Epstein-Barr Virus
| Epstein-Barr Virus | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|

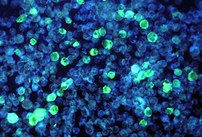
Virions of the EBV ( TEM image , deformations due to the preparation) |
||||||||||||||||||||
| Systematics | ||||||||||||||||||||
|
||||||||||||||||||||
| Taxonomic characteristics | ||||||||||||||||||||
|
||||||||||||||||||||
| Scientific name | ||||||||||||||||||||
| Human gammaherpesvirus 4 | ||||||||||||||||||||
| Short name | ||||||||||||||||||||
| HHV4 | ||||||||||||||||||||
| Left | ||||||||||||||||||||
|
The Epstein-Barr virus ( EBV , also Human Herpesvirus 4 , HHV4 , en. Human gammaherpesvirus 4 ) is a species of human pathogenic , enveloped , double-stranded DNA viruses from the Herpesviridae family . The Epstein-Barr virus was first described in 1964 by Michael Epstein and Yvonne M. Barr . They discovered EBV in B lymphocytes obtained from an African patient with Burkitt's lymphoma . The Epstein-Barr virus is the first human oncovirus to be discovered .
transmission
The main route of transmission of the virus is a droplet infection or a contact infection (especially saliva) or smear infection , transmission in the context of transplants or blood transfusions is less common . The fact that EBV could also be found in secretions from the genitals makes the transmission path through sexual contact conceivable.
At the molecular level, complement receptor type 1 (CR1) and complement receptor type 2 (CR2) are described as adhesion factors on the cell surface. The EBV uses integrins or HLA-II (HLA class II histocompatibility antigen) for entry into cells .
Consequences of infection
The infection with the virus is usually carried out in childhood. While there are usually no symptoms in this case, in adolescents or adults infected, Pfeiffer glandular fever (infectious mononucleosis) breaks out in 30–60% of all cases . From the age of 40, around 98% of people are infected with EBV. The virus persists in the body for life after both an asymptomatic and symptomatic infection . Like all herpes viruses , it can be reactivated. Usually, reactivation is not noticed by the host and is quickly curbed by its immune system . If there is immunosuppression (e.g. in people infected with HIV or in recipients of organs), the virus can multiply in an uncontrolled manner and contribute to the development of various rare cancers . For around 40 years it has been suspected that EBV plays an important etiological role in diseases such as Hodgkin's disease (lymph gland cancer), Burkitt's lymphoma and other lymphomas and in post-transplant lymphoproliferative disease . EBV thus belongs together with the hepatitis B virus (HBV), the hepatitis C virus (HCV), the human papillomavirus (HPV), the human T-lymphotropic virus 1 (HTLV-1) and the human herpes virus 8 ( HHV-8, also Kaposi's sarcoma herpes virus , KSHV) to a group of human viruses that are responsible for 10 to 15 percent of all cancers worldwide.
In the recent past, the suspicion that EBV is associated with a variety of autoimmune diseases , such as B. Multiple sclerosis , systemic lupus erythematosus and rheumatoid arthritis related. However, there are also indications that an infection with EBV cannot at least not be regarded as the sole cause of later autoimmune diseases. And the chronic fatigue syndrome and encephalitis lethargica be related to the virus in conjunction. In Africa there is also an ( endemic ) variant of EBV-associated Burkitt's lymphoma that has repeatedly led to epidemics .
An EBV infection is a possible risk factor for tumors of the nose or the larynx ( nasopharyngeal carcinoma ). However, EBV alone is not sufficient for cancer development, as the low number of cancer cases compared to the virus spread shows. Other factors play a role here (chromosomal translocation of the c-myc gene ). Malaria is also discussed as a potential accompanying influencing factor (cofactor) . Human breast cancer cells are also often infected by Epstein-Barr viruses, without a causal connection being seen.
Although EBV should not be considered a breast cancer virus, it alters the response of breast cancer cells to the taxanes used in chemotherapy . Even more common than breast cancer cells are fibroadenomas of the breast infected by Epstein-Barr virus.
Bacterial accompanying infections are possible.
Diagnosis
In general, when infected with the Epstein-Barr virus, there is almost always an increased proportion of lymphocytes in the total white blood cells (so-called relative lymphocytosis). The total number of white blood cells may be decreased, normal or increased. If a blood smear is examined under the microscope, one sees atypical mononuclear cells with characteristic changes (so-called Pfeiffer cells - specific cytotoxic ( CD8 + ) T lymphocytes morphologically directed against EBV that have a round or bulged nucleus (rarely lobed)), which sometimes already enable the diagnosis. Furthermore, the liver values are often increased.
The serological assessment of the EBV status is not always easy. In some places, so-called rapid tests are used to detect the acute infection ; however, depending on age, they can deliver up to 20% false positive and 30% false negative results. The diagnosis (normal immunocompetent patients) should be staggered, and the constellations that some patients or doctors find on their laboratory report are sometimes a little difficult to interpret:
- The detection of IgG - antibodies against the nuclear antigen of EBV (EBNA-1-IgG) proves the presence of the virus. If the EBNA-1 IgG test is clearly positive, any further virus detection test is unnecessary in the case of an acute illness (mononucleosis). Mononucleosis after a fresh infection is excluded if the EBNA IgG test is positive, as these antibodies are only produced by the immune system several weeks to months after the onset of symptoms and when the virus is latency. EBNA-1 IgG antibodies are detectable in around 95% of people with a history of EBV infection.
- If the EBNA-1-IgG is negative, the IgG should be tested against the viral capsid antigen (VCA-IgG). It is a marker of current or previous contact with EBV and usually remains detectable for life.
- To detect an acute infection, if the VCA-IgG is positive, the IgM antibodies are tested against the viral capsid (VCA-IgM). If these are positive, this indicates a fresh or recent infection (but does not prove it!).
- The VCA-IgM can persist during intense physical activity (especially in competitive athletes). One speaks of a prolonged (prolonged) healing if the EBNA-1-IgG is already positive.
- In diagnostic problem cases, an acute infection can often be distinguished from a previous infection by means of an immunoblot and / or an avidity test. Evidence of high avidity of the VCA-IgG antibodies proves that the time of infection was a long time ago; a clear VCA-p18 band in the IgG immunoblot also suggests this. Typical findings in an acute infection are: Absence of EBNA-1 IgG antibodies, low avidity of VCA IgG antibodies and detection of IgG and / or IgM antibodies against EA ( early antigen ).
- In the case of immunodeficiency (immune incompetence), the virus can go from the resting phase ( latency ) back to active reproduction (reactivation). In this case, the EBNA-1-IgG can become negative again, for example in HIV patients. A reliable assessment of EBV reactivations in the case of immunodeficiency is only possible by determining the viral load by means of the polymerase chain reaction .
- The direct detection of the virus DNA by means of the polymerase chain reaction does not usually make sense in the immune system, since the latent genome can also be detected in the blood and at the same time symptomless carriers excrete the virus constantly or temporarily with the saliva. The above-mentioned reactivations do not usually cause any symptoms to an immune-healthy person, they only represent a laboratory diagnostic problem, as the detection of VCA-IgG in high concentrations and possibly recurring VCA-IgM can lead to misinterpretations.
A particular specialty of EBV is that the acute infection of B-lymphocytes (especially B-memory cells ) with EBV enables them to form IgM antibodies from infections or vaccinations that have long since healed . These patients then often show the simultaneous presence of IgM against rubella , measles , hepatitis A , CMV and the like. v. m. and thus imitate an acute infection with these pathogens serologically. A patient with more than one positive IgM is therefore always suspect of EBV.
literature
- MA Epstein, BG Achong, YM Barr: Virus particles in cultured lymphoblasts from Burkitt's lymphoma. In: The Lancet . 1964, Vol. 283, No. 7335, pp. 702-3.
- MA Epstein, G. Henle et al .: Morphological and biological studies on a virus in cultured lymphoblasts from Burkitt's lymphoma. In: J. Exper. Med. No. 121, 1965, pp. 761-70.
- DH Crawford: Biology and Disease Associations of Epstein-Barr Virus. In: Philos Trans R Soc Lond B Biol Sci. Volume 356, 2001, pp. 461-473.
- W. Amon, PJ. Farrell: Reactivation of Epstein-Barr virus from latency. In: Rev Med Virol. May-June 2005, Vol. 15, No. 3, pp. 149-56, PMID 15546128 .
Web links
- University of Veterinary Medicine, Vienna: Epstein-Barr virus ( Memento from March 19, 2011 in the Internet Archive )
Individual evidence
- ↑ a b c d e ICTV: ICTV Taxonomy history: Human alphaherpesvirus 1 , EC 51, Berlin, Germany, July 2019; Email ratification March 2020 (MSL # 35)
- ↑ Javier G. Ogembo, Lakshmi Kannan, Ionita Ghiran, Anne Nicholson-Weller, Robert W. Finberg: Human Complement Receptor Type 1 / CD35 Is an Epstein-Barr Virus Receptor . In: Cell Reports . tape 3 , no. 2 , February 2013, p. 371–385 , doi : 10.1016 / j.celrep.2013.01.023 ( elsevier.com [accessed April 30, 2020]).
- ↑ J. Tanner, Y. Whang, J. Sample, A. Sears, E. Kieff: Soluble gp350 / 220 and deletion mutant glycoproteins block Epstein-Barr virus adsorption to lymphocytes. In: Journal of Virology . tape 62 , no. 12 , December 1, 1988, ISSN 0022-538X , pp. 4452-4464 , PMID 2460635 ( asm.org [accessed April 30, 2020]).
- ↑ LS Chesnokova, SL Nishimura, LM Hutt-Fletcher: Fusion of epithelial cells by Epstein-Barr virus proteins is triggered by binding of viral glycoproteins gHgL to integrins v 6 or v 8 . In: Proceedings of the National Academy of Sciences . tape 106 , no. 48 , December 1, 2009, ISSN 0027-8424 , p. 20464-20469 , doi : 10.1073 / pnas.0907508106 ( pnas.org [accessed April 30, 2020]).
- ^ Q. Li, MK Spriggs, S. Kovats, SM Turk, MR Comeau: Epstein-Barr virus uses HLA class II as a cofactor for infection of B lymphocytes . In: Journal of Virology . tape 71 , no. 6 , June 1997, ISSN 0022-538X , pp. 4657-4662 , PMID 9151859 ( nih.gov [accessed April 30, 2020]).
- ↑ E. Maeda et al. : Spectrum of Epstein-Barr virus-related diseases: a pictorial review . In: Jpn J Radiol . Volume 27, No. 1, 2009, pp. 4-19. PMID 19373526 .
- ↑ MK Ghandi: Epstein-Barr virus-associated lymphomas . In: Expert Rev Anti Infect Ther . Volume 4, No. 1, 2006, pp. 77-89. PMID 16441211 .
- ↑ SA Rezk, LM Weiss: Epstein-Barr virus-associated lymphoproliferative disorders . In: Hum Pathol . Volume 38, No. 9, 2009, pp. 1293-1304. PMID 17707260 .
- ↑ M. Rowe et al .: Burkitt's lymphoma: the Rosetta Stone deciphering Epstein-Barr virus biology . In: Semin Cancer Biol . Volume 19, No. 6, 2009, pp. 377-388. PMID 19619657 .
- ↑ D. Martin, JS Gutkind: Human tumor-associated viruses and new insights into the molecular mechanisms of cancer . In: Oncogene . Volume 27, No. 2, 2008, pp. 31-42. PMID 19956178 .
- ↑ E. Toussirot, J. Roudier: Epstein-Barr virus diseases in autoimmune . In: Best Pract Res Clin Rheumatol . Volume 22, No. 5, 2008, pp. 883-896. PMID 19028369 .
- ^ BA Bagert: Epstein-Barr virus in multiple sclerosis . In: Curr Neurol Neurosci Rep . Volume 9, No. 5, 2009, pp. 405-410. PMID 19664371 .
- ^ D. Pohl: Epstein-Barr virus and multiple sclerosis . In: J Neurol Sci . Volume 286, No. 1-2, 2009, pp. 62-64. PMID 19361810 .
- ↑ Julia Rautenstrauch: IDW . In: Information Service Science . September 14, 2009; Retrieved December 20, 2009.
- ↑ Kristin Strohschein, Madlen Loebel et al .: Deficient EBV-Specific B- and T-Cell Response in Patients with Chronic Fatigue Syndrome . In: PLOS ONE . tape 9 , no. 1 , January 15, 2014, ISSN 1932-6203 , p. e85387 , doi : 10.1371 / journal.pone.0085387 , PMID 24454857 .
- ^ F. Alarcón: Encephalitis lethargica due to Epstein-Barr virus infection . In: Mov Disord . 2011. PMID 21611982 .