Dengue fever
| Classification according to ICD-10 | |
|---|---|
| A90 | Dengue fever [classic dengue] |
| A91 | Dengue hemorrhagic fever |
| ICD-10 online (WHO version 2019) | |
The dengue fever [ dɛŋge- ], including dengue , polka fever , bone crusher fever , seven-day fever and shortly Dengue is a disease whose cause is an infection with the dengue virus is. The virus is a 40 to 60 nm large, enveloped RNA virus with positive polarity from the flavivirus family .
The virus is transmitted by a mosquito bite and is common in tropical and subtropical areas. The only known hosts for the virus are primates and various mosquito species. There are four different serotypes (subgroups) of the virus, which most likely independently jumped from non-human primates to humans in Asia over the past 2000 years. Since the Second World War and the subsequent globalization , dengue fever has been on the advance, among other things due to the spread of its vector, and is often referred to as an emerging disease . Dengue is the fastest spreading, viral, mosquito-borne disease; the number of cases increased thirty-fold between 1960 and 2010.
The disease often manifests itself with unspecific symptoms or symptoms resembling severe flu ; internal bleeding can also occur. In a serious disease a so-called can "Hemorrhagic Dengue" (DHF) or dengue shock - syndrome (DSS) occur, both of which can lead to death. The WHO estimates that 50 to 100 million people fall ill every year, 500,000 people suffer from severe disease and 22,000 people die of dengue fever; most of the fatalities are children. Scientists from Oxford and Heidelberg reported in the journal Nature in April 2013 that, according to their research, around 390 million people were actually infected with the pathogen causing dengue fever each year.
For a long time there was no specific antiviral treatment for the disease. At the end of 2015, the first vaccine, " Dengvaxia ", was approved by Sanofi , which is supposed to be effective against all four variants of the virus and offer vaccine protection of 93%. However, later studies have shown that those who have never had dengue fever and were then vaccinated with Dengvaxia can later become infected and then develop even more severe symptoms than people who were not vaccinated. In Germany, Austria and Switzerland there is an obligation to report suspicion, illness, death, direct and indirect pathogen detection or hemorrhagic course of the disease.
Pathogen
Dengue fever is caused by one of the four serotypes (DENV-1 to DENV-4) of the dengue virus . It is a round, enveloped virus with a diameter of 40 to 60 nm from the flavivirus family . The viral genome (in contrast to the DNA used by all living things ) consists of ribonucleic acid (RNA). The genome is about 11,000 nucleotides long and is positive-stranded, so it can be read directly from ribosomes and with this information a protein (amino acid chain) can be formed. The genome only comprises an open reading frame that codes for a polyprotein (a long amino acid chain that has to be cut into the individual functional proteins afterwards).
During an infection, the viruses attach to the cell surface of a host cell via specific receptors and are taken up by a developing endosome vesicle . These vesicles are normally used to digest substances , but the virus uses them as a means of transport to get inside the cell. Inside the endosome, the acidic pH induces the fusion of the endosome membrane and the virus envelope , which allows the virus content to penetrate the cytosol . Thereafter, the viral genome in the rough endoplasmic reticulum (ER) and in so-called vesicle packets replicated and, after maturation in the Golgi apparatus arise infectious virus particles. These leave the cell and attack other host cells.
The four different serotypes occur either in demarcated or overlapping endemic zones . Phylogenetic analyzes make it possible to subdivide the individual serotypes into genotypes . DENV-1 and DENV-2 are divided into five genotypes, DENV-3 and DENV-4 each into four genotypes. Molecular biological investigations have shown that the endemic genotypes split off from the (silvatic) genotypes occurring in forests or in the jungle in the last 2000 years. DENV-2 then jumped over to humans about 1000 years ago, DENV-4 600 years ago and DENV-1 200 years ago (all data ± 50%). No silvatic strain has yet been isolated from DENV-3, and consequently no statement can be made about a possible point in time at which the virus was split off.
transmission
The most important vectors ( vectors ) of the dengue virus are the females of the yellow fever mosquito ( Aedes aegypti , also called Egyptian tiger mosquito or dengue mosquito, synonym Stegomyia aegypti ) and the Asian tiger mosquito ( Aedes albopicta ), which is also spreading in Europe , synonym Stegomyia albopicta . In certain regions there are other types of mosquitos as carriers of dengue fever. B. the Polynesian tiger mosquito ( Aedes (Stegomyia) polynesiensis ) in the southern Pacific or Aedes (Stegomyia) scutellaris in New Guinea . In other mosquito species, a suitability for the transmission of pathogens (vector competence) was also shown.
As with other mosquito-borne arboviruses , dengue virus is ingested by a female mosquito who suckles the blood of an infected person. The viruses get into the mosquito's stomach and if the virus concentration is high enough, the virions can attack the gastric epithelial cells and multiply there. From there they get into the haemocoil (the mosquito's blood system) and on to the salivary glands . The next time the mosquito sucks blood, it injects its saliva into the wound, bringing the virus into the bloodstream of the stung primate. There is also evidence of a vertical infection of the dengue virus, i.e. the transmission from the female mosquito to her clutch and thus the larvae . This infection of the vectors without a previous blood meal appears to play a role in maintaining a reservoir of virus between outbreaks.
There are two epidemiologically distinguishable infection cycles in which the virus is transmitted from mosquitoes to humans or other primates . The yellow fever mosquito and the Asian tiger mosquito are involved in the so-called urban cycle, which are well adapted to large urban centers and transmit other diseases in addition to dengue fever.
In addition to the urban cycle, there is a silvatic cycle (forest cycle or jungle cycle) in both Africa and Asia, but very likely not in America , in which the mosquitoes Aedes (Diceromyia) furcifer and Aedes ( Stegomyia) luteocephala serve as vectors. Mainly non-human primates are infected in the jungle. While DENV-2 only circulates silvatically in Africa, in Asia this is very likely the case with all four serotypes. There is no evidence that the Silvatic cycle was involved in past dengue epidemics, but it is known that the pathogens of the Silvatic cycle can also infect humans.
distribution

Dengue fever is endemic to tropical and subtropical areas with 75% of global dengue cases occurring in the Asia / Pacific region. The main distribution areas include Latin America , Central Africa , India , Southeast Asia , parts of the Pacific (including New Caledonia and Hawaii ) and the southern United States .
Around half of the world's people live in endemic areas , and WHO's official estimates are between 50 and 100 million diseases, 500,000 serious disease courses and 22,000 deaths annually. In Asia, children account for over 90% of serious illnesses. According to the WHO , the number of illnesses roughly doubled between 2000 and 2010. Laos and the Philippines are particularly hard hit by this development.
Dengue is not endemic in Europe, with the spread of the vector mosquitoes Aedes aegypti and especially Ae. albopictus increases the risk of locally (autochthonously) transmitted infections that originate from imported cases. Between September 2012 and March 2013, for example, a dengue outbreak occurred on the Portuguese Atlantic island of Madeira with 1,080 proven cases. There were no major clinical and no deaths. The vector mosquito was Aedes aegypti , which was introduced to the island in 2005. The Asian tiger mosquito Aedes albopictus is now widespread in southern Europe and continues to expand its settlement area. In 2010, the first indigenous dengue fever cases occurred in southern France and Croatia . In 2013, another locally transmitted dengue infection was detected near Aix-en-Provence (southern France). In August 2015, two autochthonously acquired cases of dengue were discovered in Nîmes in the south of France . In October 2018, another five autochthonously acquired cases in Saint-Laurent-du-Var became known.
Symptoms
Dengue is transmitted by a mosquito bite and has an incubation period of three to 14 days. Most cases are mild ("oligosymptomatic", that is, accompanied by few symptoms), as is often observed with a flu-like infection . Symptoms include fever (up to 40 ° C) with chills and severe pain in the head, muscles, and limbs. Together with a rash ( exanthema ), these symptoms are also known as denguetrias. Diffuse hair loss can occur as a late manifestation up to two months after the onset of the disease.
In most patients, the disease resolves after 3 to 7 days. In about 2-4% of cases, however, the disease becomes severe and dengue hemorrhagic fever (DHF) or dengue shock syndrome (DSS) can occur. These severe courses end fatally in 1–5% of all cases, but the mortality rate in individual epidemics can also reach 15%.
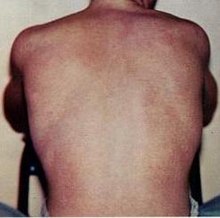
The hemorrhagic dengue (DHF) is an acute shock syndrome with haemorrhages , the permeability (in the course of permeability ) of the blood vessel walls becomes larger and, therefore, uncontrolled bleeding occur. The hemorrhagic form begins like normal dengue fever, but the condition of the sick worsens dramatically after two to six days. The blood circuit breaks down and it comes to the redness of the face, to the (inner) bleeding, fluid loss, brain-related (cerebral) seizures, coma , bleeding gums, hematemesis, melena , swelling of the liver and the general signs of shock ( tachycardia , hypotension , clammy Skin, pallor). In addition, disseminated petechiae can occur in this phase . These are microcircular hemorrhages on the skin that appear as red spots.
If the infection survives, there is brief immunity against all serotypes and lifelong immunity against the infecting strain.
Infection-enhancing antibodies
During infection with one of the four dengue serotypes (DENV-1, DENV-2, DENV-3 and DENV-4) only antibodies against this particular serotype are produced. The infected person remains vulnerable to viruses of a different serotype.
In the event of a second infection by a virus of a different serotype, the antibodies - which can be acquired through a previous illness or transmitted from mothers to their children - against the first serotype are not able to neutralize the new virions . Instead, antibody-virus complexes are formed which are absorbed by macrophages , but are not destroyed by them, but allow the viruses to continue to multiply. In the case of a second infection, this leads to a higher viral load than in the case of a first infection (these ineffective antibodies are referred to as infection-enhancing antibodies or ADE for Antibody-dependent enhancement of infection ). At the molecular level, it has been observed that cells with Fcγ receptors or complement receptors are particularly susceptible to the virus at low antibody concentrations. This explains why children whose protective maternal antibody concentration is currently decreasing are particularly often affected by DHF. Furthermore, it is assumed that the antibodies against a certain virus strain bind a second strain with reduced avidity and therefore also lead to ADE. One possible explanation for this phenomenon is that the antibodies cause the virus to bind to the cell more efficiently.
This hypothesis is considered very likely, as the following example from Cuba shows: In 1977 a DENV-1 epidemic had struck the island and infected 44% of the population, with only mild symptoms being observed. In 1981 a DENV-2 epidemic was registered with more than 10,000 cases of DSS / DHF. The death rate of children aged 3-14 years was almost 15 times higher than that of adults. In 2001, a DENV-3 epidemic broke out in Havana . Only adults were affected by DSS / DHF because the children were too young to have seen the DENV-2 epidemic of 1981.
diagnosis
The clinical diagnosis is difficult because of the large number of possible pathogens for infectious diseases with similar initial symptoms. Sporadic and only mild courses can only be reliably recognized by a virological examination.
If an infection is suspected, the dengue virus can be detected using the reverse transcriptase polymerase chain reaction (RT-PCR), in which the genetic material of the virus is duplicated and thus detected directly. The direct detection of the pathogen can also be carried out via virus isolation by culturing in cell culture, whereby this process can take one to four weeks. Both procedures are carried out with blood plasma , the PCR also with blood serum . Serologically , an enzyme-linked immunosorbent test in the acute phase cannot usually detect any dengue-specific IgM antibodies , but if it is positive it can confirm the diagnosis after the symptoms have subsided. The specific IgG - titer can distinguish between an initial infection or a secondary infection (at a initial infection occur in the first 8 days no IgG antibodies). A four-fold increase in the specific antibody titer compared to a preliminary sample is considered reliable evidence. Since the serological test methods often cross-react with other flaviviruses , these indirect methods are never conclusive for an infection.
Antigen tests based on the direct detection of the NS1 protein (which is highly conserved within the four serotypes) are also commercially available. They are characterized by their easy handling (no laboratory required), but are significantly less sensitive and specific than more complex test methods.
The handling of all test material from the patient, especially blood, is subject to strict safety regulations and may only be carried out in laboratories of protection level 3 .
Differential diagnosis
If dengue fever is suspected, other viral ( influenza , measles , rubella , chikungunya , yellow fever and Japanese encephalitis ) and bacterial ( typhoid , leptospirosis , sepsis , meningococci and rickettsial diseases) and malaria should be excluded.
According to the WHO recommendations, the blood of a patient suspected of having dengue fever should be tested for antibodies against the chikungunya virus whenever an infection with dengue virus cannot be detected and the patient has been in an area where the chikungunya fever occurs.
Reporting requirement
In Austria, dengue fever is notifiable in the event of illness or death in accordance with Section 1, Paragraph 1, Number 1, Epidemic Act 1950 . Doctors and laboratories, among others, are obliged to report this ( Section 3 Epidemics Act).
In Switzerland, doctors, hospitals, etc., or the laboratory investigating , are obliged to report positive laboratory analysis results for the disease dengue fever or the pathogen dengue virus . This results from the Epidemics Act (EpG) in conjunction with the Epidemics Ordinance and Annex 1 or Annex 3 of the Ordinance of the FDHA on the reporting of observations of communicable diseases in humans .
In Germany, according to Section 6 of the Infection Protection Act (IfSG) , dengue fever must be reported by name if a virus- related hemorrhagic fever is suspected or, according to Section 7 IfSG, if the pathogen dengue virus is detected by the doctor or the laboratory . In the second case, it is primarily the heads of the laboratories, etc., and only in the case of hemorrhagic fever also the diagnosing doctor ( Section 8 IfSG) that are required to report .
treatment
As for all diseases caused by flaviviruses , there is no causal therapy for dengue fever . In severe cases, admission to a hospital (hospitalization) must be carried out and, due to the rapidly deteriorating condition of the disease in some cases, intensive medical supervision is advisable. Symptomatic treatment includes measures to replenish fluids ( rehydration ) and administration of agents such as paracetamol to relieve pain. On acetylsalicylic acid (. Eg aspirin ) should be avoided because of their anticoagulant effect, as this in the case of internal bleeding, which can occur in dengue fever, has devastating consequences for the patient. Furthermore, the early intravenous administration of fluids can be of decisive importance.
prevention
Unlocked water containers and small amounts of stagnant water that collects in buckets, cans, bottles, car tires or plastic sheeting are sufficient as larval biotopes. In addition, the eggs of the tiger mosquitoes are drought-resistant and can therefore survive dry periods. All of this makes it difficult to control the mosquitoes.
Personal precautions against dengue include avoiding mosquito bites in areas where dengue is endemic. Institutional measures to prevent dengue fever include measures to control the disease-transmitting mosquitoes.
Personal Prevention
Bites can be avoided in particular by wearing suitable clothing and repellants such as mosquito- repellent sprays. Since the adult tiger mosquitoes are diurnal, you can only protect yourself to a limited extent with bed nets, which are effective against malaria , for example . Mosquito repellent sprays with a high DEET content can further reduce the risk of a bite.
vaccination
Strategic prevention


Although the first vaccine against dengue viruses has been available since the end of 2015, combating vector mosquitoes continues to play a central role. The yellow fever mosquito Stegomyia aegypti prefers to breed in pools of water that were created by residents in areas with problematic drinking water supplies or that accumulate in household waste; especially in tires , but also in old cans and plastic containers. These conditions are particularly common in the vicinity of urban centers in developing countries and form an excellent habitat for the yellow fever mosquito. Two strategies are followed in combating the mosquito:
- Control of the developing larvae. One of the most important strategies at the moment is based on the most comprehensive disposal of larval waters supported by the general public. In addition to measures to reduce larval waters, chemical larvicides as well as larval- eating fish and copepods are used, which directly reduce the number of larvae and thus indirectly the number of mosquitoes that transmit disease. In Vietnam, copepods of the genus Mesocyclops have been used to combat dengue fever for several years , with the implementation of the measures being checked monthly. As a result, no more cases of dengue fever occurred in the affected areas between 2002 and 2005. Pyriproxyfen is mainly recommended as a chemical larvicide because it is safe for humans and effective even in small amounts.
- Control of adult yellow fever mosquitoes. Curtains and covers of water tanks are treated with insecticide . They kill female mosquitoes which are dormant or looking for egg-laying waters. Furthermore, insecticide can be sprayed indoors, but this is not recommended by the WHO. A newer method is the use of special traps with an attractant mixture that have been optimized for catching tiger mosquitoes .
Other approaches are:
- the spread of mosquitoes immunized against the virus by wMel Wolbachia (bacteria of the genus Wolbachia ).
- the release of genetically modified males of the yellow fever mosquito There have been and still are numerous concerns about the release of around 10 million genetically modified male mosquitoes in Brazil.
- a parasitic fungus ( Beauveria bassiana ) that kills or weakens mosquitoes.
history
The origin of the name dengue is not clear. An early name for it was dandy fever ; later the Spanish name dengue came up, which indicates a pain-related, noticeably peculiar change in posture and behavior in sick people. According to other sources, dengue comes from the African language area ( Swahili : dinga ) and stands for a seizure that is triggered by an evil spirit.
The first mention of the disease is seen by some in the Chinese Jin dynasty (265–420) and later in the 1st millennium of our era. The next reports of dengue fever came from Panama (1635, 1699), Jakarta (1779–1788), Cairo (1881, 1883), Philadelphia (1789) and Spain (1881) and show the widespread spread of the disease at that time.
1927–1929 a dengue epidemic raged in Greece with more than a million infected people - the last epidemic before the eradication of the yellow fever mosquito ( Stegomyia aegypti ) in the Mediterranean area and the disappearance of dengue from this area. The mobility of troops during the Second World War led to major dengue epidemics between 1941 and 1945. As early as the 1960s, the spread of the virus increased sharply and the four serotypes were circulating in Asia. In the 1990s the global spread of dengue was complete, caused in particular by the abandonment of vector control programs, increased urbanization and globalization (individual mobility ). In 1998 a global pandemic was registered with more than 1.2 million cases in 56 countries. Dengue is on the rise and is known as the emerging disease .
Through a policy of vector control, dengue case numbers declined on the American continent during the 1960s and 1970s. Since the 1980s, however, the number of dengue fever cases in South America has risen again and the yellow fever mosquito has returned to the urban centers in South America, partly because the vector control programs were abandoned. On the American continent, major outbreaks of dengue fever followed in Brazil (2002, 2007), Paraguay (2007) and Mexico (2007). In some countries, a series of epidemics can be observed in which the serotypes alternate. There were outbreaks in Cuba in 1977 (DENV-1), 1981 (DENV-2) and 2001 (DENV-3), and in Brazil there were outbreaks in 1986 (DENV-1), 1990/1998 (DENV-2) , 2002–2005 (DENV-3) and 2007/2008 (DENV-2).
In 2019, Brazil, Mexico, Nicaragua, Colombia and Honduras were hardest hit in South and Central America.
research
In the 20th century the first steps to identify and control the causative agent of the disease were taken. After the successful scientific investigation of yellow fever virus by Finlay , Reed, and others, attention was drawn to dengue fever. Percy M. Ashburn and Charles F. Craig showed in 1907 that dengue fever is caused by a non-filterable factor, a virus just like yellow fever. Stegomyia aegypti was identified as a vector by Joseph Franklin Siler, Milton W. Hall, and Arthur Parker Hitchens in 1926.
In the late 1960s and early 1970s put Scott B. Halstead his hypothesis about infection-enhancing antibodies , which states that a second infection may be more dangerous than an initial infection. In 1970, the isolation of a virus from a human confirmed the hypothesis that silvatic pathogens can also infect humans.
Dengue fever has been studied by the US government as a potential biological weapon . This program was officially discontinued in 1970. Still, the United States was accused of being responsible for the dengue outbreak in Cuba in 1981 .
The so-called Pediatric Dengue Vaccine Initiative , financed by private and public bodies, is trying to develop a safe dengue virus vaccine . Various vaccine strains are already successfully in clinical test phases I, II and III. The French pharmaceutical company Sanofi Pasteur MSD announced in October 2010 that it would develop a vaccine by 2015. This tetravalent vaccine against all four known subtypes of dengue has already been successfully tested in a phase III study. Other researchers tried to stop the transmission with the help of Wolbachia .
literature
- Dengue - Guidelines for diagnosis, treatment, prevention and control. (PDF; 1.5 MB) WHO, accessed on June 14, 2010 (English). .
- David M. Knipe, Peter M. Howley et al. (Eds.): Fields' Virology . (2 volumes; standard work on virology) 5th edition. Lippincott Williams & Wilkins, Philadelphia 2007, ISBN 978-0-7817-6060-7 .
- Peter Stingl: Dengue fever - More than 50 million infected people: The world's most common arbovirus with continuous spread . In: Deutsches Ärzteblatt. 2005, Vol. 102, No. 22, pp. A1594-A1595.
- Anonymous: Dengue fever. The unknown pandemic . In: Pharmaceutical newspaper. 2002, Vol. 147, No. 7, pp. 52-55, ISSN 0031-7136 .
- Anonymous: Dengue fever spread around the world. In: Pharmaceutical newspaper. 2004, Vol. 149, No. 14, pp. 50-53, ISSN 0031-7136 .
- GU Kuhnle, W. Krahl: Dengue fever and hemorrhagic dengue fever. The deadly pandemic of the 20th century . In: Monthly Pediatrics . tape 147 , no. 1 , January 1999, p. 48-50 , doi : 10.1007 / s001120050397 .
- MA Tolle: Mosquito-borne diseases . In: Curr Probl Pediatr Adolesc Health Care . tape 39 , no. 4 , April 2009, p. 97-140 , doi : 10.1016 / j.cppeds.2009.01.001 , PMID 19327647 .
Selected free scientific review articles
- Pubmed search
- DJ Gubler: Dengue and dengue hemorrhagic fever . In: Clin. Microbiol. Rev. Band 11 , no. 3 , July 1998, pp. 480-496 , PMID 9665979 , PMC 88892 (free full text).
- R. Rico-Hesse: Microevolution and virulence of dengue viruses . In: Adv. Virus Res. Band 59 , 2003, p. 315-341 , PMID 14696333 , PMC 3045824 (free full text).
- PY Shu, JH Huang: Current advances in dengue diagnosis . In: Clin. Diagn. Lab. Immunol. tape 11 , no. 4 , July 2004, p. 642-650 , doi : 10.1128 / CDLI.11.4.642-650.2004 , PMID 15242935 , PMC 440621 (free full text).
- GN Malavige, S. Fernando, DJ Fernando, SL Seneviratne: Dengue viral infections . In: Postgrad Med J . tape 80 , no. 948 , October 2004, p. 588-601 , doi : 10.1136 / pgmj.2004.019638 , PMID 15466994 , PMC 1743110 (free full text).
- M. Hemungkorn, U. Thisyakorn, C. Thisyakorn: Dengue infection: a growing global health threat . In: Biosci Trends . tape 1 , no. 2 , October 2007, p. 90-96 , PMID 20103874 .
- BE Martina, P. Koraka, AD Osterhaus: Dengue virus pathogenesis: an integrated view . In: Clin. Microbiol. Rev. Band 22 , no. 4 , October 2009, p. 564-581 , doi : 10.1128 / CMR.00035-09 , PMID 19822889 , PMC 2772360 (free full text).
- SC Weaver, WK Reisen: Present and future arboviral threats . In: Antiviral Res. Band 85 , no. 2 , February 2010, p. 328-345 , doi : 10.1016 / j.antiviral.2009.10.008 , PMID 19857523 , PMC 2815176 (free full text).
About vaccinations
- Anonymous: Dengue vaccines are feverishly wanted . In Pharmazeutische Zeitung 155 (23) (2010), ISSN 0031-7136
- MJ Cardosa: Dengue vaccine design: issues and challenges . In: Br. Med. Bull. Band 54 , no. 2 , 1998, p. 395-405 , PMID 9830205 .
- UC Chaturvedi, R. Shrivastava, R. Nagar: Dengue vaccines: problems and prospects . In: Indian J. Med. Res. Band 121 , no. 5 , May 2005, pp. 639-652 , PMID 15937367 .
- R. Edelman: Dengue vaccines approach the finish line . In: Clin Infect Dis . 45 Suppl 1, July 2007, p. S56-S60 , doi : 10.1086 / 518148 , PMID 17582571 .
- K. Raviprakash, G. Defang, T. Burgess, K. Porter: Advances in dengue vaccine development . In: Hum Vaccin . tape 5 , no. 8 , August 2009, p. 520-528 , PMID 19535912 .
About history
- JG Rigau-Pérez: The early use of break-bone fever (Quebranta huesos, 1771) and dengue (1801) in Spanish . In: Am. J. Trop. Med. Hyg. Band 59 , no. 2 , August 1998, p. 272-274 , PMID 9715945 .
- G. Kuno: Emergence of the severe syndrome and mortality associated with dengue and dengue-like illness: historical records (1890 to 1950) and their compatibility with current hypotheses on the shift of disease manifestation . In: Clin. Microbiol. Rev. Band 22 , no. 2 , April 2009, p. 186-201 , doi : 10.1128 / CMR.00052-08 , PMID 19366911 , PMC 2668235 (free full text).
- N. Vasilakis, SC Weaver: The history and evolution of human dengue emergence . In: Adv. Virus Res. Band 72 , 2008, p. 1-76 , doi : 10.1016 / S0065-3527 (08) 00401-6 , PMID 19081488 .
About infection-enhancing antibodies
- TC Pierson, MS Diamond: Molecular mechanisms of antibody-mediated neutralization of flavivirus infection . In: Expert Rev Mol Med . tape 10 , 2008, p. e12 , doi : 10.1017 / S1462399408000665 , PMID 18471342 , PMC 2671962 (free full text).
Web links
- Dengue fever - information from the Robert Koch Institute
- Dengue - Information from the Centers for Disease Control and Prevention
- Dengue - Information from the World Health Organization
- DengueMap healthmap.org, accessed September 7, 2012
Individual evidence
- ↑ a b c d e f g h i j k l N. Vasilakis, SC Weaver: The history and evolution of human dengue emergence . In: Adv. Virus Res. Band 72 , 2008, p. 1-76 , doi : 10.1016 / S0065-3527 (08) 00401-6 , PMID 19081488 .
- ↑ Meyer's large pocket dictionary in 24 volumes. Volume 5 (Con-Dug), Mannheim 1992, p. 116.
- ↑ a b c WHO | Dengue and dengue haemorrhagic fever. Retrieved June 14, 2010 .
- ↑ a b c Dengue - Guidelines for diagnosis, treatment, prevention and control. (PDF; 1.5 MB) WHO, accessed on June 14, 2010 (English).
- ↑ Samir Bhatt, Peter W. Gething, Oliver J. Brady and others: The global distribution and burden of dengue. In: Nature. No. 496, April 25, 2013, pp. 504–507, doi: 10.1038 / nature12060 ( full text online ).
- ↑ Alexandra Jane Oliver: Tropical disease: Mexico allows the world's first dengue vaccine . On: Spiegel Online. dated December 10, 2015.
- ↑ Drug firm warns of 'severe disease' from dengue vaccine for people with no prior infection. In: CNN Philippines. November 30, 2017, accessed July 14, 2018 .
- ↑ a b A. Sampath, R. Padmanabhan: Molecular targets for flavivirus drug discovery . In: Antiviral Research . tape 81 , no. 1 , January 2009, p. 6-15 , doi : 10.1016 / j.antiviral.2008.08.004 , PMID 18796313 .
- ↑ D. Fontenille, AB Failloux, R. Romi: Should we expect Chikungunya and Dengue in Southern Europe? In: W. Takken, BGJ Knols (Ed.): Emerging pests and vector-borne diseases in Europe. 2007, Volume 1, Wageningen Academic Publishers, ISBN 978-90-8686-053-1 .
- ↑ L. Rosen, LE Rozeboom, BH Sweet & AB Sabin: The transmission of dengue by 'Aedes polynesiensis' Marks. In: Am. J. Trop. Med. Hyg. 1954, No. 3, pp. 878-882.
- ↑ IM Mackerras: Transmission of dengue fever by Ae. (Stegomyia) scutellaris Walk. in New Guinea. In: Trans. R. Soc. Trop. Med. Hyg. 1946, No. 40, pp. 294-312.
- ↑ a b JE Freier, L. Rosen: Vertical transmission of dengue virus by mosquitoes of the 'Aedes scutellaris' group. In: Am. J. Trap. Med. Hyg. 1987, Vol. 37, No. 3, pp. 640-647.
- ↑ a b J. E. Freier, L. Rosen: Vertical transmission of dengue virus by 'Aedes mediovittatus'. In: Am. J. Trop. Med. Hyg. 1988, Vol. 39, No. 2, pp. 218-222.
- ^ J. Günther, JP Martínez-Muñoz, DG Pérez-Ishiwara, J. Salas-Benito: Evidence of vertical transmission of dengue virus in two endemic localities in the state of Oaxaca, Mexico . In: Intervirology . tape 50 , no. 5 , 2007, p. 347-352 , doi : 10.1159 / 000107272 , PMID 17700030 .
- ↑ V. Thenmozhi, JG Hiriyan, SC Tewari include: Natural vertical transmission of dengue virus in Aedes albopictus (Diptera: Culicidae) in Kerala, a southern Indian state . In: Jpn. J. Infect. Dis. tape 60 , no. 5 , September 2007, pp. 245-249 , PMID 17881861 .
- ↑ B. Angel, V. Joshi: Distribution and seasonality of vertically transmitted dengue viruses in Aedes mosquitoes in arid and semi-arid areas of Rajasthan, India . In: J Vector Borne Dis . tape 45 , no. 1 , March 2008, p. 56-59 , PMID 18399318 .
- ↑ tropeninstitut.de
- ↑ a b c d e f g h i j k MA Tolle: Mosquito-borne diseases . In: Curr Probl Pediatr Adolesc Health Care . tape 39 , no. 4 , April 2009, p. 97-140 , doi : 10.1016 / j.cppeds.2009.01.001 , PMID 19327647 .
- ^ European Center for Disease Prevention and Control. Dengue outbreak in Madeira, Portugal, March 2013. Stockholm, ECDC 2014 ISBN 978-92-9193-564-2
- ↑ J. Schmidt-Chanasit, M. Haditsch, I. Schoeneberg, S. Gunther, K. Stark, C. Frank: Dengue virus infection in a traveler returning from Croatia to Germany. In: Euro Surveill. 2010, Volume 15, No. 40, p. 19677, PMID 20946759 .
- ↑ Marchand et al.: Autochthonous case of dengue in France, October 2013. In: Euro Surveill. 18 (50), 2013, p. 20661.
- ↑ Chikungunya et dengue - Données de la surveillance renforcée en France métropolitaine en 2015 Communication of August 24, 2015 on the website of the French Institut de Veille Sanitaire (InVS) . Retrieved August 24, 2015.
- ↑ Nice Matin newspaper, October 19, 2018
- ↑ Hair loss due to dengue fever? , additional text.
- ↑ TC Pierson, MS Diamond: Molecular mechanisms of antibody-mediated neutralization of flavivirus infection . In: Expert Rev Mol Med . tape 10 , 2008, p. e12 , doi : 10.1017 / S1462399408000665 , PMID 18471342 , PMC 2671962 (free full text).
- ↑ http://www.who.int/csr/resources/publications/dengue/034-47.pdf (PDF file)
- ↑ Viral hemorrhagic fevers. In: rki.de. Robert Koch Institute, November 28, 2019, accessed on March 23, 2020 .
- ^ W. Parks, L. Lloyd: Planning Social Mobilization and Communication for Dengue Fever Prevention and Control. WHO / CDS / WMC / 2. 2004, WHO, Geneva 2004.
- ↑ S. Schaper: Contribution to the use of Mesocyclops thermocyclopoides for the control of the mosquito 'Stegomyia aegypti' in Costa Rica. Dissertation Hanover, 2001, ISBN 3-8311-1668-7 .
- ^ B. Kay, SN Vu: New strategy against Aedes aegypti in Vietnam . In: The Lancet . tape 365 , no. 9459 , 2005, p. 613-617 , doi : 10.1016 / S0140-6736 (05) 17913-6 , PMID 15708107 .
- ^ A. Kroeger, A. Lenhart, M. Ochoa et al .: Effective control of dengue vectors with curtains and water container covers treated with insecticide in Mexico and Venezuela: cluster randomized trials. In: BMJ. 2006, No. 332, pp. 1247-1252.
- ^ A. Rose, M. Geier, AE Eiras, M. da Gloria Teixeira, M. das Gracas Vale Barbosa, MP Gomes Mourao: Novel mosquito traps in the fight against urban dengue - from monitoring to control. Introduction to a feasibility study in Manaus, Brazil. In: Proceedings of the XXIII International Congress of Entomology. Durban, South Africa 2008.
- ↑ Conor J. McMeniman, Roxanna V. Lane, Bodil N. Casset include: Stable Introduction of a life-shortening Wolbachia Infection into the Mosquito Aedes aegypti . In: Science . tape 232 , no. 5910 , January 2, 2009, p. 141-144 , doi : 10.1126 / science.1165326 .
- ↑ Nadine Poniewaß: Harmless breeding of mosquitoes displaces deadly conspecifics . On: Spiegel Online. dated August 25, 2011.
- ↑ Cinthia Briseño: Critics condemn tests with suicide mosquito . On: Spiegel Online from October 31, 2011.
- ^ The Oxitec approach . Quote: After an Oxitec male mosquito has successfully mated with a wild female, any offspring that result will not survive to adulthood, so the mosquito population declines. On: oxitec.com ; last accessed on November 22, 2016.
- ↑ Gene mosquito is supposed to save people . On: rp-online.de from April 24, 2012.
- ↑ Alexandra Jane Oliver: Parasite fungus is supposed to fight dengue fever . On: Spiegel Online. dated April 23, 2012.
- ^ Online Etymology Dictionary. Retrieved June 14, 2010 .
- ↑ WHO | Impact of Dengue. Retrieved August 7, 2010 .
- ↑ JB Siqueira, CM Martelli, GE Coelho, AC Simplicio, DL Hatch: Dengue and dengue hemorrhagic fever, Brazil, 1981-2002 . In: Emerging Infect. Dis. tape 11 , no. 1 , January 2005, p. 48-53 , PMID 15705322 .
- ↑ MF Oliveira, JM Galvao Araujo, OC Ferreira et al .: Two lineages of dengue virus type 2, Brazil . In: Emerging Infect Dis . tape 16 , no. 3 , March 2010, p. 576-578 , PMID 20202456 .
- ↑ Dengue fever outbreak in South and Central America. In: Blick.ch . November 21, 2019, accessed November 21, 2019 .
- ^ Office of Medical History. Retrieved August 11, 2010 .
- ^ PM Ashburn, CF Craig: Experimental investigations regarding the etiology of dengue fever. 1907 . In: J. Infect. Dis. tape 189 , no. 9 , May 2004, p. 1747-1783; discussion 1744-1746 , doi : 10.1086 / 383418 , PMID 15116315 .
- ^ Chemical and Biological Weapons: Possession and Programs Past and Present . On: James Martin Center for Nonproliferation Studies. Middlebury College , April 9, 2002, accessed November 14, 2008.
- ↑ USAMRIID: I. History of biological warfare; B. Significant events in the history of the US offensive program . : " 1970–1972 Total destruction of anti-personnel BW agent stocks and munitions were accomplished between May 10, 1971 and May 1, 1972. The BW plant facilities at PBA were decontaminated and turned over to the Food and Drug Administration. The offensive research program was also terminated in 1970 with a complete inventory of all BW material at Ft. Detrick and Dugway Proving Ground, and destruction of all items except those essential to defensive BW research. "
- ↑ Barry S. Levy, Victor W. Sidel: War and Public Health. American Public Health Association, 2000, ISBN 0-87553-023-0 , pp. 110-111, Google Books
- ^ William Blum: Killing Hope: US Military and CIA Interventions Since World War II . First Printing edition, Common Courage Press, March 1995, ISBN 1-56751-052-3 , Google Books .
- ^ R. Edelman: Dengue vaccines approach the finish line . In: Clin. Infect. Dis. 45 Suppl 1, July 2007, p. S56-S60 , doi : 10.1086 / 518148 , PMID 17582571 .
- ↑ Efficacy of a tetravalent Dengue Vaccine in Children in Latin America. In: New England Journal of Medicine.
- ↑ Vaccine against dengue fever planned by 2015 . On: derstandard.at of October 18, 2010, last accessed on October 1, 2014.
- ↑ Efficacy of a tetravalent Dengue Vaccine in Children in Latin America. In: New England Journal of Medicine.
- ↑ Bacteria make mosquitoes immune. Will the spread of dengue fever stop soon? On: bild.de on August 25, 2011, last accessed on October 1, 2014.