Cardiac output
The cardiac output ( CO , English cardiac output CO ) is the volume of blood that each time the heart is pumped ( flow ). The usual unit of measurement is liters per minute , which is then referred to as the cardiac output ( HMV ), formerly also called minute volume for short . The divided for better interindividual comparability through the body surface is called cardiac output cardiac index (English cardiac index ). The cardiac output was first mentioned scientifically by William Harvey , who provided proof of the existence of the blood circulation with his calculation of the half-hourly volume published in 1628 . A cardiac output that is too small is considered to be the cause of heart failure .
Physiology and calculations
In the narrower sense of the word, cardiac output describes the volume pumped into the body's circulation per unit of time ; this is sometimes illustrated by the term body time. Since the left and right ventricles of the heart act in series in mammals, the volume ejected into the pulmonary circulation per time is the same as the time volume on average over time. A very close look at the vascular supply to the lungs and heart reveals that the body time volume is about 1% greater than the lung time volume. With a right-left shunt , the body time volume is (notably) greater than the lung time volume; with the left-right shunt, the body time volume is smaller than the lung time volume. In general, the equation cardiac output + left-right shunt time volume = lung time volume + right-left shunt time volume applies. This fundamental equation is largely unknown; the word lung time volume alone is rarely used. The effective lung flow volume is sometimes smaller (or larger) than the total lung flow volume , which is also referred to as the actual small-circulatory minute volume or lung time volume.
The cardiac output
- is the lung time volume plus right-left shunt volume flow minus left-right shunt volume flow. It
- can be calculated by multiplying the heart rate by the heart rate. It is also the cardiac output
- the quotient of blood pressure and peripheral resistance ,
- the quotient of cardiac output and blood pressure (the cardiac output is the product of cardiac work and heart rate) as well as
- the square root of the quotient of cardiac output and peripheral resistance.
When determining the CO with the Swan-Ganz catheter by means of thermodilution, the Stewart- Hamilton equation is used for the calculation (see number 2 below).
Occasionally, attempts are made to favorably influence heart failure by creating an artificial left-right shunt at the atrial level ( e.g. balloon atrioseptostomy ). Because of the formula CO + LRSV = LZV + RLSV, an increase in cardiac output is not to be expected from such measures (as LRSV enlargement). Therefore, such surgical interventions are considered palliative .
Normal values
- At rest, the cardiac output in healthy adults is about 4.5-5 l / min. The lower normal value for the heart index is 2.5 (l / min) / m².
- Under stress, the CO can be increased up to six times and then be up to 30 l / min, in individual cases even more. In trained adult athletes, the cardiac output increases under maximum load up to 36 l / min. The former Spanish cyclist and multiple Tour de France winner Miguel Indurain is repeatedly said to have had a cardiac output of 50 l / min under maximum load.
Measurement
Cardiac output can only be measured indirectly in clinical practice. There are various methods of doing this:
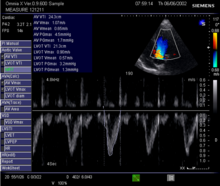
- In echocardiography: It can easily be calculated from the stroke volume and the heart rate: HMV = heart rate × stroke volume . The stroke volume and heart rate can be estimated from echocardiography. The diameter of the left ventricular outflow tract (LVOT) is measured in the 2D image and an area is calculated from this with the help of the circular area and by bypassing the PW Doppler curve in the LVOT, the Velocity Time Integral (VTI), and the heart rate (HF) multiplied. HMV = π × LVOT² / 4 × VTI × HF .
- Thermodilution is somewhat more complex. A defined amount of cold liquid is injected and the temperature profile of the blood is then recorded using a thermal probe. The HMV can be calculated using the speed of the temperature normalization. One way of putting this into practice is the Swan-Ganz catheter . This is a catheter that is advanced through a large vein in the neck (usually internal jugular vein or subclavian vein) through the right half of the heart to the pulmonary artery. For example, with the help of an integrated heating coil, the CO can also be determined continuously (i.e. without liquid being injected in the meantime).
- Dye dilution processes work similarly. A cardiac catheter is also required here.
- Model-based methods calculate the HMV continuously from the arterial blood pressure curve measured by an arterial catheter after calibration by another method (for example thermodilution). An example of this is the PiCCO (Pulscontour Continuous Cardiac Output) system from Pulsion (R), which, compared to the Swan-Ganz catheter, offers the advantage of being a significantly less invasive procedure, as there is no catheter through the heart to the inside the pulmonary artery needs to be advanced.
- The lung time volume (in l / min) can be calculated according to Fick's principle by dividing the oxygen uptake (in ml / min), which can be determined using a breathing mask, by the difference in the oxygen content of the arterial and central venous blood (in ml / l) becomes. After the resting cardiac output in humans had previously been estimated at three to twelve liters, the more precise method by Adolf Fick (1829–1901) became the reference method for determining HMV for decades.
- With the help of nuclear cardiology (and nuclear pulmology), the HMV (or the identical lung time volume ) can be determined by nuclear medicine .
- The HMV can also be determined with the help of the magnetic resonance examination.
- Another method is impedance cardiography .
- Something similar is expected from whole-body bioimpedance technology .
- Philipp Broemser and Otto Friedrich Ranke recommended sphygmography in 1930 and 1933 for bloodless determination of stroke volume . The cardiac output is obtained by multiplying it by the heart rate .
- A similar (sphygmometric) method was the Wezler- Böger method based on Otto Frank's research.
- The ballistocardiogram is also only of medical historical importance . If the patient is suspended in a lying position, the stroke volume is calculated from the recoil of the blood ejected from the two heart chambers .
- The elongation ballistocardiogram is also completely out of date. During the expulsion phase of the blood from the heart, the patient's center of gravity shifts towards the head. If you add the mass of the bed floating on a mercury bath to the patient's weight, you can use a complicated formula to calculate the stroke volume and thus the cardiac output.
- In contrast to these historical processes, there are two other modern processes. They too are not fully developed, still imprecise and of questionable clinical relevance . Mention should be made here of the electrical cardiometry for determining the cardiac output and
- in addition, the method of bioreactance also for determining cardiac output and peripheral resistance . The use of computers to determine stroke volume and thus also the HZV was described by Rudolf Groß as early as 1969 .
- The cardiac output of artificial hearts (circulatory support system) is determined device-specifically depending on the mechanics used.
Medical importance
The cardiac output depends on the heart rate, heart rhythm, preload , afterload and contractility of the heart. For practical reasons, the value of the ejection fraction (the percentage of stroke volume in the highest volume of the left ventricle at the end of diastole ) has become more common for assessing the pump function , since it can be read directly from the echocardiography . The cardiac output, on the other hand, is determined in more complex cardiac catheter examinations .
Decreased cardiac output
A reduced cardiac output is found with reduced pumping capacity of the left or right ventricle. Heart valve diseases can also reduce cardiac output, as can an underactive thyroid ( hypothyroidism ). The reduction in cardiac output during a heart attack depends on the severity of the infarction.
Increased cardiac output
A tachycardia increases the cardiac output. An increased cardiac output is found in fever , hyperthyroidism and anemia . Even in hyperdynamic shock states, such as B. septic shock , the cardiac output can be increased, although there may be a lower perfusion of organs, which is due to a decrease in peripheral resistance . During pregnancy , there is also an increased cardiac output. The reason for this is the increase in the amount of blood during pregnancy by around 1½ liters in order to ensure the supply of the placenta and uterus .
history
William Harvey (1578–1657) made the first calculations of the HZV. He determined a stroke volume in humans of only half an ounce (= 18 ml) and thus approximately a cardiac output of 1.15 l / min. In 1870 Adolf Fick determined the HZV using the Fick principle named after him. Numerous alternatives and improvements have then been proposed.
Otto Klein (1891–1968) published a paper on August 1, 1930 in the Münchener Medizinische Wochenschrift on the determination of minute volume according to Fick's principle. To do this, he had to provide his patients at the German University in Prague with a right heart catheter using the method of Werner Forßmann ( first practiced by Werner Forßmann in spring 1929 in a self- experiment) . Otto Klein measured the differences in oxygen concentration between the venous and arterial blood and determined cardiac output in his first three patients in this way (see method number 5 above) of 4.46 l / min, 6.67 l / min and 4 , 20 l / min. However, Klein's superior Wilhelm Nonnenbruch showed no interest in this research. As a Jew , Otto Klein had to emigrate to Buenos Aires in 1938 . But in 1933 he went to Boston to present his method there; here too, however, he only met with rejection. It was only twelve years later in the USA that Cournand and Richards recognized the central importance of this determination of cardiac output.
See also
literature
- Reinhard Larsen: Anesthesia and intensive medicine in cardiac, thoracic and vascular surgery. 5th edition. Springer-Verlag, Berlin / Heidelberg / New York a. a. 1999, ISBN 3-540-65024-5 , pp. 218 f.
Individual evidence
- ↑ The blood volume per unit of time meant here (unit: ml / min; SI unit l / s) must not be confused with the absolute total blood volume (SI unit: liter) of humans. If, for example, the determination of the amount of blood was previously written in historical writings , this possibility of confusion with the CO must be considered.
- ↑ The CO must not be confused with the blood flow rate (SI unit: m / s).
- ↑ Fritz Lange: Textbook of diseases of the heart and the blood flow path. Ferdinand Enke Verlag, Stuttgart 1953, p. 82.
- ↑ HMV and HZV are used synonymously, but also listed independently in specialist books (Examples: Bernd Heublein (Ed.): Heart, circulatory and vascular diseases. Volume 1, Part 1, Gustav Fischer Verlag , Stuttgart 1985, ISBN 3-437 -10806-9 , p. 798 f., And also Walter Siegenthaler , W. Vetter, A. Schrey (eds.): Hypertonie. Verlag für angewandte Wissenschaften, Munich 1980, ISBN 3-922251-73-0 , p. 283 .) - The pumped blood volume is divided by the time required for this.
- ^ William Harvey: Exercitatio anatomica de motu cordis et sanguinis in animalibus. SG Fitzer, Frankfurt 1628.
- ^ Gisela Teichmann: William Harvey and the cardiac output. In: internal medicine. Volume 19, No. 3, 1992, pp. 94-96.
- ^ Wilhelm Jakob Rutishauser , in: Otto Martin Hess, Rüdiger RW Simon (Ed.): Cardiac Catheters - Use in Diagnostics and Therapy , Springer-Verlag , Berlin / Heidelberg 2000, ISBN 3-642-62957-1 , p. 17.
- ^ Robert Franz Schmidt , Florian Lang, Manfred Heckmann (eds.): Physiology of humans . 31st edition. Springer Medizin Verlag, Heidelberg 2010, ISBN 978-3-642-01650-9 , p. 620 .
- ↑ Wilhelm Jakob Rutishauser, at the place indicated, p. 17.
- ↑ Ekkehart Koehler: One and two-dimensional echocardiography with Doppler technique. 4th edition. Ferdinand Enke Verlag , Stuttgart 1990, ISBN 3-432-91514-4 , p. 74, correctly calculates a right-left shunt "from the difference between the cardiac output in the area of the aortic valve and that of the pulmonary valve."
- ^ Wilhelm Nonnenbruch : Diseases of the circulation , in: Textbook of internal medicine, 4th edition, Springer-Verlag, 2 volumes, volume 1, Berlin 1939, pp. 327-460. Quotation on page 328: "Minute volume of the heart, which is the same as the flow rate of the lungs". With the "minute volume of breathing", however, he describes ventilation (ventilation) and not perfusion (blood flow) of both lungs in the same place.
- ^ Myron G. Sulyma: Dictionary of Cardiology. Volume 3: LQ. Medikon, Munich 1983, ISBN 3-923866-07-0 , Munich 1984, p. 442.
- ^ Hermann Josef Schieffer : Arterial hypertension. Karl Thiemig Verlag, Munich 1983, OCLC 634917262 , p. 11.
- ↑ D. Kleinknecht et alii: Transplantation, Nephrectomy and Hypertension , in: Karl Klütsch, Ernst Wollheim, Hans-Jürgen Holtmeier (Ed.): Die Niere im Kreis , Georg Thieme Verlag, Stuttgart 1971, ISBN 3-13-468201-X , P. 219. Here the total peripheral resistance (TPR) is defined as the quotient of the mean arterial pressure (MBP) and the cardiac output CO.
- ↑ Reinhard Larsen: Anesthesia and intensive medicine in cardiac, thoracic and vascular surgery. 5th edition. Springer-Verlag, Berlin / Heidelberg / New York a. a. 1999, ISBN 3-540-65024-5 , pp. 130-135 f.
- ↑ Roman Pfister, Christos Iliadis: Atrial flow regulator: therapy option for heart failure , in: "Forum Sanitas", number 2/2020, pp. 16-18.
- ^ Wilhelm Nonnenbruch : Diseases of the circulation , in: Textbook of internal medicine , 4th edition, Springer-Verlag, 2 volumes, volume 1, Berlin 1939, pp. 327-460; Quote on page 329: "With heavy muscle work, the minute volume can increase by 600% to 25 liters."
- ^ Walter Bleifeld, Christian W. Hamm: Heart and circulation. Springer-Verlag, Berlin / Heidelberg / New York 1987, ISBN 3-540-17931-3 , p. 22 f.
- ↑ Adolf Fick : About the measurement of the blood quantum in the heart ventricles. In: Negotiations of the Physico-Medical Society of Würzburg. New episode 2, XVI, 1872.
- ^ Gisela Teichmann: William Harvey and the cardiac output. 1992, p. 95.
- ↑ Wolfgang Trautwein , Otto H. Gauer , Hans-Peter Koepchen : Heart and circulation. (= Human physiology. Volume 3). Urban & Schwarzenberg , Munich / Berlin / Vienna 1972, p. 303.
- ↑ Fritz Lange: Textbook of diseases of the heart and the blood flow path. Ferdinand-Enke-Verlag, Stuttgart 1953, pp. 61 to 67.
- ↑ Wolfgang Trautwein, Otto H. Gauer, Hans-Peter Koepchen: Heart and circulation. (= Human physiology. Volume 3). Urban & Schwarzenberg, Munich / Berlin / Vienna 1972, p. 303.
- ↑ Wolfgang Trautwein, Otto H. Gauer, Hans-Peter Koepchen: Heart and circulation. (= Human physiology. Volume 3). Urban & Schwarzenberg, Munich 1972, ISBN 3-541-05411-5 , pp. 303 and 304.
- ^ Rudolf Gross : Medical Diagnostics. Springer-Verlag, Berlin / Heidelberg / New York 1969, p. 137.
- ↑ Georg Sabin: The cardiogenic shock. Kohlhammer Verlag , Stuttgart / Berlin / Cologne / Mainz 1984, ISBN 3-17-008618-9 , p. 17.
- ↑ Georg Sabin: The cardiogenic shock. Kohlhammer Verlag, Stuttgart / Berlin / Cologne / Mainz 1984, ISBN 3-17-008618-9 , p. 16.
- ↑ Cardiac output during pregnancy
- ↑ Peter Wiench: About important doctors in history. (= Special print, “The Great Doctors”. Volume I). Droemersche Verlagsanstalt , Munich 1982, ISBN 3-426-03919-2 , p. 175.
- ↑ Otto Klein : To determine the circulatory minute volume in humans according to Fick's principle (extraction of mixed venous blood by cardiac sounding). In: Munich Medical Weekly . Volume 77, August 1, 1930, pp. 1310–1352.