Avian influenza
The avian flu is also called avian influenza (of lat. Avis , bird), as bird flu predominantly and since 1981 as a highly pathogenic influenza virus infection ( HPAI , H ighly P athogenic A vian I referred nfluenza). It is a virus- induced animal notifiable disease that can affect chickens , turkeys , geese , ducks , wild waterfowl and other birds. When infected with the more aggressive strains of the virus, it usually leads to the death of the infected birds , provided they are not among the reservoir hosts. Some variants of the avian influenza virus, in particular variant A / H5N1 , have been transmitted in individual cases to humans, zoo animals such as leopards and domestic cats . HPAIV and LPAIV of subtypes A / H5 and A / H7 in wild birds and domestic poultry are subject to animal disease law and are therefore notifiable.
Avian influenza was first observed in Italy in 1878 . There were multiple outbreaks in Europe, America, and Asia in the 1930s. When avian flu spread to Ireland and the United States in 1983, millions of birds were killed to contain the outbreaks. There was another major outbreak each in 1992 in Mexico , 1997 in Hong Kong and 2015 in the USA .
As a result of the events related to avian influenza H5N1 , avian influenza H7N9 and avian influenza H5N8 , influenza subtypes A / H5N1, A / H7N9 and A / H5N8 received special media attention.
It is not certain whether the so-called English sweat , which was associated with bird death in the 15th and 16th centuries, was also an illness caused by influenza viruses.
Pathogen
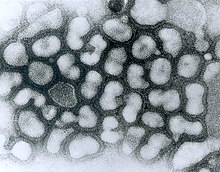
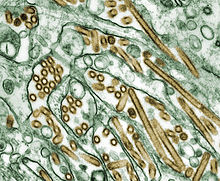
The causative agent of classical avian influenza (KP) is a highly pathogenic avian influenza virus (HPAIV) called influenza A virus (i.e. flu virus) and thus an enveloped single (-) - stranded RNA virus [ss (-) RNA] the orthomyxovirus family .
In general, 3 types are distinguished according to the OIE Manual.
- LPAIV (Low Pathogenic Avian Influenza Virus) : low pathogenic virus, not subtype H 5, H 7
- LPNAIV (Low Pathogenic Notifiable Influenza Virus) : low pathogenic virus ( IVPI <1.2 or corresponding hemagglutinin sequence) of type H5 or H7
- HPNAIV (Highly Pathogenic Notifiable Influenza Virus) : Highly pathogenic virus (IVPI> 1.2 or typical hemagglutinin sequence with basic amino acids at the cleavage site) of type H5 or H7
The correct name for an influenza virus would be: A / goose / Guangdong / 1/96 (H5N1): "A" for the influenza subtype (A, B, or C); " goose " for the English name of the host from which the virus was first isolated; " Guangdong " for the place name of the first occurrence, the first number for the number of the sample and the second number for the year.
It was not until 1954 that the German virologist Werner Schäfer, who was then working at the Max Planck Institute for Virus Research in Tübingen, finally proved that the viruses of human influenza and classic avian influenza belong to the same group.
Subtypes and pathogenicity
As a result of genetic changes , new variants of the flu virus are constantly emerging. These variants are divided into subtypes based on certain surface properties (for a detailed explanation of the variability of the pathogens see under Influenza ). There are 18 H subtypes and 11 N subtypes. Type A / H5N1, for example, has the 5th variant of hemagglutinin (H5) and the 1st variant of neuraminidase (N1) on its surface . These sub-types usually only infect certain hosts at a time, while a wider range of infection vectors can spread them without these animals becoming ill.
Mutations can change both the host species and the pathogenic properties considerably. Here the surface protein hemagglutinin plays an important role, which is responsible for the recognition and attachment of the virion to the host cell. This hemagglutinin is formed as precursor HA0 and must then be split into two subunits (HA1 & HA2) by certain host enzymes, so-called proteases, so that the viruses can infect new cells.
The hemagglutinin of the less pathogenic virus strains (they are also referred to as less pathogenic or abbreviated as LPAI in English ) can only be cleaved by extracellular trypsin-like proteases, which are only present in the respiratory and digestive tract and thus limit the infection locally.
The cleavage site of highly pathogenic virus strains (HPAI) contains basic amino acids so that it is cleaved by ubiquitous, intracellular, so-called furin-like proteases and thus allows infection of the entire host.
So far, highly pathogenic variants are only known from the HA subtypes H5 and H7.
Many of the possible combinations of H and N have been detected in water birds such as ducks and geese, including less pathogenic variants of A / H5N1. Since no natural reservoir for highly pathogenic variants of the avian influenza virus has been detectable up to now, the virologists are currently assuming that the transition from a less pathogenic to a highly pathogenic state was the result of a mutation, which at the same time allows the species barrier of duck birds to be removed (Anatidae ) to overcome chicken birds (Galliformes). According to Science , such transitions have occurred at least 19 times since 1959 and each resulted in an epidemic among farmed poultry. In some of these cases, it was even possible to trace the path from a less pathogenic state in water birds to a less pathogenic state in chicken birds to a highly pathogenic state in chicken birds.
Transitions to humans have been documented so far (as of April 2015) for A / H5N1, A / H6N1, A / H7N2, A / H7N3, A / H7N7, A / H9N2, A / 10N7 and A / H11N9.
The following subtypes in particular have caused great damage in poultry holdings:
A / H5N1
The subtype A / H5N1 is considered to be particularly aggressive ( HPAI, Highly Pathogenic Avian Influenza ). An altered non-structural gene means that certain messenger substances in the immune system , which normally fight off viruses, no longer have any effect on the A / H5N1 subtype. That is why it kills infected birds that do not belong to its virus reservoir very quickly and, because of its pathogenic properties , it is closely monitored by scientists for interdependencies with other phyla and transgressions of species boundaries ; according to the World Health Organization , A / H5N1 is the only subtype of the H5 group that can be transmitted to humans. For more details on the current A / H5N1 outbreaks in poultry and humans, see Avian Influenza H5N1 and Distribution of H5N1 .
A highly pathogenic avian A / H5N1 virus first appeared in chicken birds in Scotland in 1959: A / chicken / Scotland / 59 (H5N1).
A / H5N2
This subtype may have occurred. a. in Japan in the summer of 2005, as a result of which, according to press reports, more than 1.5 million chickens and other poultry were killed. There had been several outbreaks in poultry farms in the United States in 1983 and 1984, killing 17 million animals. There were also several outbreaks in Mexico between 1992 and 1995. In December 2008 a low pathogenic H5N2 virus was found in Belgium and Germany. This led to the culling of three poultry stocks in Lower Saxony.
A / H5N3
This subtype caused large deaths among wild tern in South Africa in 1961 . This was also the first detection of influenza viruses in a wild bird population. In October 2008, a low-pathogen H5N3 virus was detected in a goose at the Leipzig Zoo as part of a routine check. In the same year there were outbreaks in several poultry farms in the district of Cloppenburg, Lower Saxony. As a result, over 560,000 head of poultry were killed in this region by the end of January 2009.
A / H7N1
From March 1999, a massive epidemic broke out in Italy, as a result of which more than 13 million animals were affected by the beginning of 2000. There was no evidence of transmission to humans.
A / H7N3
In North America, the spread of this subtype has been confirmed several times. Most recently, in April 2004, 18 farms in British Columbia were quarantined and two cases of human transmission were documented.
A / H7N7
In 2003, 89 human infections with this ( HPAI, Highly Pathogenic Avian Influenza ) subtype were confirmed in the Netherlands . One case was fatal. It was a veterinarian who was able to detect this virus subtype in the lung tissue. In addition, 30,000 useful birds had to be killed. In 1996 there was an infection in the UK . In 2013 in China, in an attempt to reconstruct the reassortment of influenza A viruses prior to the outbreak of the H7N9 avian flu , a previously unknown variant of A / H7N7 was isolated from over-the-counter chickens that could also be transferred to ferrets in the laboratory ; With regard to influenza, ferrets are regarded as a model organism for humans.
A / H7N9
Presumably after contact with infected poultry, people were infected for the first time in February 2013 by the so-called H7N9 bird flu and, as a result, deaths in people from the H7N9 influenza A virus in the People's Republic of China .
transmission
Avian influenza can infect all bird species. Wild ducks and other waterfowl are considered natural reservoirs for the virus, but they usually do not become seriously ill because the virus has adapted to them. It needs these reservoir hosts for its reproduction. Chickens and turkeys in particular are at greater risk, but also pheasants , quails , guinea fowl and wild birds. Migratory water birds, sea birds and shorebirds are less susceptible to the disease. However, they are vectors and their migratory behavior contributes to their wide geographic distribution. Although pigeons are not said to be very susceptible to bird flu viruses themselves, it is feared that they spread the pathogen as mechanical vectors in the plumage. For example, the North Rhine-Westphalian State Environment Ministry declared a pigeon flight ban during a rampant avian influenza in 2003.
Mammals are less susceptible to the virus, but - such as domestic pigs - are occasionally infected. It was reported from Thailand that tigers and leopards died of A / H5N1 in two zoos after eating infected poultry.
Basically, the same infection routes are observed as with other influenza viruses . The viruses spread through droplet infection via inhaled air or via fecal particles on clothing and equipment. Outside of their hosts, the avian flu pathogens are usually only functional for a few days, and under favorable conditions for many months. Avian influenza viruses generally remain intact for 105 days in liquid manure, 30 to 35 days in feces and poultry meat or eggs at 4 ° C, and for seven days at 20 ° C. According to previous knowledge, transmission via cooked poultry and other meat products is excluded.
Symptoms
The acute form of avian influenza manifests itself in signs of general weakness ( apathy , inappetence , dull, shaggy plumage), high fever , difficult breathing with open beak, edema on the head, neck, crest, wattles, legs and feet, blue discoloration of the skin and the Mucous membranes , watery-slimy and greenish diarrhea and neurological disorders (strange posture of the head, motor disorders ).
With a chronic course, the laying performance decreases, the eggs are thin-walled or shell-less.
The mortality depends on the age of the animals and the virulence of the pathogen. With highly virulent pathogens, the disease is fatal in almost all animals. More than 15% of a flock of poultry can die before symptoms appear ( peracute course ).
Combat
In the event of outbreaks of avian influenza in animal husbandry, the entire animal population of the affected keeper is regularly killed . The carcasses are burned or otherwise rendered harmless to prevent transmission to other livestock. Therefore, the number of animals killed is usually much larger than the number of animals that have been proven to be infected.
In principle, the animals can also be effectively protected against avian influenza by a preventive vaccination . However, based on current knowledge, a live vaccine based on low pathogen pathogens is ruled out because of the risk of mutation . Immunization with inactivated influenza viruses is also controversial among experts, however, since no vaccine available to date prevents subsequent infection, the subsequent virus replication and the excretion of pathogenic viruses; Rather, only the clinical disease of the vaccinated animals is prevented. In this way, vaccinated animals can become virus carriers and spread pathogenic viruses. Another problem is the reliable (microbiological / serological) differentiation of the vaccinated animals from sick or contagious animals.
As a solution to this dilemma vaccines were in Central America and East Asia therefore already been developed and - especially against A / H5N1 - already used that from attenuated fowl pox made viruses, which the hemagglutinin H5 was inserted. A German research group from the Friedrich Loeffler Institute is trying u. a. to genetically modify a common vaccine strain against Newcastle disease so that it is available for vaccination against H5 or H7. In animals vaccinated in this way, suitable antibody detection tests could later be used to differentiate whether they only show an immune response against the vaccine or - in the case of a virus infection - against the pathogenic viruses. Work at the University of Veterinary Medicine Hanover suggests that the use of marker vaccines based on a non-communicable vesicular stomatitis virus (VSV) could be successful in differentiating between infected and vaccinated animals and in safety.
In Germany, avian influenza control takes place on the legal basis of the Animal Diseases Act and the Avian Influenza Ordinance , which in October 2007 summarized several other ordinances that were issued after the first massive occurrence of A / H5N1.
In order to combat the bird flu, which was also spreading again in Germany in 2016, existing regulations were temporarily extended to smaller holdings by means of a statutory ordinance.
Because many birds are able to transmit the pathogen ( vector properties ), the trade or breeding of, for example, parrots and parakeets must be officially approved. These non-native bird species tend to escape occasionally despite being kept in cages and can therefore also contribute to the uncontrolled spread of avian influenza, as last happened in Cologne in 2004/2005.
Genetic engineering
British scientists from the University of Cambridge , University of Edinburgh and the Veterinary Laboratories Agency have transgenic chickens developed which can not transmit the avian influenza. The chickens were fitted with an expression cassette which produced a piece of RNA that served as a bait for polymerase. Instead of binding to the virus genome and thereby helping the virus to replicate, the polymerase then clings to this bait. The transgenic chickens still died from avian influenza, but no longer infected other chickens. The aim is the complete immunization of chickens against A / H5N1. In 2019, the first genetically modified animals with full immunity will be hatched at the Roslin Institute at the University of Edinburgh.
See also
- Atypical avian influenza (Newcastle disease)
- Spanish flu
- Equine influenza
- Stable compulsory
- World Organization for Animal Health
literature
- David E. Swayne (Ed.): Avian Influenza. Blackwell Publishing, 2008, ISBN 978-0-8138-2047-7 .
Web links
- What do you mean by "bird flu" and avian influenza? Answers from the German Federal Ministry for Food, Agriculture and Consumer Protection .
- Bird flu in animals - information from the Swiss Federal Food Safety and Veterinary Office
- Austrian Influenza Pandemic Plan.
- Friedrich-Loeffler-Institut : Information sheet on classical avian influenza (PDF; 152 kB)
- Robert Koch Institute : Advice for Doctors: Influenza (Seasonal Influenza, Influenza A (H1N1) 2009, Avian Influenza) Avian influenza.
- Federal Ministry of Justice : German ordinance on protection against avian influenza of October 18, 2007
- German Animal Health Act
- World Health Organization (WHO): Influenza at the Human-Animal Interface.
- EU legislation to combat avian influenza
- Foreign animal diseases, the gray book. (PDF; 4.6 MB) Study by the Committee on Foreign Animal Diseases of the US Animal Health Association from 2008 (English)
- English language website of the International Society for Infectious Diseases
Individual evidence
- ↑ Adjective avian "related to birds", " coming from birds" from Latin avis "bird"
- ↑ Jacqueline P. Jacob et al .: Avian Influenza in Poultry. Source: The Institute of Food and Agricultural Sciences (IFAS) at the University of Florida , as of April 2014, accessed on June 5, 2015.
- ↑ Werner Schäfer: Comparative sero-immunological studies on the viruses of influenza and classic avian influenza. In: Journal of Nature Research B . 10, 1955, pp. 80-91 ( online ).
- ↑ Research Report 1/2006 of the Senate of the Federal Research Centers , p. 5.
- ↑ Dennis Normile: Are Wild Birds to Blame? In: Science . Volume 310, No. 5747, 2005, p. 426, doi: 10.1126 / science.310.5747.426
- ^ Mathilde Richard et al. : Limited airborne transmission of H7N9 influenza A virus between ferrets. In: Nature . Volume 501, No. 7468, 2013, pp. 560-563, doi: 10.1038 / nature12476
- ↑ Sung-Hsi Wei et al. : Human infection with avian influenza A H6N1 virus: an epidemiological analysis. In: Tha Lancet . Volume 1, No. 10, 2013, pp. 771-778, doi: 10.1016 / S2213-2600 (13) 70221-2
- ↑ Dennis J. Alexander: A review of avian influenza in different bird species. In: Veterinary Microbiology. Volume 74, 2000, pp. 3–13, full text (PDF)
- ↑ WB Becker: The isolation and classification of tern virus influenza virus A / Tern / South Africa / 1961. Journal of Hygiene, Volume 64, p. 309 (1966)
- ↑ Avian influenza in the district of Cloppenburg is spreading. On: aerztezeitung.de from December 15, 2008
- ↑ The exclusion zone around the ostrich farm has been lifted. Review on: suedkurier.de from January 15, 2014
- ^ Ilaria Capua et al. : The 1999-2000 avian influenza (H7N1) epidemic in Italy: veterinary and human health implications. In: Acta Tropica. Volume 83, No. 1, 2002, pp. 7-11, doi: 10.1016 / S0001-706X (02) 00057-8
- ↑ a b For numerous references see: Scott Krauss, Robert G. Webster: Predicting the Next Influenza Virus. In: Science. Volume 337, No. 6095, 2012, p. 644, doi: 10.1126 / science.337.6095.644-a
- ↑ Avian Influenza A Virus Infections of Humans / Instances of Avian Influenza A Virus Infections of Humans. On: cdc.gov of May 23, 2008
-
↑ Tommy Tsan-Yuk Lam: The genesis and source of the H7N9 influenza viruses causing human infections in China. In: Nature. Volume 502, 2013, pp. 241–244, doi: 10.1038 / nature12515
H7N7 viruses: the new bird flu has a potentially dangerous relative. On: zeit.de from August 21, 2013 -
↑ H7N9 avian influenza human infections in China. On: who.int of April 1, 2013
Süddeutsche Zeitung of April 2, 2013: New type of bird flu calls WHO on the scene.
straitstimes.com: Man dies of H7N9 bird flu in China, third fatality from lesser-known strain. ( Memento from April 4, 2013 in the Internet Archive ) - ↑ Research Report 1/2006 of the Senate of the Federal Research Centers, p. 7
- ↑ Nazeer Hussain Kalhoro: Generation and Evaluation of a DIVA (Differentiating Infected from Vaccinated Animals) Vector Vaccines for Protection of Poultry against Avian Influenza virus infections : German title: Production and Evaluation of DIVA (Differentiation of infected and vaccinated animals) vector vaccines for Protection of poultry against infections with avian influenza viruses , Hanover, University of Veterinary Medicine, dissertation, 2008. Full text (PDF, English; 18.9 MB) and summary (HTML, abstract, German and English)
- ↑ Ordinance on special protective measures in small poultry holdings
-
↑ Martin Enserink: Transgenic Chickens Could Thwart Bird Flu, Pandemic Curb Risk. In: Science. Volume 331, No. 6014, 2011, pp. 132-133, doi: 10.1126 / science.331.6014.132-a
Jon Lyall et al .: Suppression of Avian Influenza Transmission in Genetically Modified Chickens. In: Science. Volume 331, No. 6014, 2011. pp. 223-226, doi: 10.1126 / science.1198020 - ↑ Chickens soon to be flu-resistant? In: schweizerbauer.ch . January 29, 2019, accessed January 30, 2019 .