dialysis
As dialysis ( Greek διάλυσις dialysis , German , resolution ', detachment', 'separation' ) is a blood purification method referred to, which when renal failure is as a replacement method for use. Alongside kidney transplantation, dialysis is the most important renal replacement therapy for chronic kidney failure and one of the treatment options for acute kidney failure .
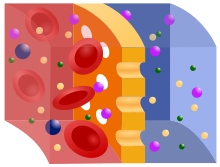
Dialysis in the real sense is the exchange of substances by diffusion through a semipermeable membrane , with dissolved molecules migrating from highly concentrated liquids (here blood / plasma) into weakly concentrated solutions (dialysis solution).
history
Thomas Graham described dialysis as a separation process in 1861. In 1913 Leonard Rowntree and John Abel developed the first hemodialysis machine ; they called it (as "vividiffusion apparatus" and as an artificial kidney English : "artificial kidney").
Hemodialysis (HD)
The world's first "blood washing" via semipermeable membranes in humans wascarried outin 1924 by Georg Haas in Giessen. The breakthrough, however, was only brought Willem Kolff in 1945 in Kampen (Netherlands) with his drum dialysis machine with cellophane -hoses as a dialysis membrane. This membrane allowed a controlled blood purification of defined amounts of substance. A technically superior parallel development by Nils Alwall in Lund (Sweden) in 1946 also allowed edema fluid to be flushed out of the lungs and tissue ( ultrafiltration ). Other pioneers were Erich Streicher and Curt Moeller .
Peritoneal dialysis (PD or peritoneal dialysis)
At the end of the 19th century, the foundations for peritoneal dialysis (PD) were laid by Georg Ganter . In 1923 he carried out the first clinical peritoneal dialysis in Würzburg. Stephen Rosenak and P. Sewon developed a metal catheter for continuous peritoneal lavage in the 1920s. In 1959,long-term use became possiblefor the first time with the help offlexible plastic catheters made of polyethylene . The first automated peritoneal dialysis took place in the early 1960s. Today's PD has made its breakthrough thanks to indwelling catheters made of silicone rubber. In 1975, Popovich and Moncrief (Texas), the first signs of the so-called continuous ambulatory peritoneal dialysis (CAPD, continuous ambulatory peritoneal dialysis, s. U.). At the end of the 1970s, the Oreopoulos working group in Toronto presented the current form of CAPD.
Dialysis procedure
On the one hand, a distinction is made between extracorporeal (outside the body) and intracorporeal (inside the body) procedures. On the other hand, a distinction is also made based on where the dialysis takes place: in a (dialysis) center or at home. The most common extracorporeal procedure is hemodialysis (in the center). The non-extracorporeal procedure is peritoneal dialysis (at home).
Since extensive knowledge of the possible side effects is required to carry out the procedure, these are usually used by nephrologists or intensive care physicians.
Center dialysis
Hemodialysis (HD)
Hemodialysis is the exchange of dissolved substances via a semipermeable membrane ( dialyzer ) by diffusion along a concentration gradient between blood and dialysate, with additional fluid being withdrawn by means of ultrafiltration through a hydrostatic pressure difference . In hemodialysis, the principle of equalizing the concentration of small-molecule substances in two liquids that are separated by a semipermeable membrane ( osmosis ) is used. Separated from the filter membrane, on one side is the blood with electrolytes such as potassium and phosphate as well as with the urinary substances (e.g. creatinine , urea, uric acid ). On the other side of the membrane there is a low-germ, prepared solution ( dialysis fluid ), the water of which was prepared by reverse osmosis during online preparation , which does not contain any waste products and a proportion of electrolytes (e.g. potassium ions from 0 to 4 mmol / l and calcium ions from 1.5 to 1.75 mmol / l). The semipermeable filter membrane (dialysis membrane) between blood and dialysis solution has pores that allow small molecules such as water, electrolytes and urinary substances to pass through, but hold back large molecules such as proteins and blood cells. In addition, metabolic acidosis can be compensated for by bicarbonate during hemodialysis, which results in better circulatory stability and fewer subjective complaints than the earlier acetate buffering, which was less expensive in terms of equipment.
Basic requirements for carrying out a four to five hour hemodialysis are adequate circulatory stability, adequate blood volume and good (arterial, venous) access to the patient. The latter is achieved through the surgical application of an arteriovenous shunt (formerly an external Scribner shunt, now usually an internal Cimino shunt ) on the forearm or upper arm. Vascular prostheses (Goretex) are also used for problematic blood vessels. In very rare cases, the shunt is placed on the thigh or between the subclavian artery and the subclavian vein (also called collier or décolleté shunt because of its location), with or without the use of artificial vessels. Another option is to insert a dialysis catheter into a suitably large body vein for acute dialysis ( Shaldon catheter , usually via the neck ( internal jugular vein ) or through the subclavian vein, rarely via the groin ( femoral vein )) only in multimorbid patients with a very poor vascular situation or severe heart failure ( Demers atrial catheter or Hickman catheter ).
During a treatment, blood is pumped out of the patient via the patient access, guided past the dialysis membrane in the dialyzer (filter) and then returned to the patient after cleaning. Toxins (metabolic degradation products) and low molecular weight substances (membrane-permeable substances) are transported from the blood by diffusion through the membrane to the other side of the filter into the dialysis solution (dialysate) due to the concentration gradient and thereby removed. Fresh dialysate is constantly flowing through the dialyzer (approx. 500 ml / min). The hemodialysis treatment is usually carried out for around four to five hours (night dialysis up to eight hours) per treatment and at least three times a week (depending on body weight, residual kidney function, cardiac output). Patients on home hemodialysis avoid the problematic longer treatment interval on the weekend and dialyze more often, usually every two days or daily.
Chronic renal failure patients also often experience overhydration . The excess water is removed from the blood by applying a pressure gradient (negative pressure on the dialysate side). This controls how much fluid is withdrawn from the blood, thus mimicking the natural diuretic function of the kidney. The withdrawal of fluids is limited by the fact that in the body the fluid (also applies to the toxins) cannot diffuse into the bloodstream as quickly as desired in order to compensate for the fluid loss , which threatens a life-threatening drop in blood pressure . In addition, different tissues release fluid at different rates. For example, muscles cramp even though there is still too much fluid in the body. These effects limit the amount of fluid that can be withdrawn through dialysis and patients are therefore not allowed to drink freely. On the other hand, since many patients suffer from constant strong thirst due to the accumulation of urinary substances in the body , the small amount allowed to drink (remaining excretion in 24 hours plus 500 ml) is often perceived as stressful.
An extension of the dialysis time is mainly possible with the daily home hemodialysis (HHD) and enables a more even therapy. Since the dialysis effectiveness is highest in the first half of treatment, it is medically sensible, but rarely practiced, to carry out frequent but short dialyses instead of rare, longer dialyses. Daily hemodialysis combines the advantages of peritoneal dialysis (dialysis every day) and conventional hemodialysis (high effectiveness). For patients who do not have the option of home hemodialysis, night dialysis is available in the center to extend the dialysis time. Some patients can sleep during dialysis, sometimes only after a period of getting used to it, but others not at all. Due to the practicality and patient acceptance, but also because the health insurances only pay flat rates per patient for treatment, dialysis more frequently than three times a week is not offered for patients who have no possibility of HHD. Exceptions to this are additional dialyses in the event of overhydration in order to reduce the patient's “dry weight”, or the phase of dialysis intake ( “andialysis” ), in which the patient may be dialyzed daily for a week.
Dialysis patients are often iron deficient . This is caused by the loss of blood during dialysis and by reduced iron absorption in the intestine. Therefore, an intravenous iron supplement, e.g. B. iron gluconate , injected. To avoid iron overload ( hemochromatosis ), it is advisable to regularly check the concentration of ferritin in the serum. Many dialysis patients receive erythropoietin analogues to stimulate blood formation .
Intermittent peritoneal dialysis (IPD)
Intermittent peritoneal dialysis is performed 3–4 times a week in a dialysis facility. In a period of about 8 hours, about 30-40 l of dialysis solution are used in about half an hour individual phases. In terms of time, IDP is the most closely comparable form of peritoneal dialysis with machine hemodialysis, in which the dialysis is directed and monitored by medical staff.
Home dialysis
Home hemodialysis
With home hemodialysis, the patient independently performs the dialysis treatment with the dialysis machine at home three to six times a week. He can also be supported by a helper - usually his partner. The patient's apartment should have sufficient space in which the dialysis machine can be set up, ideally in a separate room.
Peritoneal dialysis (PD)
Peritoneal dialysis (PD) is also known under the term peritoneal dialysis. There are different PD methods, e.g. B. the method of APD (continuous cyclical PD, see below) carried out with devices or the manual CAPD (continuously ambulatory peritoneal dialysis, continuous ambulatory peritoneal dialysis, see below). The IPD (intermittent PD, see above) is part of the center dialysis. The choice of procedure depends, among other things, on the transport properties of the peritoneum (see below) and the patient's underlying disease.
PD and HD are equivalent dialysis procedures. Scientific data from the USA and Europe show a better survival for PD patients in the first 3 years and a similar long-term survival as for HD patients. Nevertheless, PD is used in only 5–10% of all patients in Germany. The quality of life of PD patients is rated significantly higher, because on the one hand PD patients can organize their time more individually, on the other hand they have greater spatial flexibility and independence. Employment, hobbies, food and fluid intake are significantly less restricted.
The peritoneum is a serous skin that lines the abdominal cavity and envelops large parts of the intestine. It is a tissue with relatively good blood circulation, which also plays an important role in the body's immune system, for example.
Due to its special structure, the peritoneum can also be used as a “filter membrane”: a tube ( catheter ) is implanted into the patient's abdominal cavity. A dialysis solution is filled into the abdominal cavity via this catheter and left there for several hours (e.g. with CAPD) or for 20-30 minutes (e.g. IPD). The small molecular substances can now pass from the blood via the capillary vessels of the peritoneum into the dialysis solution, since there is a concentration gradient. If fluid (water) is to be withdrawn from the body in this way, the dialysis solution must have a higher content of soluble substances than the blood. For this it is enriched with glucose , dextrins or other substances (experimentally). The dialysis solution must be drained off after a certain period of time (usually around four to six hours for CAPD) and replaced with a fresh one. In contrast to the artificial membrane in blood dialysis, the peritoneum is also quite permeable for proteins, which leads to a relevant loss of protein. Advantages of this procedure are: the longer maintenance of the residual kidney function, the fewer complications of dialysis access and the protection of the circulatory system, which enables renal replacement therapy even in very old people and people with heart disease. Another possible advantage is that patients are largely independent of a dialysis center: if they are suitable, dialysis can be carried out at home, and holiday trips are also less complicated, as the materials are delivered directly to the holiday destination and there is no need to make appointments with a holiday dialysis center. A disadvantage of peritoneal dialysis is the risk that the abdominal cavity will be infected with pathogenic germs with possible contact with the environment, resulting in peritonitis . In contrast to peritonitis of other causes, which are a serious and often fatal disease, CAPD-associated peritonitis is easy to treat, can often even be treated on an outpatient basis and has a low mortality rate. To do this, an antibiotic is given directly into the abdominal cavity with the dialysis solution. However, repeated peritonitis leads to a deterioration in the effectiveness of peritoneal dialysis. Patients must therefore work very carefully when changing solutions. Modern catheter systems enable the tip and the interior of the catheter to be kept sterile . The procedure is limited because of its comparatively lower effectiveness due to body weight and residual kidney function - if the body mass is larger and residual kidney function is low, PD is less suitable. In the course of using, in particular, stronger glucose-containing dialysis solutions over several years, changes in the peritoneum occur in some patients, which, with the same glucose concentration, result in a decreasing or even negative filtration performance. Then, in order to avoid the formation of edema and high blood pressure, the concentration of glucose in the dialysis solution must be increased and the residence time of the solution in the abdominal cavity reduced. Due to the changes in the peritoneum, which in the vast majority of cases eventually lead to a so-called ultrafiltration failure and thus insufficient detoxification and drainage, peritoneal dialysis is always a temporary procedure. Young people have had good experiences with peritoneal dialysis as a “bridge to transplant”. The ongoing glucose uptake from the dialysis solution and the continuous loss of protein can also lead to the development or worsening of diabetes mellitus. Nevertheless, studies have shown that diabetics, in particular, benefit from peritoneal dialysis in the first few years of mandatory dialysis.
Automated Peritoneal Dialysis (APD)
Automated peritoneal dialysis (APD) is a home therapy procedure that is usually carried out during the night and in which the bag is changed automatically by a machine.
Continuous ambulatory peritoneal dialysis (CAPD)
In contrast to the APD, with the CAPD the bag change is carried out by the patient himself or with the help of family members or nursing services during the day by hand at home (or at work).
Special forms of hemodialysis
Hemofiltration
Hemofiltration is a pure ultrafiltration and replacement by electrolyte solution. With hemofiltration (filtering off plasma water with substitution), fluid is withdrawn from the blood without using a rinsing solution (dialysate). Due to a pressure gradient (transmembrane pressure) applied to the filter membrane via a pump, plasma fluid is convectively withdrawn from the blood via the membrane (ultrafiltration). This transmembrane flow also removes all substances that can pass through the filter. This enables slow detoxification and, if necessary, a rapid change in volume in the patient's body. The withdrawn liquid is replaced by an electrolyte solution (substituate) that is individually adapted. It is a machine process.
Spontaneous filtration is a process in which blood flows spontaneously from artery to vein, plasma fluid is squeezed out by the intrinsic pressure of an artery in the patient's circulation (without a pump) and replaced by an electrolyte solution: Continuous arteriovenous hemofiltration (CAVH). This method, which was developed in 1977 by Fritz Scheler's colleague Peter Kramer in Göttingen, was ineffective and dependent on blood pressure, was soon replaced by pump-driven continuous venovenous hemofiltration (CVVH), which in turn was expanded by combining it with dialysis for continuous venovenous hemodiafiltration (CVVHDF) . These procedures are used in intensive care units to treat patients with acute kidney failure.
In principle similar to CAVH and CVVH, the procedures are continuous arteriovenous hemodialysis (CAVHD) and continuous venovenous hemodialysis (CVVHD).
Hemodiafiltration
Hemodiafiltration is an extracorporeal blood purification process in which hemodialysis and hemofiltration are used in combination. This method is used in particular in the case of chronic renal insufficiency and enables both low and medium molecular weight substances to be removed with the controlled replacement of the ultrafiltrate with physiological electrolyte solution (diluate). The replacement solution is added to the blood either before or after the dialyzer and removed again in the dialyzer ( ultrafiltration ). This allows a higher transmembrane flow to be created, which leads to the more effective removal of toxins.
Hemoperfusion
Hemoperfusion is not a kidney replacement method, but a treatment method for acute poisoning and is only carried out by clinics specially set up for this purpose. The blood is pumped through adsorbents (e.g. activated charcoal or exchanger resins), which can remove some fat-soluble or protein-bound substances (e.g. certain overdosed drugs, organic solvents, insecticides, fungal toxins) from the blood. The method is only established for a comparatively small number of substances.
Start of dialysis therapy (blood wash)
The decision as to whether and when dialysis treatment or hemofiltration is necessary in patients with kidney failure depends on various factors, which can be acute or chronic.
- Acute indications for starting dialysis treatment:
- Acute kidney failure, e.g. B. during sepsis ("blood poisoning"), after a trauma (accident) or after major surgery
- Hyperkalemia
- Metabolic acidosis
- Overhydration (usually manifests as pulmonary edema with shortness of breath)
- Uremic serositis, such as pericarditis , and uremic encephalopathy
- Acute poisoning with dialyzable substances such as lithium or acetylsalicylic acid
- Chronic causes for starting dialysis treatment:
- Symptomatic kidney failure
- Low Glomerular Filtration Rate (GFR), most often with a GFR lower than 10-15 ml / min / 1.73 m²
- Otherwise uncontrollable hyperphosphataemia or uremia ( urea -N greater than approx. 100 mg / dl)
Dialysis is indicated when it cannot be avoided with diet or medication. In this way, the plasma level of the harmful substances that are phased out in urine can often be reduced.
See also
literature
- Hemodialysis Journal . Bulletin of the interest group of dialysis patients Saar eV Vol. 1, 1973/1974 - Vol. 3, 1975, ZDB -ID 224632-6 , continued as: The dialysis patient. Official organ of the Bundesverband Niere eV Vol. 1, 1976 - 32, 2007, ISSN 0724-0252 , continued as: The kidney patient . Official organ of the Bundesverband Niere eV vol. 33, 2008 - ongoing , ISSN 1865-8822 .
- Diatra magazine (made up of "dialysis" and "transplantation")
- Gerd Breuch, Willi Servos: Dialysis for Beginners. Elsevier, Urban and Fischer, Munich a. a. 2007, ISBN 978-3-437-27790-0 .
- Günther Schönweiß: Dialysis Primer 2. Plea for individual dialysis. 2nd, completely revised and enlarged edition. abakiss, Bad Kissingen 1996, ISBN 3-931916-01-4 .
- Kidney Int . Suppl. 2008 Apr; Dialysis outcomes in Colombia (DOC) study: a comparison of patient survival on peritoneal dialysis vs hemodialysis in Colombia. Sanabria M1 et al.
- Perit Dial Int. 2014 Jan 2. Better Outcomes Of Peritoneal Dialysis In Diabetic Patients In Spite Of Risk Of Loss Of Autonomy For Home Dialysis. Cotovoio, P et al.
- Steffen Geberth & Rainer Nowack: Practice of dialysis. Springer, 2nd edition, Berlin & Heidelberg 2014. ISBN 978-3-642-41207-3 (print); ISBN 978-3-642-41208-0 (eBook),
- Amitava Majumder, Anne Paschen: Medical working techniques. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 29–93, here: pp. 60–66 ( dialysis ).
Web links
- Federal Association of Kidneys V. Self-help umbrella organization. Retrieved January 31, 2009 .
- Association of German Kidney Centers (DN) e. V. Accessed January 31, 2009 .
- The blood flow on the dialysis machine (video). Retrieved January 31, 2009 .
Individual evidence
- ^ Manfred Vasold: Dialysis. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 304 f .; here: p. 304.
- ↑ Volkmar Heinze : Dialysis. In: Hans Joachim Sarre : Kidney Diseases. 4th edition. Georg Thieme Verlag, Stuttgart 1976, ISBN 3-13-392804-X , p. 559.
- ↑ Amitava Majumder, Anne Paschen: Medical working techniques. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 29-93, here: pp. 62-66 ( dialysis method ).
- ↑ Amitava Majumder, Anne Paschen: Medical working techniques. In: Jörg Braun, Roland Preuss (Ed.): Clinic Guide Intensive Care Medicine. 9th edition. Elsevier, Munich 2016, ISBN 978-3-437-23763-8 , pp. 29–93, here: pp. 62–66 ( dialysis method ), in particular p. 62.
- ↑ a b Renal replacement therapy: CORETH research project provides new insights into the choice of procedure , PM of the German Society for Nephrology of October 18, 2017, accessed on December 14, 2018
- ↑ Dialysis - What is it? , Apotheken Umschau, accessed on December 14, 2018
- ↑ Jay B Wish, George R Aronoff, Bruce R Bacon, Carlo Brugnara, Kai-Uwe Eckardt: Positive Iron Balance in Chronic Kidney Disease: How Much is Too Much and How to Tell? In: American Journal of Nephrology . tape 47 , no. 2 , 2018, ISSN 1421-9670 , p. 72-83 , doi : 10.1159 / 000486968 , PMID 29439253 .
- ↑ Jay B Wish, George R Aronoff, Bruce R Bacon, Carlo Brugnara, Kai-Uwe Eckardt: Positive Iron Balance in Chronic Kidney Disease: How Much is Too Much and How to Tell? In: American Journal of Nephrology . tape 47 , no. 2 , 2018, ISSN 1421-9670 , p. 72-83 , doi : 10.1159 / 000486968 , PMID 29439253 .
- ^ Iain C Macdougall, Claire White, Stefan D Anker, Sunil Bhandari, Kenneth Farrington: Intravenous Iron in Patients Undergoing Maintenance Hemodialysis . In: New England Journal of Medicine . tape 380 , no. 5 , January 31, 2019, ISSN 0028-4793 , p. 447–458 , doi : 10.1056 / NEJMoa1810742 ( nejm.org [accessed March 4, 2019]).
- ↑ Eric D. Weinhandl et al .: Propensity-Matched Mortality Comparison of Incident Hemodialysis and Peritoneal Dialysis Patients . In: Journal of the American Society of Nephrology: JASN . tape 21 , no. 3 , March 2010, p. 499–506 , doi : 10.1681 / ASN.2009060635 , PMID 20133483 , PMC 2831857 (free full text).
- ↑ Heaf JG et al .: Relative Survival of Peritoneal Dialysis and Hemodialysis Patients: Effect of Cohort and Mode of Dialysis Initiation . In: PLoS One . March 2014, doi : 10.1371 / journal.pone.0090119 .
- ↑ MW Van de Luijtgaarden et al .: Trends in dialysis modality choice and related patient survival in the ERA-EDTA Registry over a 20-year period . In: Nephrol Dial Transplant . tape 31 , no. 1 , January 2016, p. 120-128 , doi : 10.1093 / ndt / gfv295 , PMID 26311215 .
- ↑ B. Waldum-Grevbo et al .: Impact of initial dialysis modality on mortality: a propensity-matched study. In: BMC Nephrology: 179 . tape June 16 , 2015, p. 179 , doi : 10.1186 / s12882-015-0175-5 , PMID 26519164 , PMC 4628291 (free full text).
- ^ R. Saran, B. Robinson, KC Abbott et al .: US Renal Data System 2017 Annual Data Report: epidemiology of kidney disease in the United States . In: American Journal of Kidney Diseases . tape 71 , 3 (suppl 1), 2018, p. 1–673 , doi : 10.1053 / j.ajkd.2018.01.002 , PMID 29477157 .
- ↑ Jahn M et al .: New indications for peritoneal dialysis . In: Nephrologist . tape 12 , 2017, p. 6-13 .
- ↑ Kidney Int Suppl. 2008 Apr; Dialysis outcomes in Colombia (DOC) study: a comparison of patient survival on peritoneal dialysis vs hemodialysis in Colombia. Sanabria M1, Muñoz J, Trillos C, Hernández G, Latorre C, Díaz CS, Murad S, Rodríguez K, Rivera A, Amador A, Ardila F, Caicedo A, Camargo D, Díaz A, González J, Leguizamón H, Lopera P, Marín L, Nieto I, Vargas E.
- ^ Ann Clin Microbiol Antimicrob. 2006; 5: 6; Treatment and outcome of CPD-associated peritonitis. Troidle L, Finkelstein F
- ↑ Kidney Int Suppl. 2008 Apr; Dialysis outcomes in Colombia (DOC) study: a comparison of patient survival on peritoneal dialysis vs hemodialysis in Colombia. Sanabria M1 et al.
- ↑ W. Koller, TH Luger, Ch. Putensen, G. Putz: Blood purifying procedures in intensive care medicine. In: J. Kilian, H. Benzer, FW Ahnefeld (ed.): Basic principles of ventilation. Springer, Berlin a. a. 1991, ISBN 3-540-53078-9 , 2nd, unchanged edition, ibid. 1994, ISBN 3-540-57904-4 , pp. 404-419; here: p. 408.
- ↑ Michael Heck, Michael Fresenius: Repetitorium Anaesthesiologie. Preparation for the anesthesiological specialist examination and the European diploma in anesthesiology. 3rd, completely revised edition. Springer, Berlin / Heidelberg / New York et al. 2001, ISBN 3-540-67331-8 , p. 804.
- ↑ Amitava Majumder, Anne Paschen: Medical working techniques. 2016, p. 62 f.
- ^ Hans Joachim Sarre : Kidney diseases , 4th edition, Georg Thieme Verlag, Stuttgart 1976, ISBN 3-13-392804-X , p. 603.