Heinrich Albrecht and Leopold Arzt described the entity more precisely around 1910, Warthin used the term in 1929 as papillary cystadenoma lymphomatosum. into American literature.
Epidemiology
The age peak of the Warthin tumor is in the 6th – 7th grade. Decade of life, whereby the mean age of onset is given as 62 years. A manifestation in childhood is possible, but the tumor rarely occurs before the age of 40. The historically clear preference of the tumor for the male sex, which was given as 10: 1 in 1953, has presumably shifted to the disadvantage of the female sex, presumably due to changed lifestyle habits ( tobacco abuse ). More recent figures only show a slightly increased incidence of illness in men or even a balanced gender ratio. The incidence of the disease in African Americans and Black Africans is lower than that of whites, although an increase in incidence has been observed in African Americans over the past few decades.
etiology
The actual causes underlying the tumor development are largely unknown. The lesion is mainly classified as a true neoplasm, but according to one hypothesis it could also belong to a group of acquired multicystic reactive diseases in the head and neck area; The latter approach is supported by the polyclonality of the epithelial tumor component observed in some studies . According to recent findings, the lymphoid stroma of the Warthin tumor is also of polyclonal origin and is therefore probably only reactive and not neoplastic. In turn, other studies were able to demonstrate a translocation between chromosomes 11 and 19 with the formation of a fusion gene (CRTC1-MAML2) at least in some of the Warthin tumors . Interestingly, this change is also found in mucoepidermoid carcinoma . It is believed that the tumor is derived from heterotopic salivary ducts located in lymph nodes. This is supported by the fact that Warthin tumors are most often found superficially at the lower pole of the parotid gland, where most of the intraparotid lymph nodes are usually present. Another hypothesis interprets the Warthin tumor as an adenomatous proliferation , which is secondary to lymphocytic infiltration. A significant risk factor is cigarette smoking, which studies show that the incidence of the disease increases by a factor of 8-15 on average. Apparently there is a dose-effect relationship , with the risk increasing linearly with the duration and non-linearly with the intensity of tobacco abuse. The positive effect of the intensity of the tobacco abuse decreases at high intensities. In one study, 89% of patients with Warthin's tumor were smokers and 66% were heavy smokers. The risk of a Warthin tumor occurring on both sides is also significantly increased in smokers. One possible explanation is the damage to mitochondrial DNA by reactive oxygen species in smokers. Indeed, the epithelial cells of Warthin tumor often show loss of mitochondrial DNA and structurally abnormal mitochondria with decreased metabolic function. A single case report describes a familial occurrence of Warthin tumors in identical twins.
An increased incidence of disease was also observed after exposure to ionizing radiation , for example in atomic bomb survivors.
The possibility of viruses being involved in the development of the disease is also being discussed . For example, the human herpes virus type 8 (HHV-8) is often found in Warthin tumors. An etiological role of the Epstein-Barr virus (EBV) or the cytomegalovirus (CMV) is now considered unlikely. The incidence of Warthin tumors is said to be higher in HIV- infected patients.
Finally, an association of Warthin's tumor with various autoimmune diseases is also reported.
pathology
The tumor almost always manifests itself within the parotid gland (> 90%), preferably in its lower organ pole. 3-8% of patients show tumors in extra-land, usually in high cervical lymph nodes . This must not be confused with a lymph node metastasis , which is not observed in the pure Warthin tumor. Individual reports describe Warthin tumors in the area of the mandibular salivary gland, the lacrimal gland, the larynx, the buccal mucosa, the hard palate or the lip. In 7-12% of cases bilateral tumors are present, in 2-6% multifocal tumors. Warthin tumors account for 14-30% of all salivary gland tumors in total and 70% of all bilateral salivary gland neoplasms. Macroscopically , Warthin tumors usually appear as well-circumscribed, round to ovoid tissue masses with a light brown to gray-brown color, which is due to the high cytochrome content of the tissue. In addition to solid parts, the tumor often shows slit-shaped cystic structures up to several centimeters in size , which are filled with clear, slimy or whitish to brownish fluid.
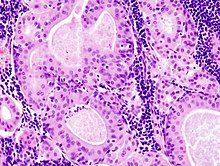
Histologically , there is a tumor that is sharply demarcated by a thin connective tissue capsule and consists of an epithelial, solid area and cyst-forming component, which is embedded in a lymphoid stroma . The epithelium lining the cyst structures shows a two-layer structure of oncocytic, highly cylindrical cells and basal, flat to cubic cells. Papillae with fibrovascular stroma are also formed. Cell debris and eosinophilic secretion products are often found in the cyst lumens . There are no noteworthy cell or nuclear atypia or significant mitotic activity . Infarcts , necroses , squamous cell metaplasia or bleeding can distort the typical histological picture. These changes can occur spontaneously or as a result of a previous fine needle biopsy . The stroma often contains lymph follicles with germinal centers and is rich in B lymphocytes .
According to Seifert, a distinction is made between four histological subtypes of Warthin's tumor, mainly depending on the quantitative ratio of the epithelial and stromal components. This classification has no clinical significance, but it does indicate to the pathologist the morphological range of the tumor.
| Histological subtype | definition | Relative frequency |
|---|---|---|
| Type 1 (classic type) | 50% epithelium, 50% stroma | 77% |
| Type 2 (low-current type) | 70-80% epithelium, 20-30% stroma | 13.5% |
| Type 3 (high current type) | 20-30% epithelium, 70-80% stroma | 2% |
| Type 4 (metaplastic type) | extensive squamous cell metaplasia | 7.5% |
Immunohistochemistry
Immunohistochemically , the oncocytic cells of the Warthin tumor show an expression of the cytokeratins 7, 8, 18 and 19, which is typical for highly cylindrical epithelia.Like the normal salivary gland parenchyma and most benign salivary gland tumors, Warthin tumors express the glycoprotein CD 9 for ribonuclease , lactoferrin , carcinoembryonic antigen (CEA) and lysozyme , while the detection of the markers amylase , vimentin and desmin is negative. In the majority of cases, bcl-2 expression can be localized in the luminal and basal epithelia . In contrast to some other benign and malignant salivary gland tumors, the epithelial tumor cells of the Warthin tumor form somatostatin in some cases . In addition, the epithelial tumor component shows an expression of progesterone but not of estrogen receptors.
cytology
The cell material obtained from a Warthin tumor by means of fine needle aspiration shows a characteristic appearance cytomorphologically - provided that a sufficient and representative amount of tissue has been obtained. Flat cell plates of oncocytic (i.e., intensely red stained in the HE staining) cell elements appear against a background consisting of lymphocytes and / or amorphous cell debris.
Ultrastructural
Under the electron microscope , the cytoplasm of the luminal cell elements of the Warthin tumor is almost completely occupied by enlarged and abnormally shaped mitochondria. The abundance of mitochondria explains the affinity of these cells for acidic dyes and thus their light microscopic oncocytic morphology. On the surface, the cells show microvilli and apocrine protrusions. Individual luminal cells are apparently also equipped with cilia. Besides mitochondria, the basal cell elements show abundant tonofilaments . Within the lumen of the cystic structures formed by the epithelial cell elements, there are cell debris to varying degrees, some of which may have been derived from degenerated lymphocytes. The stroma is formed by tightly packed lymphocytes that are stored within a mesh of reticular cells.
clinic
The affected patients are usually noticeable by a painless swelling in the area of the parotid gland. At the time of diagnosis, the average tumor size is 2-4 cm, in the extreme up to 12 cm. Less than 10% of patients have symptoms of variable magnitude.
Possible complications are infection of the tumor tissue or compression of the facial nerve running between the superficial and deep parts of the parotid gland . A facial palsy but is rarely observed.
diagnosis
Sonography , computed tomography or magnetic resonance tomography are suitable for preoperative diagnosis . Scintigraphy , which uses the property of Warthin tumors to accumulate technetium 99m pertechnetate more than the surrounding normal salivary gland tissue, has more historical significance . Under certain circumstances, a definitive diagnosis can already be made on the basis of a preoperative fine needle biopsy, although the diagnostic accuracy of this procedure for Warthin's tumor is high with over 95 percent correct diagnosis. At the latest on the surgical specimen, the diagnosis can be confirmed after a histological examination by the pathologist.
Differential diagnosis
The histological picture of the Warthin tumor is usually characteristic, so the diagnosis is usually unproblematic. Differential diagnoses to be excluded by the pathologist are lymphoepithelioma-like carcinoma or mucoepidermoid carcinoma . Warthin tumors with extensive squamous epithelial metaplasia can occasionally cause diagnostic difficulties, especially if there are simultaneous infarctions. In particular, there is a risk of being mistaken for squamous cell carcinoma , especially since the metaplastic variant of the Warthin tumor can also have cell atypia .
therapy
The standard therapy is the complete surgical tumor removal, usually in the form of a superficial (lateral) parotidectomy , in which the mostly tumor-bearing outer lobe of the parotid gland is removed, or an enucleation (peeling). The advantages of enucleation are shorter operating times, a lower frequency of complications (injury to the facial nerve with postoperative facial nerve palsy , Frey's syndrome ) and better maintenance of the function of the parotid gland. The cosmetic result is also usually cheaper. Since the Warthin tumor is a less aggressive, benign neoplasm, once the diagnosis has been confirmed, surgery can be dispensed with in multimorbid patients with a high risk of anesthesia. However, it must be carefully considered that if a diagnosis is made solely by fine needle biopsy, there is a fundamental risk that malignant tumors will also be overlooked.
forecast
Warthin tumors are characterized by slow growth. Malignant transformation has only been described in a few individual cases so far; The derived malignancies include non-Hodgkin and Hodgkin lymphomas , epidermoid carcinomas , mucoepidermoid carcinomas , squamous cell carcinomas , oncocytic adenocarcinomas and Merkel cell carcinomas . Due to the small number of cases, however, it is by no means clear whether Warthin tumors are actually associated with a statistically increased risk of degeneration, or whether it is simply a coincidental temporal and spatial coincidence of a malignant tumor with the Warthin tumor.
As a complication of the diagnostic fine needle puncture, inflammatory changes (swelling, pain, abscess formation ) occur in some cases , although there is not necessarily a bacterial infection present. This can result in a spontaneous infarction of the tumor tissue, which according to a study is observed in around 9 percent of cases after a puncture.
After surgical treatment of the Warthin tumor, low recurrence rates of 2.5-5% are observed. A recurrence of the tumor is favored by a multicentricity of the tumor tissue and an incomplete surgical removal. In contrast, an intraoperative tumor rupture does not seem to have any negative effects in this regard.
Individual evidence
- ↑ a b c d e f g h i j R. HW Simpson, JW Eveson: Warthin tumor. In: Pathology and Genetics of Head and Neck Tumours. IARCPress, Lyon 2000.
- ↑ a b c d e f A. Teymoortash: Head and neck: Salivary gland: Warthin's Tumors. In: Atlas Genet Cytogenet Oncol Haematol. April 2008. http://atlasgeneticsoncology.org//Tumors/WarthinsTumID5424.html
- ↑ a b c d S. Dubner: Parotid Tumors, Benign (November 20, 2008); http://emedicine.medscape.com/article/1289560-overview
- ↑ O. Hildebrand: About congenital epithelial cysts and fistulas of the neck. In: Arch Klin Chir. 49, 1895, pp. 167-206.
- ^ H. Albrecht, L. Doctor: Contributions to the question of tissue confusion. Papillary cystadenomas in lymph glands. In: Frankfurt Ztschr f Path. 4, 1910, p. 47.
- ↑ AS Warthin: Papillary cystadenoma lymphomatosum. A rare teratoid of the parotid region. In: J Cancer Res. 13, 1929, p. 116.
- ^ A b G. H. Yoo, DW Eisele, FB Askin, JS Driben, ME Johns: Warthin's tumor: a 40-year experience at The Johns Hopkins Hospital. In: Laryngoscope. 104 (7), Jul 1994, pp. 799-803.
- ↑ MA Yaor: The pattern of presentation of salivary gland tumors in Africa: A review of published reports. In: Ear Nose Throat J. 89 (2), Feb 2010, pp. E17-E21. PMID 20155665
- ↑ S. Suster, J. Rosai: Multilocular thymic cyst. An acquired reactive process. Study of 18 cases. In: Am J Surg Pathol . 15, 1991, pp. 388-398. PMID 2006719
- ↑ K. Honda, K. Kashima, T. Daa, S. Yokoyama, I. Nakayama: Clonal analysis of the epithelial component of Warthin's tumor. In: Hum Pathol . 31, 2000, pp. 1377-1380.
- ↑ K. Song, JD Cotelingam, M. Lowery-Nordberg, W. Sun: Characterization of the lymphoid stroma in Warthin's tumor of salivary gland by immunohistochemistry, heavy chain gene and Bcl-2 gene rearrangement. In: Am J Transl Res. 1 (4), Apr 5, 2009, pp. 352-357. PMID 19956447
- ^ ID O'Neill: New insights into the nature of Warthin's tumor. In: J Oral Pathol Med , 38 (1), Jan 2009, pp. 145-149. PMID 18647217
- ^ AS Thompson, HC Bryant: Histogenesis of papillary cystadenoma lymphomatosum (Warthin's tumor) of the parotid salivary gland. In: Am J Pathol . 26, 1950, pp. 807-849. PMID 15432614
- ↑ G. Colella, P. Biondi, A. Itro, D. Compilato, G. Campisi: Warthin's tumor distribution within the parotid gland. A feasible etiologic source from lymph nodal tissue . In: Minerva Stomatol. 59 (5), May 2010, pp. 245-249, 250-252.
- ↑ JM Aguirre, MA Echebarría, R. Martínez-Conde, C. Rodriguez, JJ Burgos, JM Rivera: Warthin tumor. A new hypothesis concerning its development. In: Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 85 (1), Jan 1998, pp. 60-63. PMID 9474616
- ↑ S. Sadetzki, B. Oberman, L. Mandelzweig, A. Chetrit, T. Ben-Tal, A. Jarus-Hakak, S. Duvdevani, E. Cardis, M. Wolf: Smoking and risk of parotid gland tumors: a nationwide case-control study. In: Cancer . 112 (9), May 1, 2008, pp. 1974-1982. PMID 18361448
- ↑ a b L. S. Freedman, B. Oberman, S. Sadetzki: Using time-dependent covariate analysis to elucidate the relation of smoking history to Warthin's tumor risk. In: Am J Epidemiol. 170 (9), Nov 1, 2009, pp. 1178-1185. PMID 19755633
- ↑ a b Peter Klussmann J, Wittekindt C, S. Florian Preuss, A. Al Attab, U. Schroeder, O. Guntinas-Lichius: High risk for bilateral Warthin tumor in heavy smokers - review of 185 cases. In: Acta Otolaryngol. 126 (11), Dec 2006, pp. 1213-1217. PMID 17050316
- ↑ L. Gallego, L. Junquera, P. Villarreal, L. Villalaín: Familial Warthin Tumor: Occurrence in Monozygotic Twins. In: J Oral Maxillofac Surg. 68 (6), Jun 2010, pp. 1400-1401. PMID 19944513
- ↑ J. Sandros, G. Stenman, J. Mark: Cytogenetic and molecular observations in human and experimental salivary gland tumors. In: Cancer Genet Cytogenet. 44, 1990, pp. 153-167. PMID 2153439
- ↑ E. Dalpa, V. Gourvas, S. Baritaki, S. Miyakis, V. Samaras, C. Barbatis, G. Sourvinos, DA Spandidos: High prevalence of Human Herpes Virus 8 (HHV-8) in patients with Warthin's tumors of the salivary gland. In: J Clin Virol. 42 (2), Jun 2008, pp. 182-185. PMID 18339579
- ↑ CJ Laane, AH Murr, AN Mhatre, KD Jones, AK Lalwani: Role of Epstein-Barr virus and cytomegalovirus in the etiology of benign parotid tumors. In: Head & Neck . 24 (5), May 2002, pp. 443-50. PMID 12001074
- ↑ E. Francavilla, P. Boccato, M. Carretta, G. Gava, F. Breda, P. Cadrobbi: Warthin's tumor during HIV infection. In: Int Conf AIDS. 8, 19-24. Jul 1992, p. 80.
- ↑ O. Gallo, C. Bocciolini: Warthin's tumor associated with autoimmune diseases and tobacco use. In: Acta Otolaryngol. 117 (4), Jul 1997, pp. 623-627. PMID 9288224
- ↑ M. Ellies, R. Laskawi, C. Arglebe: Extraglandular Warthin's Tumors: clinical evaluation and long-term follow-up. In: Br J Oral Maxillofac Surg . 36 (1), Feb 1998, pp. 52-53.
- ↑ G. Bonavolontà, F. Tranfa, p Staibano, G. Di Matteo, P. Orabona, G. De Rosa: Warthin tumor of the lacrimal gland. In: Am J Ophthalmol. 124 (6), Dec 1997, pp. 857-858. PMID 9402842
- ↑ S. Saunders, U. Igbokwe, D. Harmse: Warthin tumor of the buccal mucosa. In: Br J Oral Maxillofac Surg. 46 (4), Jun 2008, pp. 332-333. PMID 17933444
- ↑ R. Becelli, R. Morello, G. Renzi, C. Dominici: Warthin's tumor of the hard palate. In: J Craniofac Surg. 18 (5), Sep 2007, pp. 1182-1184. PMID 17912110
- ^ AD Almeida, JA Hanemann, DT Oliveira: Warthin Tumor of the Upper Lip: An Unusual Location. In: Int J Surg Pathol. 2009 Feb 3. [Epub ahead of print] PMID 19189998
- ↑ JM Hilton, JS Phillips, HB Hellquist, DJ Premachandra: Multifocal multi-site Warthin tumor. In: Eur Arch Otorhinolaryngol. 265 (12), Dec 2008, pp. 1573-1575.
- ↑ a b c PathConsult: Warthin's Tumor (January 9, 2006), Elsevier; Warthin's tumor. ( Memento from July 3, 2011 in the web archive archive.today )
- ^ S. Li, ZW Baloch, JE Tomaszewski, VA LiVolsi: Worrisome histologic alterations following fine-needle aspiration of benign parotid lesions. In: Arch Pathol Lab Med . 124 (1), Jan 2000, pp. 87-91. PMID 10629137
- ↑ J. Cossman, MJ Deegan, JG Batsakis: Warthin tumor. B-lymphocytes within the lymphoid infiltrate. In: Arch Pathol Lab Med. 101, 1977, pp. 354-356. PMID 326225
- ↑ G. Seifert, HG Bull, K. Donath: Histologic subclassification of the cystadenolymphoma of the parotid gland. Analysis of 275 cases. In: Virchows Arch A Pathol Anat Histol. 388 (1), 1980, pp. 13-38. PMID 7467121
- ↑ K. Sakamoto, T. Ono, Y. Nakamura, H. Harada, T. Nakashima: Expression of cluster of differentiation 9 glycoprotein in benign and malignant parotid gland tumors. In: J Laryngol Otol. 123 Suppl 31, May 2009, pp. 58-63. PMID 19460206
- ↑ ES Abd Elhamid, MH Elshafei: Immunohistochemical localization of mdm-2, p27 Kip1 and bcl-2 in Warthin's tumor of the parotid gland. In: Diagn Pathol. 4 (1), May 16, 2009, p. 14. PMID 19445705
- ↑ Y. Hayashi, H. Saito, S. Saito, T. Yanagawa, H. Yoshida, Y. Yura, M. Sato: Immunoreactive somatostatin in Warthin's tumor. In: Am J Pathol . 123 (2), May 1986, pp. 250-255. PMID 2871759 .
- ↑ A. Teymoortash, BM Lippert, JA Werner: Steroid hormone receptors in parotid gland cystadenolymphoma (Warthin's tumor). In: Clin Otolaryngol Allied Sci. 26 (5), Oct 2001, pp. 411-416. PMID 11678950
- ↑ AV Parwani, SZ Ali: Diagnostic accuracy and pitfalls in fine-needle aspiration interpretation of Warthin tumor. In: Cancer. 99 (3), Jun 25, 2003, pp. 166-171. PMID 12811857 .
- ^ Y. Yu: Ultrastructural study of adenolymphoma. In: Zhonghua Kou Qiang Yi Xue Za Zhi. 26 (3), May 1991, pp. 155-157, 191.
- ↑ a b c B. T. Hwang, K. Sugihara, K. Kawashima, S. Yamashita: Scanning electron microscopic study of Warthin's tumor. In: J Oral Pathol. 16 (3), Mar 1987, pp. 118-123.
- ↑ NM el-Hossary, LM Fathy: Luminal epithelium of Warthin's Tumors: a scanning electron microscopic study. In: Egypt Dent J. 40 (3), Jul 1994, pp. 791-794. PMID 9588158
- ↑ I. Dardick, A. Claude, WR Parks, D. Hoppe, J. Stinson, BF Burns, J. Little, Brown DL, SH Dairkee: Warthin's tumor: an ultra structural and immunohistochemical study of basilar epithelium. In: Ultrastruct Pathol. 12 (4), 1988, pp. 419-432. PMID 2458648
- ↑ A. Franzen: Ear, Nose and Throat Medicine . Elsevier, Urban & Fischer Verlag, 2007, ISBN 978-3-437-42961-3 .
- ↑ AE Canbay, S. Knorz, KD Heimann, H. Hildmann, KU Tiedjen: Value of scintigraphy and sonography in the diagnosis of cystadenolymphomas of the parotid gland. In: Laryngorhinootologie. 81 (11), Nov 2002, pp. 815-819. PMID 12458467
- ↑ LL Veder, JD Kerrebijn, FM Smedts, MA den Bakker: Diagnostic accuracy of fine-needle aspiration cytology in Warthin tumors. In: Head Neck. 2010 Mar 26. PMID 20848407
- ↑ CDM Fletcher: Diagnostic Histopathology of Tumors. 3. Edition. Churchill Livingstone, 2007.
- ^ H. Yerli, S. Avci, E. Aydin, U. Arikan: The metaplastic variant of Warthin tumor of the parotid gland: dynamic multislice computerized tomography and magnetic resonance imaging findings with histopathologic correlation in a case. In: Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 109 (3), Mar 2010, pp. E95 – e98. Epub 2009 Dec 6. PMID 19969491
- ↑ GY Yu, DQ Ma, XB Liu, MY Zhang, Q. Zhang: Local excision of the parotid gland in the treatment of Warthin's tumor. In: Br J Oral Maxillofac Surg. 36 (3), Jun 1998, pp. 186-189. PMID 9678883
- ↑ VM Reddy, T. Thangarajah, F. Castellanos-Arango, A. Panarese: Conservative management of warthin tumor. In: J Otolaryngol Head Neck Surg. 37 (5), Oct 2008, pp. 744-749. PMID 19128687
- ^ MR Raymond, JH Yoo, JG Heathcote, CM McLachlin, HB Lampe: Accuracy of fine-needle aspiration biopsy for Warthin's tumors. In: J Otolaryngol. 31 (5), Oct 2002, pp. 263-270. PMID 12512889
- ↑ T. Thangarajah, VM Reddy, F. Castellanos-Arango, A. Panarese: Current controversies in the management of Warthin tumor. In: Postgrad Med J. 85 (999), Jan 2009, pp. 3-8. PMID 19240281
- ↑ S. Gorai, T. Numata, S. Kawada, M. Nakano, J. Tamaru, T. Kobayashi: Malignant lymphoma arising from heterotopic Warthin's tumor in the neck: case report and review of the literature. In: Tohoku J Exp Med. 212 (2), Jun 2007, pp. 199-205. PMID 17548964
- ↑ M. Melato, G. Falconieri, R. Fanin, M. Baccarani: Hodgkin's disease occurring in a Warthin's tumor: first case report. In: Pathol Res Pract. 181 (5), Oct 1986, pp. 615-620. PMID 3786253
- ↑ F. Bolat, F. Kayaselcuk, AN Erkan, CA Cagici, N. Bal, I. Tuncer: Epidermoid carcinoma arising in Warthin's tumor. In: Pathol Oncol Res. 10 (4), 2004, pp. 240-242. PMID 15619648
- ^ S. Yamada, T. Matsuo, S. Fujita, K. Suyama, A. Yamaguchi, A. Mizuno: Mucoepidermoid carcinoma arising in Warthin's tumor of the parotid gland. In: Pathol Int. 52 (10), Oct 2002, pp. 653-656. PMID 12445138
- ^ GA Morrison, HJ Shaw: Squamous carcinoma arising within a Warthin's tumor of the parotid gland. In: J Laryngol Otol. 102 (12), Dec 1988, pp. 1189-1191. PMID 3066838
- ^ O. Bengoechea, F. Sanchez, B. Larrinaga, JM Martinez-Penuela: Oncocytic adenocarcinoma arising in Warthin's tumor. In: Pathol Res Pract. 185, 1989, pp. 907-911. PMID 2482485
- ^ A. Fornelli, V. Eusebi, G. Pasquinelli, P. Quattrone, J. Rosai: Merkel cell carcinoma of the parotid gland associated with Warthin tumor: report of two cases. In: Histopathology. 39 (4), Oct 2001, pp. 342-346. PMID 1168393
- ↑ K. Suzuki, H. Iwai, T. Kaneko, M. Sakaguchi, S. Hoshino, M. Inaba: Induction of parotitis by fine-needle aspiration in parotid Warthin's tumor. In: Otolaryngol Head Neck Surg. 141 (2), Aug 2009, pp. 282-284. PMID 19643266
- ^ TR Taylor, NJ Cozens, I. Robinson: Warthin's tumor: a retrospective case series. In: Br J Radiol. 82 (983), Nov 2009, pp. 916-919. Epub 2009 May 11. PMID 19433486
- ↑ M. Ethunandan, CA Pratt, B. Higgins, A. Morrison, T. Umar, DW Macpherson, AW Wilson: Factors influencing the occurrence of multicentric and 'recurrent' Warthin's tumor: a cross sectional study. In: Int J Oral Maxillofac Surg. 37 (9), Sep 2008, pp. 831-834. PMID 18550337