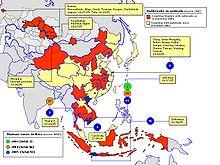
Distribution of H5N1
The spread of influenza A / H5N1 , the highly pathogenic agent of the so-called avian influenza H5N1 from Southeast Asia to Europe, has been closely followed and analyzed by both the World Health Organization (WHO) and the World Organization for Animal Health (OIE) and by the mass media since 1996 . It was (and is) the fear that the highly pathogenic variant of the virus Influenza A virus subtype H5N1 transition to a greater extent from person to person and so on a recent pandemic of genuine virus flu ( influenza could result).
1959–1996: the history
Waterfowl and poultry have long been known to be the natural reservoir of the less pathogenic variant of A / H5N1. The World Health Organization (WHO) is aware of the first reports of two purely local transitions of this variant from A / H5N1 to animal husbandry from 1959 (chickens in Scotland ) and 1991 (turkeys in England ). In wild birds before 1996 - also in Europe - only one non-pathogenic, i.e. non-disease-causing variant could be detected.
In the summer and early autumn of 1996, the first outbreak of a variant of A / H5N1 that was later classified as highly pathogenic occurred on a goose farm in the Guangdong province of the People's Republic of China , where 40 percent of the animals became ill. This was also the first ever evidence of a highly pathogenic variant of the H5 virus. This virus variant, with the full name Influenza A / Goose / Guangdong / 1/96 (H5N1) , was also found to be fatal to chickens in experiments immediately initiated. The hemagglutinin gene (H5) was found to be related to the H5N1 virus strains isolated in Hong Kong from 1997 onwards. A genetic analysis of the neuraminidase gene (N1), however, showed a greater similarity with an H7N1 virus isolated from a parrot in Northern Ireland in 1973 than with the H5N1 virus isolated later in Hong Kong. From these and other details, Chinese researchers concluded that there must have been a reassortment of the genes in H5N1 viruses in southern China in 1996 , which ultimately led to the repeated outbreaks among farmed poultry in 1997.
According to a report by researchers from Shantou University, between January 2004 and June 2005, 2 out of 100 marketed ducks and geese appeared to be healthy with A / H5N1. In the same study, it was shown that at that time there were already three geographic genetic variants of the virus in the Chinese provinces of Guangdong , Hunan and Yunnan ; From this, the researchers concluded that the viruses in this region had been spreading in domestic poultry for at least 10 years. The H5N1 variants that later circulated in Thailand and Vietnam were referred to as descendants from these three southern Chinese provinces.
1997–2004: first outbreaks of the highly pathogenic variant among breeding poultry
The highly pathogenic form of the virus A / H5N1 made a massive impact in poultry farms in Hong Kong and in the adjacent area of the People's Republic of China from spring 1997 , which led to chicken deaths there. After a boy was infected in May 1997 and another 18 people in November / December of that year, the Hong Kong authorities reacted on December 28, 1997 with an unprecedented mass killing of the entire chicken herd - around 1.5 million chickens were culled . This measure was rated as a success as no further cases were initially discovered. Only in 2003 were A / H5N1 diseases detected again. However, renewed mass killings in Hong Kong had no long-term success. In January 2004, an outbreak even broke out in a flock of chickens in the Tibetan capital Lhasa after infected chickens were transported there from the city of Lanzhou ( Gansu Province ) 1,500 km away .
Outbreaks were reported in 19 South Korean poultry flocks in December 2003 and March 2004 , in January 2004 in Thailand and Vietnam and in laying hens in Japan , in February 2004 in Indonesia , and repeatedly in summer 2004 in Malaysia .
At the beginning of 2004 and again in autumn 2004, several leopards, tigers and a large number of domestic cats that had been fed raw poultry meat were infected and killed at the Sri Racha Tiger Zoo in Thailand .
The reported outbreaks of H5N1 diseases among wild birds and in animal husbandry are listed on the website of the World Organization for Animal Health (OIE).
2005: massive expansion from Asia to Eastern Europe
Outbreaks of A / H5N1 among wild birds were first observed in 2005. Bird migrations were also blamed for allowing the disease to spread from Southeast Asia to Europe in 2005. However, there was no clear evidence for this thesis.
In poultry farming in Asia
2005:
On May 26, 2005, the journal Nature reported that officials in Indonesia had detected A / H5N1 in pigs and feared that the virus could have infected half of all pigs in some parts of the country without causing symptoms in them. Previously, there had already been reports from China of H5N1 finds in pigs .
On August 26, 2005, the Vietnamese authorities announced that three Owston civets had died of H5N1 in late June 2005 in Cuc Phuong National Park , south of Hanoi. The authorities said that other animals in the park, including a. Chickens and rats have been examined without any further cases of illness being found.
According to the Indonesian Ministry of Agriculture, A / H5N1 had spread to at least 22 of the country's 33 provinces by mid-September 2005. From the end of 2003 to mid-2005, more than 16 million head of poultry died of this virus or were emergency slaughtered in this country. A spokesman for the UN Food and Agriculture Organization (FAO) said on September 22, 2005 that the virus had become endemic in Indonesia and was spreading further. On September 21, 2005, the Indonesian Ministry of Health announced that H5N1 had been detected in 19 animals in the Ragunan Zoo in the capital Jakarta , including eagles and peacocks , and in several zoo employees. The zoo was then closed for three weeks.
On October 7, 2005, the Swiss Agricultural Information Service (LID) and later other sources reported another, particularly dramatic outbreak of A / H5N1 in Russia. A farm in the Kurgan region in southern Siberia with around 460,000 birds was affected .
According to an official document from the Chinese Ministry of Agriculture dated November 10, 2005, there was an A / H5N1 outbreak in northeast China's Liaoning Province as of November 6, with 300 poultry deaths recorded, 2.5 million animals preventive killed and 198 million animals vaccinated against H5N1 and H5N2. According to a WHO report, there were a total of 32 outbreaks of H5N1 in livestock farming in 12 Chinese provinces in 2005, as a result of which 24 million animals were killed and destroyed.
According to Science on October 21, 2005, more than 100 million breeding birds will have been killed as part of A / H5N1 containment measures.
Among wild birds in Asia
2005:
An A / H5N1 outbreak among migratory birds was first reported in May 2005 in Qinghai Province in northwest China . According to official information, around 6,000 dead migratory birds of various species were found there in the spring of 2005, 90 percent of which were bar geese . Immediately after the migratory bird outbreak, an outbreak was found in a poultry farm in the same Chinese province. Since the authorities prevented both Chinese and foreign scientists from investigating the outbreaks and the onward migration of the surviving migratory birds, it could not be determined whether the breeding poultry was infected by the migratory birds or, conversely, the migratory birds by the breeding poultry. Genetic studies of the viruses from Qinghai allow the conclusion that the migratory birds were infected with virus variants that were previously only known from southern China.
In May 2006, a report in the journal Nature announced that barge geese near Quinghai Lake had also been kept on farms since 2003. On the one hand, these breeding programs should help to increase the number of wild populations. On the other hand, long-term efforts were made to domesticate this species of geese. According to "Nature", this feeds the suspicion that the penetration of the highly pathogenic H5N1 variant into the wild population (and subsequently the large-scale spread to Siberia and Europe) could have occurred in the wild bird breeding station.
- At the end of July 2005, A / H5N1 was detected in poultry flocks in Siberia ( Novosibirsk region ) and Kazakhstan . Transmission by migratory birds as a result of the joint use of water by wild and farmed poultry was named as the route of infection.
- At the beginning of August 2005 around 100 ducks, geese and swans died on A / H5N1 on a remote lake in Mongolia (about 350 kilometers south of Lake Baikal ). According to Science of October 21, 2005, transmission through human influences (animal transport) is considered unlikely in this local outbreak.
- On August 16, 2005, the Russian Civil Protection Ministry announced in Moscow that the pathogen discovered in migratory birds in the city of Chelyabinsk in the Urals was A / H5N1. From China, the pathogen had spread via Novosibirsk , Tyumen , Omsk , Kurgan and Altai to Chelyabinsk, which is around 1,000 kilometers from Novosibirsk.
On the Arabian Peninsula
2005:
On November 10, 2005, the World Organization for Animal Health (OIE) from Kuwait was informed that a sample taken routinely from a flamingo on November 2 had tested positive for antibodies against H5N1 and that the animal had later been killed. The droppings of migratory birds were mentioned as a possible carrier of the infection. Repeated routine tests on other birds in Kuwait did not produce any additional positive results.
In Europe
2005:
The head of the German reference laboratory for influenza viruses in poultry at the Friedrich-Loeffler-Institut , Ortrud Werner, was quoted on September 15, 2005 by the dpa news agency as saying that the danger posed by migratory birds to introduce A / H5N1 to Western Europe was considered low by experts will be assessed. The spread of the influenza viruses to Russia was more likely through animal trade than through bird migration. For Western Europe, too, the greatest danger comes from the illegal import of infected or diseased animals. It is known from China and Mongolia that infected animals fall ill quickly and die promptly. The virus has not yet been detected in clinically healthy wild birds that are able to survive longer bird migration. However, this assessment contradicts the statements of Asian experts who have repeatedly linked the spread of the H5N1 virus in Southeast Asia to bird migration.
In fact, H5N1 viruses were not detected in migratory birds in Europe in 2005.
- On October 7, 2005 it became known from Romania that antibodies against the virus had been found in three domestic ducks from the town of Ceamurlia de Jos in the administrative district of Tulcea in the Danube Delta that had died in September. On October 15, 2005, A / H5N1 viruses were definitely detected by the EU reference laboratory in Weybridge near London . At a later in the northeast of the country in Vaslui county on the border with Moldova found dead heron , the virus was also detected on 27 October.
- On October 8, 2005, it became known that around 2,000 turkeys had died of A / H5N1 in northwestern Turkey, in the province of Balikesir . According to information provided by the EU on October 13, 2005, the virus was proven beyond doubt and a direct relationship to the virus found in Russia, Mongolia and China was established.
- On October 17, 2005, experts from the National and Kapodistrias University of Athens reported that a suspected case had been discovered on the island of Oinousses (East Aegean ) off Chios . Subsequent laboratory tests in the EU reference laboratory in Weybridge near London were able to rule out an H5N1 infection.
- According to the EU Commission on October 19, 2005, there was also an outbreak of A / H5N1 in the Russian region of Tula , around 300 kilometers south of Moscow . Subsequent analyzes showed the close relationship of the pathogen with the virus variants already known from Novosibirsk , Mongolia and the Chinese province of Qinghai . For a suspected case also reported from Macedonia (from the villages of Mogila and Germiyan near Bitola ), no confirmation for H5N1 was later known.
- On October 19, 2005, influenza viruses of type H5 were found in several dead wild swans in Croatia near the town of Zdenci. About 1500 animals (migratory birds) had perished on a fish pond, of which 15 perished there. On October 26, 2005, the EU reference laboratory in Weybridge near London confirmed that it was A / H5N1. Immediately after the suspicion became known, the EU had already imposed a preventive import ban on poultry from Croatia.
- On 23 October 2005, known that one of Suriname to the UK imported and there in a quarantine station dead parrot A / H5N1 was detected. The British chief veterinarian said that the animal was probably only infected with the virus in the station, where it was kept with birds from Taiwan . The EU immediately took this incident as an opportunity to temporarily ban the import of pet birds to Europe.
- On November 2, 2005, the Ministry of Agriculture announced in Zagreb that A / H5N1 had been detected in a swan shot in Croatia . According to its marker ring, this animal came from Hungary and was shot down in an area where eight other swans had previously tested positive for this virus. The Hungarian Ministry of Agriculture announced at the same time that all tests for A / H5N1 in their country had so far been negative.
- Since November 25, 2005, there have been repeated outbreaks of H5N1 in private chickens and geese in the Ukrainian Autonomous Republic of Crimea .
Transitions from H5N1 to Mammals
Mammals are less susceptible to the virus, but they can also become infected.
On May 26, 2005, for example, the journal Nature reported that officials in Indonesia had detected A / H5N1 in pigs and feared that the virus could have infected half of all pigs in some parts of the country without causing symptoms in them. Previously, there had already been reports from China of H5N1 finds in pigs .
The Dutch researcher Albert Osterhaus was in the time quoted on 19 January 2006 that A / H5N1 dogs, horses, pumas, tigers and leopards have infected in animal experiments and mice, ferrets , monkeys and cats.
Cats
2004–2006: In February 2004, the World Health Organization (WHO) first reported an H5N1 outbreak among cats. In Nakornpathom ( Indonesia ) 14 out of 15 cats died suddenly in a private household, and the virus was detectable in 2 out of 3 carcasses tested. One of the cats had previously eaten chicken on a farm that had an H5N1 outbreak. Also in 2004, the team led by Albert Osterhaus , a virologist at the Erasmus University in Rotterdam , showed that infected cats can transmit the virus to other cats. According to a report by New Scientist magazinein 2006, one in five cats in Java had antibodies to go A / H5N1, suggesting that these animals were or are infected but survived the infection. For this study, blood samples from 500 Javanese street cats were analyzed; H5N1 antibodies were detectable in around 100 animals. According to the head of the study, Chairul Anwar Nidom ( Airlangga University , Surabaya ), alikely far larger number of cats havedied of an H5N1 infection; Nidom had already detected A / H5N1 viruses in Indonesian domestic pigs in 2005. The investigations were initiated after aconspicuous number of dead cats in the vicinity of H5N1 outbreaks among poultryin Java and Bali . According to New Scientist ,Albert Osterhaus fearsthat cats could be an intermediate host for A / H5N1 in which the viruses gradually adapt to mammals and are then more easily transmitted to humans or even from human to human.
2004–2015: In 2004 it was reported from Thailand that several tigers , leopards and domestic catsin two zooshad died of A / H5N1 after eating infected poultry. The deaths at Suphanburi Zoo(two tigers, two leopards) have been attributed to severe pneumonia that occurred immediately after eating the infected poultry. Under similarly dramatic circumstances, 45 tigers died in another Thai zoo, and more than 100 more were euthanized. In 2015, several tigers were infected in the People's Republic of China.
2005: At the end of June 2005 in Vietnam, inthe Cuc Phuong National Park 120 km south of Hanoi , three crawling cats ( Hemigalus owstoni) died as a result of an H5N1 infection. In January 2006, a young cat caught in the vicinity of an H5N1 outbreak among poultry in Cipedang (West Java , Indonesia) alsotested positive for A / H5N1 by US doctors workingin Indonesia . This variant of the virus had genetic traits that were known from virus isolates from infected humans, but differed from those variants that had previously been isolated from birds.
2006:
After H5N1 outbreaks among poultry, it was reported from Iraq in early 2006 that cat deaths had occurred in the affected areas. Here, too, A / H5N1 could later be detected in two examined cats.
On March 2, 2006, the infection of a cat with the highly pathogenic Asia variant of A / H5N1 was detected for the first time in Europe. The animal was found dead on February 28 on the island of Rügen near the Wittower ferry. Two other H5N1 infections in dead cats from the same area became known on March 7, 2006. "An infection of humans, which cannot theoretically be excluded, can presumably only occur with very close contact with infected animals," said the President of the Friedrich Loeffler Institute (FLI) at the time.
On March 6, 2006, the Styrian Agricultural Council announced that the saliva of three cats in a Graz animal shelter had repeatedly been found positive in the laboratory of the Agency for Health and Food Safety (AGES). It was the animal shelter to which the first swan infected in Austria was brought and later the entire poultry population was killed. According to Health Minister Maria Rauch-Kallat, saliva samples were taken from 40 cats in a routine test in an enclosure adjacent to the enclosure of the infected birds. After a few days, however, the virus was not detectable in any of the 40 cats, i.e. none of the three previously infected cats. It remained unclear how the disappearance of the viruses can be explained.
The Dutch virologist Albert Osterhaus published a study at the beginning of 2006 in which cats were infected with A / H5N1. After their death it was found that almost all internal organs were infected by the virus, so that the liver and kidneys had also failed. It was also found that infected cats can excrete the virus to a significant extent both through the respiratory tract and in the faeces.
In an article for the journal Nature in April 2006 Albert Osterhaus pointed out that cats should not be underestimated as possible carriers of A / H5N1 viruses. His research group rated the risk that the A / H5N1 viruses in cats could develop the ability to effectively spread from mammal to mammal as relatively high; this would increase the risk of a pandemic influenza among humans. An occasional transmission from cats to humans cannot be ruled out even now. In addition, laboratory experiments have shown that cats after A / H5N1 infection developed pneumonia in a manner very similar to that in humans (this is the main cause of death in infected people) and therefore represent the best animal model for studying the disease.
2012: Free roaming cats died in Israel in 2012 after eating carcasses of turkeys that died of A / H5N1.
dogs
2006: In the journal Nature on February 16, 2006, a long-known study by the Thai National Institute for Animal Health was reported, according to which antibodies against A / H5N1 were found in 160 of 629 tested street dogs with normal health and in 8 of 111 domestic cats. This indicated an existing or at least pre-existing infection with the virus. So far, however, it has not been possible to specifically infect dogs with A / H5N1 in experiments. There was also no evidence that dogs contract the virus or excrete viruses and thus contribute to their spread. A risk to humans from dogs was therefore classified by the experts as extremely unlikely. On March 16, 2006, however, the news agency afp reportedthat authorities from Baku ( Azerbaijan ) had found “a variant of a bird flu pathogen” in a stray dog. According to a report in New Scientist magazine,H5N1-infected dogs have also been discoveredin Bali , according to official Indonesian information.
Beech marten
2006: On March 9, 2006, the Friedrich Loeffler Institute announced that A / H5N1 hadinfecteda stone marten . The animal wasfound aliveon March 2, 2006 on the island of Rügen near the Wittower ferry near Schaprode , but with clinical symptoms and was later euthanized. It was the first animal of its kind in the world to be found to be infected with H5N1.
Since 2006: spread in Western Europe and Africa
2006:
In 2006, H5N1 spread at a sensational rate in Southeast Asia, the Middle East, Europe and Africa. In the individual countries concerned, similar, but in some cases very different, measures were often prescribed:
- China: Compulsory cage in Anhui province , ban on "backyard farms " in Hong Kong
- Germany: compulsory stable
- France: Stable compulsory with exceptions
- Italy: Free range poultry must be kept under wire mesh
- Canada: Stable compulsory in the province of Québec
- Croatia: Stable compulsory during bird migration
- Netherlands: Stable compulsory with exceptions
- Nigeria: Ban on "backyard keeping" in Abuja
- Norway: Stable compulsory in eight districts in the south of the country
- Austria: Stable compulsory from October to December and unlimited in the region where swans infected with H5N1 were found
- Sweden: compulsory stable
- Switzerland: Poultry must be kept covered and fenced
- Slovenia: compulsory stable
- Spain: compulsory stable (in the vicinity of the only place of discovery so far, as of July 7, 2006); stricter controls in a 10 km area around the site
- Thailand: Restrictions on the free range of ducks, ban on live poultry markets in Bangkok , increased collectivization of small poultry farms in some provinces
- Ukraine: Prohibition of sales of poultry products produced in private households in Crimea
- Vietnam: Ban on poultry farming in cities
2007:
The virus was detected in a total of 31 countries - between Japan and Great Britain - in 2007, including eight countries for the first time, most frequently in Indonesia and Nigeria. In 2008 there was evidence in Egypt, Bangladesh, Benin, People's Republic of China and Hong Kong, Germany, Great Britain, India, Iran, Israel, Japan, Cambodia, South Korea, Laos, Myanmar, Nigeria, Pakistan, Poland, Romania, Russia, Saudi Arabia, Switzerland, Thailand, Togo, Turkey, Ukraine and Vietnam.
South East Asia
2006:
New outbreaks of A / H5N1 have been repeatedly reported to the World Organization for Animal Health (OIE) from both Thailand, Vietnam and Cambodia.
- On January 1, 2006, an outbreak of A / H5N1 was discovered among quails in Guiyang County in Guizhou Province (People's Republic of China) , which according to official reports killed 16,000 animals; a further 42,000 quails were killed as a precaution.
- On January 10, was in Hong Kong in Tai Po a wild Oriental Magpie-Robin (Copsychus saularis) found dead, an A / H5N1 strain was detected in a few days later, which was also known from southern China, South Korea and Japan.
- An outbreak of A / H5N1 was reported again from the People's Republic of China on February 2, 2006, from the town of Yijing near the city of Yangquan in Shanxi Province . 15,000 chickens perished there, more than 60,000 chickens of the same herd; 125,000 animals in the neighborhood were killed as a precaution.
- On February 6, 2006, an outbreak of A / H5N1 among chickens was also known in Malaysia , the Ministry of Agriculture in Kuala Lumpur informed the World Organization for Animal Health on February 23.
- On February 23, 2006, the animal disease laboratory in the Indian city of Bhopal announced that more than 40,000 chickens had died of A / H5N1 in Navapur in the western Indian state of Maharashtra as of January 27. According to official information to the OIE, more than 400,000 animals were prophylactically killed there and after a simultaneous outbreak in Gujarat state . H5N1 outbreaks occurred repeatedly in March and April in dozens of locations in the states of Maharashtra and Madhya Pradesh , as a result of which more than 600,000 other animals died or were killed.
- On February 23, 2006, an outbreak of H5N1 viruses in poultry farming was also known from Abbottabad and Charsadda in the northwestern border province in Pakistan . 3,500 animals died there, and more than 20,000 other animals were killed as a precaution. After July 1, 2006, there was another outbreak in poultry holdings in Islamabad Province , which officials attributed to wild bird transmission; 3.5 million animals were vaccinated against influenza viruses.
- On March 8, 2006, A / H5N1 was detected in a poultry farm in Mandalayn in Myanmar (Burma) . On March 20, 2006, the Afghan Ministry of Agriculture reported to the OIE that since March 2, 2006, more than ten H5N1 outbreaks had been detected in five provinces and confirmed by the reference laboratory in Padua.
- After a break of almost three years, several new outbreaks in animal husbandry were also reported from South Korea at the end of November 2006, with the infection area there being under the migration path of millions of birds from Russia, Kazakhstan and Mongolia, which were moving south at the time.
2007:
- On January 10, 2007, for the first time since the beginning of 2004, an H5N1 outbreak was also reported from Japan (from Kiyotake, Miyazaki Prefecture ) in a 12,000-animal poultry facility and in April 2008 in three swans (Towada Lake in Akita Prefecture). On February 3, 2007, an outbreak was reported in Vientiane ( Laos ) and, after February 5, 2007, for the first time in Dhaka ( Bangladesh ); a total of 35,800 fell victim to this. A similar number of breeding animals killed was reported from Myanmar in October 2007.
2009-2013:
In Nepal , the virus was first detected in January 2009, in 2013 about 60,000 poultry birds died in Nepal, more than 100,000 were killed. In April 2013, 164,000 ducks died in connection with H5N1 infections in North Korea .
Middle East, Turkey, Europe
2006:
- At the beginning of January 2006, a major outbreak of A / H5N1 among domestic poultry in the eastern Turkish province of Van became known, which the authorities apparently had not detected in time. In any case, in the village of Dogubeyazit, the pathogen spread to some residents and caused several deaths. By the end of January, outbreaks of H5N1 among chickens and turkeys were also discovered in western Turkey and in various other regions of the country. Official Turkish information to the World Organization for Animal Health revealed H5N1 cases and a. Discovered near Adıyaman , Diyarbakir , Ankara , Elazığ , Izmir , Mardin , Malatya , Tokat , Trabzon and Samsun .
- On January 4, 2006, a further seven foci of A / H5N1 infection in poultry in Romania were discovered after the EU reference laboratory in Weybridge examined samples. The affected villages were around 150 km northeast of Bucharest near the Carpathian knee. In the following weeks, new outbreaks from Romania were reported again and again, in mid-May press reports mentioned a total of 65 sources of infection in the Danube Delta, on the Carpathian Bend and in the southern Romanian lowlands. Since the outbreak of the A / H5N1 virus in the Danube Delta at the beginning of October 2005, the animal disease has spread approx. 400 km to the west. In mid-May 2006 alone, several hundred thousand breeding animals were killed as a preventive measure after an outbreak in Codlea . In mid-May 2006, the head of the National Office for Animal Health and his deputy were dismissed due to insufficient efforts to contain the disease.
- On January 29, 2006, the EU Commission announced that H5N1 infections had been found in chickens and turkeys in Turkish-controlled Northern Cyprus , near the port city of Famagusta , and confirmed in the EU reference laboratory in Weybridge .
- On February 3, the World Organization for Animal Health was informed by the Iraqi Ministry of Agriculture that there had been repeated H5 outbreaks in northern Iraq since January 18, killing several hundred privately kept animals (chickens, geese, turkeys, ducks). On February 7, an H5 outbreak among pigeons was serologically confirmed by a laboratory in Baghdad .
- On February 10, the Ministry of Health of Azerbaijan announced that the EU reference laboratory in Weybridge, UK, had confirmed that after January 29, near the Apsheron peninsula on the Caspian Sea (near Baku), migratory birds of various species were dead in the water A / H5N1 were discovered. As a result of several H5N1 outbreaks in large poultry flocks, 300,000 breeding animals were killed in the Khyzy and Biljasuvar regions after February 22, according to official data from the Baku Ministry of Agriculture.
- On February 11, 2006, the Reuters news agency reported that the Italian health department and authorities from Greece had reported suspected H5N1 cases in southern Italy and northern Greece. In Italy, the virus was detected in some of a total of around 70 dead mute swans in Calabria , Puglia and Sicily (found on February 1), and in Greece in three swans near the port city of Thessaloniki , which had already been found on January 30. H5N1 was also detected in a red-necked goose (Branta ruficollis) in the region of Sterea Hellas . At the same time there were reports of new H5N1 cases in Romania near the Bulgarian border and the discovery of an H5N1-infected mute swan near the Romanian border in Bulgaria . This swan was spotted on the Danube on January 31, but the incident was not reported to the World Organization for Animal Health until February 12.
- On February 12, according to the EU Commission, H5 viruses were detected in a mute swan that had died near Maribor and in a gray heron in Slovenia . A special laboratory in Padua confirmed on February 16 that the swan was H5N1. As early as February 15, the Slovenian Ministry of Agriculture declared the entire national territory to be a bird flu risk zone.
- On February 14, the Iranian veterinary authority announced the first cases of H5N1 infection in that country. An official statement said laboratory results from abroad had confirmed that more than 150 mute swans found dead as of February 2 had died of H5N1 viruses. The swans came from wetlands on the northern Iranian coast, near the port of Bandar-e Ansali on the Caspian Sea , where many migratory birds winter. As a preventive measure, more than 40,000 poultry and wild birds were killed in the two affected areas.
- On February 15, 2006, 11 dead mute swans were reported from Hungary , in which an H5N1 infection was detected a few days later. The animals were discovered 60 kilometers northwest of the capital Budapest on the partially frozen Danube . At the same time, new, secure records of wild birds from the Romanian Danube Delta and from a chicken farm in the Russian republic of Dagestan , where more than 500,000 animals were emergency slaughtered in Machachkala, were reported. On February 16, 30 swans from Croatia and Bosnia-Herzegovina (Lake Plivsko) were also reported to have died with the H5 influenza virus infestation detected in rapid tests. In Albania , 60 domestic chickens died of H5N1 in the Vlora district . The animals found in Bosnia-Herzegovina came from a troop of around 15 swans which, according to the State Veterinary Office, had recently immigrated. On February 23, the Slovak Ministry of Agriculture announced that H5N1 had been detected in a falcon and a grebes near the capital, Bratislava . Both animals were found dead near or in the Danube on February 21. At the beginning of March, several dead mute swans also tested positive for A / H5N1 in Poland . Dead, H5N1-infected mute swans were also found on the banks of the Drina in Serbia ( Zapadna Bačka and Zlatibor district ) in late February and early March .
- On 17 February 2006 was announced by the French Ministry of Agriculture, one on February 13 in the center of the country (in the town of Joyeux in the Ain department ) together with 6 other ducks birds found dead Pochard was "very likely" died of H5N1. Genetic analyzes showed that 98.8 percent of the viruses are identical to the H5N1 viruses known from Asia. A large observation zone was set up around the site, including the town of Versailleux , where 10,500 young (56 days old) turkeys were killed after February 23, after the farm owner had previously discovered 400 dead animals. Here, too, the H5N1 variant known from Qinghai could later be detected. Further H5N1 evidence in the Ain department concerned several wild swans, ducks, geese and a common buzzard on the following days.
- On February 19, further wild birds were discovered in Sicily and Umbria in which the highly pathogenic form of A / H5N1 could be detected. Mute swans were affected again , but also purple hens , buzzards and mallards .
- On March 15, the EU reference laboratory confirmed the first detection of A / H5N1 in Sweden , in a mallard that was kept as ornamental poultry along with other birds on a farm near Oskarshamn on the Swedish Baltic coast. February preventive (i.e. symptomless) had been examined. On the same day, the Danish State Veterinary Office reported an H5 detection to the OIE, namely in a common buzzard found dead on March 12 in Storstrøms ( South Zealand ).
- On March 17, the Israeli Ministry of Agriculture reported to the OIE that in two turkey farms near Be'er Scheva as well as in two other turkey farms near Jerusalem and Ashkelon almost 12,000 animals died as a result of an H5N1 infection and almost 60,000 others were killed as a preventive measure were. Shortly thereafter, there were several outbreaks in the Palestinian Territories - more than 40,000 animals were killed in the Gaza area - and on March 23, for the first time, in Kofranja , Jordan ; 18,000 animals were killed on one farm.
- On March 30, a dead whooper swan was discovered near Anstruther in Scotland , in which the highly pathogenic H5N1 variant was reliably detected for the first time in Great Britain a few days later. As a preventive measure, the poultry in the region were vaccinated.
- On May 16, the first H5N1 outbreak in Denmark was discovered in a poultry population of around 100 on the Baltic island of Funen .
- On 30 June 2006, in Salburúa wetland of the Spanish province of Alava a great crested grebe found dead in the July 7, a secured H5N1 Detection was.
2007:
- For the first time since August 2006, A / H5N1 was detected in an EU country in early 2007, namely on a Hungarian goose farm, as the EU Commission announced on January 30, 2007. As a precaution, around 3,300 geese were culled there to prevent the pathogen from spreading.
- On February 9, 2007, the BBC reported: The H5N1 bird flu outbreak in a British poultry farm in Suffolk is believed to be due to the import of contaminated turkey meat from Hungary.
- On December 4, 2007, the Romanian newspaper Jurnalul National reported : H5N1 bird flu had again been reported on a farm in the village of Murighiol in the Danube Delta. The entire poultry population - 76 animals - was killed immediately.
- On December 7, British authorities reported the second case of H5N1 avian flu in the east of England within a week. The H5N1 virus was in turkeys on a farm on the border between Norfolk and Suffolk proven. The previous week the killing of more than 6,000 animals on the infested farm in Diss in Norfolk had already been ordered and, to be on the safe side, more than 20,000 other animals from four neighboring farms had been culled. The H5N1 avian flu had already broken out in Suffolk in February 2007, which is why around 159,000 turkeys were killed in a farm in Holton as a precautionary measure.
- On December 9, 2007, A / H5N1 was detected on a chicken farm in the municipality of Bieżuń, northwest of Warsaw. About 110,000 laying hens were killed as a precaution. In addition, 100,000 eggs were seized. However, some products have already reached stores. This was the fourth major case of bird flu on a Polish poultry farm since December 2006.
After 2007: There were also isolated outbreaks of A / H5N1 in Europe in the following years.
Austria
2006:
On February 14, 2006, a representative of the Food Safety Authority in Vienna announced evidence of an H5 infection in two swans who had been found dead in the Austrian community of Mellach (near the market town of Wildon ) in the south of the provincial capital of Graz . The following day, the official Austrian Agency for Health and Food Safety (AGES) announced that it had already definitively proven the genetic material of the H5N1 virus on February 13th (the day of the discovery). The diagnosis was confirmed on February 18 by the EU reference laboratory in Weybridge , UK .
On February 18, the suspicion of an H5N1 infection was confirmed in a swan in Vienna . The animal was found dead on February 14 on the Old Danube in the area of the so-called water park. Also on February 18, most of the regions in Styria and large areas in Carinthia and Burgenland were declared to be H5N1 risk zones , as well as a general stable requirement for all of Austria until the end of April. In Styria, the virus was confirmed on the fourth swan. All four swans came from the Mellach community.
On February 21, a total of five positive results were confirmed in Styria. Another 100 dead birds were sent to the AGES laboratory in Mödling . In Tyrol , three dead ducks, a cormorant and a swan were sent to the AGES laboratory on suspicion of H5N1 bird flu.
A protection zone was set up in Graz on February 22nd . Of 130 dead birds sent for examination in Styria, the infection has already been confirmed in eleven cases. The results were negative in 30 cases, the remaining results are still pending. The all-clear has come from Vienna, Tyrol and Carinthia. There was a negative finding in twelve animals examined. A result from Vienna is still pending. On March 6, there are 28 confirmed cases in Styria. H5N1 was temporarily found in three cats.
On March 3, AGES diagnosed a wild duck from the Pernegg reservoir in Styria with an H5N1 virus. The AGES also found the virus in five water birds from the Bregenz district . A protection zone was established in both cases.
A total of 124 “positive cases and suspected cases” in wild birds were reported by AGES with a reference date of April 26th, ducks and swans in particular were affected.
2006–2008: The World Organization for Animal Health (OIE) published only one official H5N1 notification - submitted on February 20, 2006 - by the end of 2008 for Austria.
Germany
2006:
On the evening of February 14, 2006 it became known that two mute swans found dead near Wiek (Rügen) were suspected of having H5N1 based on a genetic analysis; the animals had already been found on February 8th. This suspicion was officially confirmed the following morning by the head of the Robert Koch Institute . In the early afternoon, the ddp agency reported the discovery of more than 100 freshly dead swans near the Wittower ferry on Rügen , citing the district office in Bergen . At the same time it became known that H5N1 had also been found in a hawk , which had also been found on February 8 by a hunter near Dranske . Dead wild birds had been repeatedly examined in the previous weeks without H5N1 being found in them.
On February 15, 2006, the Friedrich Loeffler Institute announced that the H5N1 / Asia viruses found on Rügen were closely related to virus variants that had been detected in Mongolia and on Lake Qinghai in western China in 2005 . On the evening of February 16, 2006, the Federal Ministry of Agriculture announced ten more H5N1 finds on Rügen, namely six mute swans, three whooper swans (which are considered migratory birds) and a Canada goose . One of the whooper swans was ringed in Latvia . On the following days, the detected H5N1 infections increased to more than 100, including cormorants and a common buzzard .
In accordance with the provisions of the Avian Influenza Ordinance , restricted areas were set up in the vicinity of discovery sites , and stalls were compulsory and poultry were prohibited from transporting; the entire island was declared an observation area. The nationwide stable requirement for poultry came into force on February 17, 2006 due to an emergency ordinance of the BMELV .
On February 19, at the instruction of the responsible minister Till Backhaus, the first herds were culled in farms that are close to wild bird colonies, although, according to Chancellor Merkel , no diseases have been observed in farm animals. This was criticized by the German Animal Welfare Association as "actionism" that happens for political reasons; the Friedrich Loeffler Institute's risk assessment has not yet been completed. Furthermore, two H5N1 records were found in a common buzzard from the Ostvorpommern district and in a herring gull from the Nordvorpommern district .
Because of the animal disease, the Rügen district declared a disaster on February 19. This was announced the next day in the districts of Nordvorpommern and Ostvorpommern. In order to fight the epidemic, especially to collect dead animals and to disinfect shoes and vehicles, soldiers of the German Armed Forces were then deployed alongside volunteer forces, for example fire brigades and disaster relief workers.
On February 23, a dead tufted duck that had already been found on February 17 on the island of Walfisch , about five kilometers from the city of Wismar in the north-west Mecklenburg district , tested positive for A / H5N1. With this find, the number of affected districts in Mecklenburg-Western Pomerania increased to four, and it is also the westernmost H5N1 evidence to date.

On February 24, further H5N1 cases became known: in mallards in Schleswig-Holstein in the Ostholstein district near Neustadt and in Timmendorfer Strand as well as for the first time in southern Germany ( Baden-Württemberg ) in a pochard in Überlingen on Lake Constance . The virus type H5N1 / Asia was later detected in the discovery from Überlingen. On February 26, the responsible state minister announced that in the district of Konstanz , too , a duck was found in the communities of Singen and Öhningen , in which the suspicion of H5N1 / Asia was later confirmed. On the following days, further H5N1 infections became known in Schleswig-Holstein, including a. with one dead swan each on the island of Fehmarn (Ostholstein district) and near Hohwacht ( Plön district ) and a mountain duck from the vicinity of Kollmar ( Steinburg district ).
On February 25, it was announced that H5N1 had been detected in a mute swan and a wild duck in the Uckermark district in Brandenburg . On March 3, the Brandenburg Ministry of Agriculture announced that A / H5N1 had been found on a coot found on a lake plot in Wandlitz .
Also on February 25, according to a witness , a gray goose fell “dead from the sky” and hit a field near the village of Düshorn in the Heidekreis district ( Lower Saxony ). A week later, on March 4th, the Lower Saxony Ministry of Agriculture announced that A / H5N1 had been detected in the dead animal; this affected the sixth federal state in Germany. The district set up a restricted area with a three-kilometer radius and an observation area with a ten-kilometer radius around the site. The observation area included u. a. the places Walsrode , Bad Fallingbostel and Bomlitz . Both in the restricted area and in the observation area, dog and cat owners had to ensure that their animals could not roam freely.
On February 28, 2006, A / H5N1 was detected in a cat on Rügen (details see above ). On the same day, the Bavarian State Ministry for the Environment, Health and Consumer Protection announced that A / H5N1 had also been detected in two wild birds in Upper Bavaria . Both the mute swan from the Schwabstadl community in the Landsberg am Lech district and the mallard from the Sachsenkam community in the Bad Tölz district were found dead on February 20. On the following days, further H5N1 infections were detected in wild animals in Bavaria. a. with a mute swan from the Swabian Schmiechen , with two ducks from Lindau on Lake Constance and with a wild duck found dead in the courtyard of the Straubing prison .
According to information from the Baden-Württemberg Ministry of Agriculture in Mannheim, A / H5N1 was found in a dead wild duck on March 3, 2006 . Immediately afterwards, a local transport stop for birds and hatching eggs was ordered, which also extends to the Hessian municipality of Viernheim and parts of Lampertheim (both in the Bergstrasse district ). On March 4, a dead wild bird was found on the former Great Lakes site in Constance that tested positive for A / H5N1. After the confirmed test on March 13, a 3 km exclusion zone was immediately set up.
On March 24th, the discovery of a dead wild bird infected with the H5N1 virus was announced in Nuremberg . Here, too, a restricted area and an observation area were set up.
Also on March 24th, the Berlin Senate Department for Health announced that a dead buzzard with the H5N1 virus had been found in the Marzahn-Hellersdorf district . A restricted area with a radius of three kilometers and an observation area with a radius of ten kilometers were immediately set up. A day later it was announced that the origin of the buzzard could not be determined due to a mishap with the labeling. The restricted area was lifted and the entire urban area of Berlin became an observation area.
On April 5, 2006, the Saxon Ministry of Social Affairs in Dresden informed that the highly pathogenic variant of the H5N1 virus had been detected by the Friedrich Loeffler Institute on a poultry farm in Wermsdorf in the Muldental district . It is the first occurrence of A5 / H5N1 on a German poultry farm. 14,000 turkeys, geese and chickens were killed instantly.
Thereafter, new H5N1 cases outside of the immediately affected areas were hardly reported by the news agencies. Nonetheless, individual wild birds were repeatedly found in April and May 2006: in Brandenburg in the Märkisch-Oderland district and in the Dahme-Spreewald district ; in Mecklenburg-Western Pomerania in the district of Ostvorpommern ; in Schleswig-Holstein in the districts of Ostholstein , Plön , Rendsburg-Eckernförde and Steinburg ; in Baden-Württemberg in the Lake Constance district , in Constance and in Sigmaringen ; in Bavaria in the districts of Deggendorf , Dillingen , Donau-Ries , Fürstenfeldbruck , Kelheim , Landsberg am Lech , Lindau am Bodensee , Neu-Ulm , Rosenheim , Straubing-Bogen and Weißenburg-Gunzenhausen as well as in Straubing .
A black swan was registered in August as the 344th and last reported death of the H5N1 virus in the Dresden Zoo in 2006.
2007:
A few infections among wild and domestic poultry did not become known again until summer 2007.
At the end of August there was an H5N1 outbreak in a large duck fattening farm near Erlangen , so that all 160,000 animals were killed. This was the largest preventive killing of farm animals that had ever occurred in Germany. After another suspected case in Schwandorf , Upper Palatinate , around 205,000 ducks were killed as a precaution at the beginning of September.
On December 16, the State Ministry of Agriculture in Brandenburg reported that the H5N1 virus had reappeared in a private chicken coop in the Oberhavel district; eleven animals were killed. How the chickens got infected is unclear. There are two large poultry farms in the observation area: a broiler fattening facility consisting of ten halls with around 220,000 animals and a facility with 24,000 laying hens.
2008-2010:
Another case became known in Germany on October 9, 2008 after A / H5N1 had been detected in a duck on a poultry farm in Saxony. At the beginning of March 2009, the virus was detected in 39 wild ducks at Lake Starnberg .
On November 12, 2010, A / H5N1 was found in a poultry farm in Mecklenburg-Western Pomerania. As the Parchim district announced, 17,000 ducks and geese were killed as a precaution. This was the first major bird flu case in Germany in 2010.
Switzerland
2006: In the first week of March 2006 were Steckborn in the canton of Thurgau a Pochard and Feuerthalen in canton Zurich a coot found, the infected H5N1 by the competent Swiss authorities in mid-March as were reported to the World Organization for Animal Health. Between March 6 and 10,some H5N1-infected wild birds (including the little grebe , tufted duck and pochard) were foundnear Schaffhausen , Dörflingen and Feuerthalen.
2008: An outbreak among wild birdswas onlyreported to the OIEfrom Lucerne in the spring of 2008.
Africa
2006:
On February 8, 2006, the World Organization for Animal Health (OIE) announced in Paris that there had been an outbreak of A / H5N1 in a large battery of laying hens in the Nigerian city of Jaji in the state of Kaduna since January 10, 2006 . By the end of June, H5N1 infections were known from 14 of the 31 Nigerian states. In the journal Nature , a Luxembourg research group came to the conclusion, after genetic analyzes, that A / H5N1 had been introduced into Nigeria at least three times independently of one another. Southern Russia and Northern Europe were identified as the regions of origin of the virus strains. Nigerian poultry farms import hatching eggs from abroad, including Turkey , according to BirdLife . Poultry farming is the second most important economic factor in the country, but there are no import controls.
In a statement published on the WHO website on February 9, 2006, the director of the World Health Organization expressed extreme concern that transitions from A / H5N1 to people in Nigeria and its neighboring countries were not recognized or recognized too late, and thus possibly also an increased transition could initially go undetected from person to person: “The African health systems are already struggling to cope with the illnesses of children and adults from HIV / AIDS , tuberculosis , malaria , respiratory diseases and other infections. H5N1 diseases in humans may therefore be difficult to distinguish from other diseases. We also don't know what effects it will have if many people, who are already immunocompromised and vulnerable to health, are also exposed to the pathogens of avian influenza. "
- On February 28, it was officially announced from Niger that an H5N1 outbreak among "traditionally kept poultry" had occurred in the Zinder region from February 13, affecting 20,000 animals. Another outbreak occurred in the Maradi region in April .
- On February 18, the Egyptian Ministry of Agriculture informed the World Organization for Animal Health that H5N1 had been detected in privately kept animals by two national research institutions in the greater Cairo area and in the regions of Giza, Menia, Quena and Qualiubia. In the months that followed, until the autumn, individual animals kept in private backyards were repeatedly discovered, in which the Central Laboratory for Veterinary Inspection of Poultry Production detected H5N1.
- On March 12, the responsible ministry of the West African state of Cameroon reported to the OIE that A / H5N1 had already performed in this state on February 21. The Pasteur Institute in Paris detected the virus in a group of 50 breeding ducks from the city of Maroua (northern Cameroon).
- From March 25th, according to the first official reports, there were several H5N1 outbreaks in Sudan near Khartoum , Gezira , Atbara and Juba , both in larger poultry flocks and in private owners, in which more than 60,000 animals died according to official reports to the OIE. It was later revealed that H5N1 had already been diagnosed on a farm in Atbara on February 20, 2006. After more than 900,000 animals had been vaccinated in the affected areas, there were no new H5N1 outbreaks in Sudan in 2006, according to official reports.
- On April 3, 2006, the responsible ministry of Burkina Faso reported to the OIE that an H5N1 outbreak had occurred in guinea fowl in the province of Kadiogo from March 1 , which was confirmed by the reference laboratory in Padua. Additional outbreaks were reported in Houet and Sanguié provinces in May .
- On April 6, an H5N1 outbreak also occurred in Djibouti for the first time , in a small poultry farm near the capital near Boulaos . However, the incident was only reported to the OIE on May 27th. On April 23, H5N1 had become known in humans from the country.
- On April 25, the Ministry of Livestock Production of the Ivory Coast reported to the OIE that from March 30, several H5N1 outbreaks had occurred among private poultry in the vicinity of the capital Abidjan . Several thousand chickens and ducks as well as a sparrowhawk (épervier) were affected .
2006–2008: By the end of 2008, the OIE had reports of repeated H5N1 infections from Nigeria , Niger , Egypt , Cameroon , Sudan , Burkina Faso , Djibouti , Ivory Coast , Ghana , Togo and Benin .
North America
2015: The first highly pathogenic variant of A / H5N1detectedin North America contains a previously unknown reassortment and was found in a teal . There is evidence that the virus had contact with viruses of the A / H5N8 subtype, as had recently been found in a gyrfalcon kept nearby. Virus detection from a wigeon also showed reassortment through contact of subtypes A / H5N2 and A / H5N1 . In Canada , H1 / N1 has been found in chickens.
Transitions from A / H5N1 to humans
The known diseases in humans are registered by the World Health Organization (WHO) and - after the reports from the member countries of the WHO have been checked in trusted laboratories of the WHO - published on the WHO website,
Before 2004: The first proven transmissions from H5N1 to humans wereidentifiedas individual cases by the relevant national authorities as well as by the World Health Organization , which means that the H5N1 viruses always passed directly from animals to humans. The first death from H5N1 infection occurred on May 21, 1997, five days after a three-year-old boy wasadmitted to the intensive care unit of a Hong Kong hospitalwith a diagnosis of Reye's syndrome , acute influenza pneumonia, and dyspnea.
2004: The first suspected cases of person-to-person transitions became known in 2004. However, these first suspected cases were not sufficiently analyzed by the health authorities to allow reliable conclusions to be drawn about the chain of infection.
Suspected human-to-human transitions
2004-2005:
The first suspected case was reported from the hospital in the South Vietnamese city of Cần Thơ . A 19-year-old man and his 22-year-old cousin died there on July 30, 2004. The 19-year-old man's 25-year-old sister developed flu-like symptoms a little later, tested positive for H5N1 and eventually died too. Her two relatives were not tested, so the official statements only mentioned one confirmed death.
The second suspected case became known in September 2004 from the north of Thailand . There, an eleven-year-old girl had developed flu-like symptoms that were treated as dengue fever . Her aunt, with whom the girl was living at the time, also developed similar symptoms shortly afterwards. The child's mother traveled north from Bangkok to visit her daughter in the hospital and shortly thereafter began showing symptoms similar to those of her two relatives. Daughter and mother died, the third person survived. However, tests were only carried out on adults, so the official statements only spoke of one confirmed death, one survivor and a suspected human-to-human transmission.
At the end of December 2004, a 47-year-old man in Hanoi fell ill with H5N1 and at the beginning of January 2005 his 42-year-old brother. Investigations to prove human-to-human transmission remained inconclusive. A common source of infection was also not known. In January 2005, the death delayed by a few days as a result of an H5N1 infection of a 35-year-old woman and her 13-year-old daughter and a slightly delayed H5N1 infection in a 17-year-old adolescent and his 22-year-old sister remained unreliable Vietnamese district of Phuoc Long , as a result of which the boy died. The suspected brother-to-sister transmission, which became known from Cambodia in January 2005 , also remained unresolved. First a 14-year-old boy and shortly afterwards his 25-year-old sister died of an H5N1 infection.
In a similar form, multiple illnesses among relatives became known again and again in the following months, each of which occurred with a time delay, so that a common source of infection could not explain the occurrence with sufficient certainty.
From Indonesia in July 2005, three deaths were reported (one man and two of his children) who do not have close contact with infected poultry. A team of experts from the World Health Organization found only one ornamental bird in the family's neighborhood, in whose faeces A / H5N1 could be detected. It remained unclear whether this was the source of the infection and how the infection spread to the three members of the family.
2007–2008: From Jiangsu , People's Republic of China , it was announced by the WHO at the beginning of December 2007 that a 24-year-old man died of an H5N1 infection who last visited a poultry market six days before the symptoms appeared, but had no contact there had clearly diseased poultry. A few days after his death, his 52-year-old father fell ill with H5N1. In April 2008, Chinese researchers reported that a detailed genetic comparison of the viruses of father and son had shown that the genetic makeup of the viruses - apart from a single small change in the sequence of the genetic components - was identical. In a publication in The Lancet , the most likely explanation was that the virus was transmitted from son to father.
A chain transfer in Indonesia
2006:
On May 4, 2006, according to WHO information , a 37-year-old woman died in the Indonesian village of Kubu Sembelang ( Karo district , North Sumatra ) Animals had died. However, no H5N1 virus could be detected in either the remaining chickens or the faeces, and no H5N1 test was carried out on the woman herself. Shortly afterwards, her two young sons (May 9th, May 12th), her sister (May 10th) and their baby (May 14th) and a ten-year-old nephew (May 13th) died as a result of an H5N1 infection. The father of the nephew, a brother of the woman who was initially ill, died on May 22nd, her second brother fell ill, but survived the infection. 54 relatives and contact persons of the family were then quarantined by the local health authorities and treated with the antiviral drug oseltamivir as a preventative measure . Furthermore, all 400 households in the village were kept under observation for three weeks in order to be able to immediately isolate any further patients with new febrile illnesses. With no cases outside the family, the WHO stated on May 31 that the pandemic phase 3 could be maintained unchanged. In the sick, a higher viral load in the throat and nose than in previous cases in Indonesia was proven.
The transition of the infection from the ten-year-old boy to the last brother of the woman who was initially ill was identified by the WHO in mid-June 2006 as the first really confirmed case of human-to-human transmission. This is also the first documented suspected case of chain transmission from the initially ill woman to the child (her nephew) and then to the child's father (her brother).
What is remarkable about this family tragedy is that a precise analysis of the viral RNA revealed a relationship between the date of death and the mutation rate: the later death occurred, the more mutations were detectable. Compared to the first death in this family, the RNA of the man who died last had 20 mutations, although their biological significance is still unclear.
The official case numbers
1997 and from 2003: The development of the number of cases since 2003 is updated daily by the World Health Organization on its website. Not included in this statistic is an outbreak in Hong Kong in 1997when 18 people were infected with A / H5N1 and 6 of them died. The first fatality in May 1997 was a three-year-old boy who had developed an acute respiratory disease known as Reye's syndrome . Obviously, those people who dealt with live poultry in a confined space were at risk of infection.
People's Republic of China
2003–2006: Official reports of illnesses and deathsfrom the People's Republic of China have only been available since mid-November 2005. a. was questioned by respected Japanese virologist Masato Tashiro after touring China in November 2005. These reports came only after Prime Minister Wen Jiabao spoke of a "very serious situation", particularly in the northeast Chinese province of Liaoning . There and in other provinces there had previously been large outbreaks of A / H5N1 among poultry. For example, Nature quotedChinese sources on June 2, 2005, which reported several dozen sick and dead people after an outbreak of A / H5N1 in May 2005 among migratory birds in the northwestern Chinese province of Qinghai . The official Chinese news agency Xinhua immediately denied these reports, but at the same time admitted that the hospitals in the region had set up “special outpatient clinics for febrile patients”. Tests on mice have shown that the Qinghai variant of A / H5N1 is as dangerous for humans as the variants known from Vietnam and Thailand. In June 2006 it became known that a 24-year-old man had proven to have died in China as early as November 2003 as a result of an H5N1 infection.
Thailand
2004: In Thailand, an official review of all illnesses registered in Q1 2004 in 67 of the 76 provinces in people who developed flu-like symptoms or pneumonia after exposure to H5N1-infected poultry found it alongside the 12 confirmed H5N1 illnesses there were a further 21 suspected cases, but these were not included in the statistics. Should this result be transferable to other Asian regions, the actual number of H5N1 cases would be significantly higher, but the death rate at the same time, would be significantly lower than shown in the official statistics.
Turkey and the Middle East
2005-2006:
In Turkey , on January 4, 2006, the authorities in the eastern Turkish city of Van reported several suspected H5N1 cases (mostly children and adolescents) later confirmed by the WHO. All persons had previously dealt intensively with sick poultry. Three siblings aged 11, 14 and 15 years from the village of Doğubeyazıt died, the 14-year-old boy died on January 1, 2006. Genetic analyzes showed that the viruses are very similar to the variants known from Qinghai and Tamiflu and probably even respond to amantadine .
According to a report by the Iraqi Ministry of Health, a 15-year-old girl from Raniya ( Sulaimaniyya province ) died on January 17 as a result of an H5N1 infection, and 10 days later her uncle, who had cared for the girl, died.
On March 14, 2006, the WHO reported on its website the first three deaths from the Salyan district on the Caspian Sea in Azerbaijan , where a total of nine cases were registered after March 6. Four of the fatalities were related or friends and lived close together, the majority of those infected were young women between 15 and 20 years of age. Investigations by the WHO did not reveal any H5N1 evidence in domestic poultry, but did so in sick swans. Relatives of the sick admitted that swans found dead had been removed and the feathers sold. The WHO also considers transmission through the consumption of swan meat to be possible. These cases of illness are considered to be the first evidence that the virus has migrated from wild animals to humans.
Egypt and Djibouti
2006:
On March 29, 2006, the WHO reported that two deaths in Egypt were attributed to influenza A / H5N1 by the US Naval Medical Research Unit (NAMRU-3) . Two 30-year-old women who were handling sick poultry in their home died near Cairo in mid-March. In the following weeks of March, other serious illnesses were linked to A / H5N1 and were finally confirmed by the Weybridge reference laboratory. In the following years a few Egyptians died as a result of an H5N1 infection.
On May 12, the Djibouti Ministry of Health officially announced that the Cairo laboratory had detected NAMRU-3 A / H5N1 in a two-year-old girl who had been ill since April 23. This was also the first H5N1 detection in the Horn of Africa . It was carried out as part of a targeted search for suspected cases in humans, as there had been reports of increased deaths among chickens in this country since the beginning of April. In the official WHO report it was noted that the search for other H5N1 diseases in this country would be hampered by the lack of laboratory capacity and a simultaneous outbreak of dengue fever , since this disease causes symptoms similar to H5N1 infection.
2006–2014: Every year from 2006 to 2013, people in Egypt were infected with the H5N1 virus and several died from it. In these eight years, 173 infections and 63 fatalities were counted, more than half of them in the years 2009 to 2011. In the last two months of 2014, 33 infections and 14 deaths were registered after there had been only isolated cases since spring 2012 .
2015: In the first three months of 2015, 119 infections and 30 deaths were confirmed.
Myanmar and Pakistan
2007:
At the end of November 2007, after a routine check-up that followed an A / H5N1 outbreak among farmed poultry in eastern Myanmar , a seven-year-old girl was found to be infected with H5N1 and later confirmed by WHO. The child was treated in Rangoon and survived the disease.
On December 15, 2007, the WHO reported that 8 cases of illness had been registered in the region of Peshawar ( Pakistan ) and that several sick people had died. The H5N1 infections occurred in an area where poultry had previously contracted A / H5N1.
Possible causes of spread
The reasons for the spread of the bird flu virus are controversial. It is widely believed that it occurs through wild birds. However, there are also indications that the hitherto unsuccessful search for the transmission pathways has wrongly been focused on migratory birds: there is hardly any evidence for this transmission path, apart from local distribution over a few kilometers.
Alternative theories relate to the world trade with poultry , the use of poultry manure as fertilizer in fish farms and in agriculture, slaughterhouse wastes and other waste products of mass poultry farming and the import of wild birds. Sievert Lorenzen, who did research at the Zoological Institute of the University of Kiel, came to the conclusion that it was not migrating wild birds that spread H5N1, but the poultry industry. Among other things, he referred to the findings of the GRAIN organization.
Lorenzen explains:
- The highly pathogenic form of the H5N1 virus can only develop within mass poultry holdings and from there into the open, e.g. B. with poultry droppings or with the exhaust air from the systems.
- The H5N1 avian flu did not spread along the major bird migration routes, but along the major trade routes for poultry and poultry products from mass farms.
- Poultry in small and medium-sized farms that are far from industrial poultry farming played no role in the spread of the H5N1 avian flu.
The bird protection organizations BirdLife and NABU share this view . According to this, migratory birds would not be the vectors of bird flu, but the victims of human activity. If there were increasing indications that factory farming was primarily responsible for the large-scale spread of the epidemic, German crisis management would also have to be reconsidered.
See also
Web links
- World Health Organization (WHO) (PDF): Number of cases in humans, per month, 2003–2006 (PDF; 654 kB)
Individual evidence
- ↑ Avian influenza A (H5N1) - update 31: Situation (poultry) in Asia: need for a long-term response, comparison with previous outbreaks . who.int, March 2, 2004
- ↑ XU Xiyan et al. a .: Genetitic characterization of the pathogenic Influenza A / Goose / Guangdong / 1/96 (H5N1) Virus: Similarity of Its Hemagglutinin Gene to Those of H5N1 Viruses from the 1997 Outbreaks in Hong Kong. In: Virology. Volume 261, No. 1, 1999, pp. 15-19, doi: 10.1006 / viro.1999.9820 , full text. (PDF; 106 kB)
- ↑ H. Chen et al .: Establishment of multiple sublineages of H5N1 influenza virus in Asia: Implications for pandemic control. In: PNAS . Volume 103, 2006, pp. 2845-2850; doi: 10.1073 / pnas.0511120103 . The continuation of the control examinations between June 2005 and June 2006 also showed that the poultry sold on the southern Chinese markets was heavily contaminated: 3.5% of the geese, 3.3% of the ducks and 0.5% of the chickens were infected with H5N1; A total of 53,220 animals were tested: GJD Smith: Emergence and predominance of an H5N1 influenza variant in China. In: PNAS. Volume 103, 2006, pp. 16936-16941; doi: 10.1073 / pnas.0608157103
- ↑ chicken flu - Hong Kong in 1997 at Chemgapedia ( Fachinformationszentrum for the chemical , Berlin) and René snacking et al .: The Next Influenza Pandemic: Lessons from Hong Kong, 1997. In: Emerging Infectious Diseases . Volume 5, No. 2, CDC 1999, doi: 10.3201 / eid0502.990202 , full text
- ↑ oie.int World Organization for Animal Health: "Update on Highly Pathogenic Avian Influenza in Animals" (worldwide overview, from 2004)
- ↑ Nature . Volume 430, 2004, p. 955.
- ↑ b-safe.ch from September 1, 2005 (scroll to the date after opening the link)
- ^ New Scientist, July 9, 2005, p. 14.
- ↑ Nature. Volume 441, 2006, p. 263.
- ↑ In May 2009 there was another outbreak at Lake Genggahu in Qinghai Province, as a result of which 121 wild birds died and 600 breeding animals were killed as a preventive measure. Immediate notification report (PDF; 43 kB) oie.int; Authorities of the People's Republic of China to the OIE, Ref OIE: 8107 dated May 17, 2009
- ↑ D. Cyranoski: Bird flu data languish in Chinese journals . In: Nature . 430, No. 7003, 2004, p. 955. doi : 10.1038 / 430955a .
- ^ D. Butler: Can cats spread avian flu? . In: Nature . 440, No. 7081, 2006, p. 135. doi : 10.1038 / 440135a .
- ↑ a b New Scientist , No. 2588, January 24, 2007, pp. 6-7.
- ↑ A. Amonsina et al .: Genetic characterization of H5N1 influenza A viruses isolated from zoo tigers in Thailand . In: Virology . 344, No. 2, 2006, pp. 480-91. doi : 10.1016 / j.virol.2005.08.032 .
- ↑ WHO: Immediate notification report of February 25, 2015 (PDF) Report reference: REF OIE 17249, Country: China (People's Rep. Of).
- ^ New Scientist , No. 2588, Jan 2007, pp. 6-7.
- ↑ similar also: T. Kuiken, G. Rimmelzwaan, D. van Riel, G. van Amerongen, M. Baars, R. Fouchier, A. Osterhaus: Avian H5N1 Influenza in Cats . In: Science . 306, No. 5694, 2004, p. 241. doi : 10.1126 / science.1102287 .
- ^ T. Kuiken, R. Fouchier, G. Rimmelzwaan, A. Osterhaus, P. Roeder: Feline friend or potential foe? . In: Nature . 440, No. 7085, 2006, p. 741. doi : 10.1038 / 440741a .
- ^ D. van Riel, VJ Munster, E. de Wit, GF Rimmelzwaan, RAM Fouchier, Ab DME Osterhaus, T. Kuiken: H5N1 Virus Attachment to Lower Respiratory Tract . In: Science . 312, No. 5772, 2006, p. 399. doi : 10.1126 / science.1125548 .
- ↑ Information received on 03/15/2012 from Dr Nadav Galon, Director, Veterinary Services and Animal Health, Ministry of Agriculture and Rural Development, BET DAGAN, Israel. On: oie.int of March 15, 2012
- ^ D. Butler: Thai dogs carry bird-flu virus, but will they spread it? . In: Nature . 439, No. 7078, 2006, p. 773. doi : 10.1038 / 439773a .
- ^ Science. Volume 319, 2008, p. 1178.
- ↑ oie.int : Update on Avian Influenza Highly Patheogenic in Animals. (Type H5 and H7). (for 2008)
- ^ OIE: Disease information. Volume 19, No. 6, February 9, 2006, p. 94, full text ( Memento from September 23, 2015 in the Internet Archive )
- ↑ Follow-up report No. 1. (PDF; 34 kB), OIE Ref: 4568, of the Indian health authorities from February 23, 2006
- ↑ OIE: Disease Information , Volume 19, No. 23, June 8, 2006 ( Memento from September 23, 2015 in the Internet Archive ), p. 450, full text ( Memento from September 23, 2015 in the Internet Archive )
- ↑ oie.int (PDF; 28 kB): Immediate notification report, Ref OIE: 4608 , of the Pakistani health authorities of March 2, 2006
- ↑ oie.in (PDF; 36 kB) Message from the Indian health authorities dated December 2, 2006, OIE Ref: 4619
- ↑ Immediate notification report (Ref OIE: 7695). (PDF; 19 kB) oie.int, January 16, 2008.
- ↑ Follow-up report No. 8. Reference OIE: 13510. (PDF; 84 kB) oie.int, May 26, 2013:
- ↑ Immediate notification report. REF OIE 13447, Report Date: 13/05/2013, Country: Korea (Dem. People's Rep.) . (PDF; 48 kB) oie.int, May 13, 2013:
- ↑ tagesspiegel.de of April 1, 2006: "Bussard in Berlin had aggressive bird flu."
- ↑ The virus is dormant. In: Süddeutsche Zeitung . No. 4/2007 of January 5, 2007, p. 22.
- ↑ Süddeutsche Zeitung. No. 153 of 6 July 2006, p. 18.
- ↑ Nature. Volume 442, 2006, p. 37.
- ↑ who.int of February 9, 2006: "Avian influenza in Africa: statement by the Director-General of WHO."
- ↑ oie.int (PDF; 26 kB) Immediate notification report, Ref OIE: 1090 of the national health authorities of February 28, 2006
- ↑ oie.int (PDF; 24 kB) Follow-up report No. 2, OIE Ref: 1792
- ↑ oie.int (PDF; 53 kB) Immediate notification report, Ref OIE: 4291 , of the Egyptian health authorities from February 18, 2006
- ↑ oie.int (PDF; 756 kB) of December 3, 2007, Follow-up report No .: 2, OIE Ref: 5687 (comprehensive overview).
- ↑ oie.int (PDF; 34 kB) Immediate notification report, Ref OIE: 4133 , of the Sudanese authorities from April 18, 2006.
- ↑ oie.int (PDF; 47 kB) Follow-up report No. 4, OIE Ref: 4635.
- ↑ oie.int (PDF; 47 kB) Follow-up report No. 5, OIE Ref: 6515 , of the Sudanese Health Authorities dated November 25, 2007.
- ^ OIE: Immediate notification report. (PDF) of January 20, 2015, REF OIE 17014, Report Date: 20/01/2015, Country: United States of America.
- ↑ Report reference: REF OIE 16771, Report Date: 16/12/2014, Country: United States of America. (PDF) On: oie.int , December 16, 2014.
- ↑ OIE: Report of April 15, 2015 , Information received on April 15, 2015 from Dr John Clifford, Deputy Administrator, Animal and Plant Health Inspection Service, United States Department of Agriculture, Washington.
- ↑ Report reference: CAN-2015-NAI-001 REF OIE 17152, Report Date: 06/02/2015, Country: Canada. (PDF) On: oie.int , February 7, 2015.
- ↑ who.int : "Influenza at the Human-Animal Interface (HAI)" - entry page to the WHO reports on A / H5N1.
- ↑ JC De Jong, EC J Claas, A. Osterhaus , RG Webster and WL Lim: A pandemic warning. In: Nature. Volume 389, 1997, p. 554.
- ↑ Details on the family clusters 2004/05: recombinomics.com of February 3, 2005: Commentary: Visible Human to Human Bird Flu Transmission in Vietnam.
- ^ Science . July 29, 2005, p. 684.
- ↑ who.int of December 4, 2007: "Avian influenza - situation in China - update 4"
- ↑ welt.de of April 8, 2008: "China proves infection from person to person"
- ↑ Hua Wang et al .: Probable limited person-to-person transmission of highly pathogenic avian influenza A (H5N1) virus in China. In: The Lancet . Volume 371, No. 9622, 1008, pp. 1427-1434, doi: 10.1016 / S0140-6736 (08) 60493-6
- ↑ Avian influenza - situation in Indonesia - update 16. To: who.int from May 31, 2006.
- ↑ Declan Butler: Pandemic 'dry run' is cause for concern. In: Nature . Volume 441, 2006, pp. 554–555, doi: 10.1038 / 441554a , full text ( Memento from December 2, 2013 in the Internet Archive ; PDF)
- ↑ Bird Flu Passed From Son to Father, WHO Says. On: nytimes.com from June 23, 2006.
- ↑ Dennis Normile: human transmission but no pandemic in Indonesia. In: Science , Volume 312, 2006, p. 1855, doi: 10.1126 / science.312.5782.1855b .
- ^ Declan Butler: Family tragedy spotlights flu mutations. In: Nature , Volume 442, No. 7099, 2006, pp. 114-115, doi: 10.1038 / 442114a . ( Excerpts from the author ).
- ↑ who.int (PDF; 26 kB): "Cumulative number of confirmed human cases of avian influenza A / (H5N1) reported to WHO" (number of cases since 2003).
- ↑ H5N1 avian influenza: Timeline of major events . (PDF; 385 kB) Status: December 13, 2011.
- ↑ Nature, July 7, 2005
- ^ The New England Journal of Medicine. Volume 354, 2006, pp. 2731 f.
- ↑ recombinomics.com of January 5, 2005: Commentary: Fatality Rate in Missed Thailand Bird Flu Cases.
- ^ WHO study results according to Frankfurter Allgemeine Zeitung No. 127 of June 2, 2006, p. 34.
- ↑ who.int of March 29, 2006: Avian influenza - situation in Egypt.
- ↑ a b Cumulative number of confirmed human cases of avian influenza A (H5N1) reported to WHO. WHO, accessed May 18, 2015 .
- ↑ Avian influenza A (H5N1) situation update, April 30, 2015 Egypt. (PDF) Retrieved May 18, 2015 (Infographic).
- ↑ who.int (PDF): Influenza at the human-animal interface. Summary and assessment as of 26 January 2015.
-
↑ who.int (PDF; 385 kB) H5N1 avian influenza: Timeline of major events , p. 21
flu.org.cn of December 16, 2007: "Bird flu kills first human in Pakistan, child first case in Myanmar." ( Report from the AFP news agency ) - ↑ who.int Avian influenza - situation in Pakistan , December 15th 2007
- ↑ see e.g. B. Wolfgang Fiedler: The role of wild birds in the transmission of avian influenza. In: Reports on bird protection. Volume 42, 2005, pp. 33-45.
- ↑ Sivert Lorenzen: Evolution and spread of the bird flu virus H5N1 Asia and aspects of biosecurity. In: Veterinary survey. Volume 63, No. 6, 2008, pp. 333–339, full text (PDF; 122 kB)
- ↑ Fowl play - The poultry industry's central role in the bird flu crisis . ( Memento from February 1, 2012 in the Internet Archive ; PDF; 420 kB) GRAIN Briefing, February 2006
- ^ BirdLife Statement on Avian Influenza. ( Memento of May 13, 2008 in the Internet Archive ) As of August 2007
- ↑ How dangerous is bird flu? The NABU info page on the topic. nabu.de; accessed on September 23, 2015
- ↑ Info sheet: Avian influenza and wild birds: What role do wild birds play in the spread of the virus? (PDF; 554 kB) Prepared by: International Scientific Task Force on Avian Flu ; accessed on September 23, 2015.