Patellar fracture
| Classification according to ICD-10 | |
|---|---|
| S82 | Fracture of the lower leg, including the upper ankle |
| S82.0 | Fracture of the patella, kneecap |
| ICD-10 online (WHO version 2019) | |
As a patellar fracture in is Unfallheilkunde of breaking the kneecap called. This fracture usually results from a fall or direct impact with the kneecap with the knee bent. These are mostly transverse or debris fractures, often with considerable displacement of the fragments. With the exception of the very rare longitudinal fracture without displacement, patellar fractures must be treated consistently; conservative treatment with immobilization is rarely sufficient . Surgical treatment is usually required, as an inadequately treated patellar fracture can result in the loss of function of the kneecap and consequently a severe functional disorder of the knee joint , including the inability to walk or stand.
Anatomy and function of the kneecap
The kneecap is a roughly triangular shaped bone that is integrated into the tendon-extensor apparatus of the knee joint as a so-called sesamoid bone . In this way, the kneecap transfers a large part of the stretching force of the thigh muscles to the tendon attachment on the head of the tibia . The extensor apparatus is the active extensor of the knee joint. The kneecap is the only part of this extensor apparatus that has articulated contact with the knee joint, which means that it acts as a gliding deflection point ( hypomochlion ) with increasing flexion. The counter surface of the thigh roller is called the patellar slide bearing. On both sides in the longitudinal direction next to the kneecap, the holding apparatus of the patella (retinaculum) runs, which transfers part of the stretching force and centers the kneecap in the plain bearing.
This special arrangement and function of the kneecap leads to high tensile stress on the bone as well as increasing bending stress when flexing. The kneecap withstands this force without breaking even under the highest loads, so that the tendon attachments of the quadriceps tendon or the patellar tendon tend to tear off spontaneously under overload. Isolated tears of the bone do not occur.
Injury patterns and consequences
In the event of a fall on the knee (e.g. on a step) or impact of the bent knee on an obstacle (e.g. with a motorcyclist), there is a direct break line of the kneecap and, in addition, increased tensile stress in the thigh muscles due to the defensive movement . None of the individual factors alone can lead to a kneecap fracture. The combined action of force (direct front wall impression and tensile stress), however, leads to a complete rupture of the kneecap. If the muscles act vigorously, the reserve extensor apparatus of the kneecap ( retinaculum patellae ) is torn transversely: The ends of the fracture then acutely move apart, the leg can no longer be extended, and standing becomes impossible.
The fracture of the kneecap in a historical context
The fundamental importance of the kneecap for walking upright makes the attention that has always been paid to its fractures understandable. Due to the near-surface subcutaneous position of the kneecap, the easily comprehensible functional processes, the considerable loss of function in the case of a kneecap fracture and the high demands that the kneecap fracture places on the treating doctor, the patellar fracture was the focus of interest from doctors and patients from an early stage. With a patellar fracture, the patient not only loses the ability to actively straighten the leg, it is also impossible for him to stabilize the knee joint so that he can no longer stand on the injured leg. The clinical picture of the kneecap fracture with the fracture gap palpable through the skin as a dent , dislocation and crepitation (fracture rubbing) was already described by Soranos of Ephesus in the first century in Rome. The casualties are highly disabled in accordance with the loss of function.
A particular problem in the treatment of patellar fractures arises from the dislocating muscle pull of the quadriceps muscle, which makes it much more difficult to attach the fragments to one another. At the same time, it must be taken into account that fractures of this largest sesamoid bone in the body are a joint injury. A treatment that immobilizes the fracture for the purpose of healing the fracture always involves the risk of stiffening of the knee joint. The results after conservative treatment were therefore often unsatisfactory. Ambroise Paré had not seen a patient treated who had not limped all his life. At the beginning of the 20th century, a fracture of the kneecap often led to disability and retirement and in a number of cases, both after conservative and surgical treatment, to the death of the patient.
Surgical fracture treatment in general has received significant impulses from the care of the patellar fracture. On the one hand, the functional restriction and the connection with the non-healed fracture was always understandable. On the other hand, the kneecap, which can be felt through the skin, was very early on for surgeons to attempt sutures. Marc Aurel Severin from Naples describes the first successful suture in 1646. He exposed the poorly healed patella of a clergyman, freshened the fracture surfaces, then brought them into as close contact as possible and tied them together. It is not known which suture material he used, but the success: in the spring the clergyman was able to walk again. Silver wires were used for later suturing attempts, for example in the first application of antisepsis by Sir Joseph Lister on a rider's patellar fracture in London in 1877, which was decisive for the development of surgery .
Diagnosis
First of all, it is based on symptoms and clinical signs: The typical clinical appearance of a complete kneecap fracture is the inability to stretch the knee joint, a gap between the pieces of bone (fragments) that can be felt through the skin and local pain and swelling. During the examination, the patient is allowed to lift his leg straight, which fails: the lower leg cannot be lifted with it. These signs allow a reliable diagnosis without X-ray diagnostics, which is why the fracture of the kneecap has been a clearly defined clinical picture for centuries.
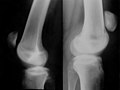
roentgen
With simple x-ray images of the knee joint in two planes (from the front and from the side), any fracture of the kneecap can be reliably diagnosed. The fragments appear pulled apart and usually with a simple transverse or diagonal break, which corresponds to the typical force applied from the front. This also means that the cartilaginous joint surface of the kneecap to the thigh roll ("patellar slide bearing") is destroyed.
With higher forces such as B. in traffic accidents or poor bone structure ( osteoporosis ), so-called multiple fragment fractures or star fractures occur, which mean a much greater destruction of bones and articular surface, but in principle primarily have the same effect on knee function.
The representation of the multiple-fragment fracture in the X-ray image is less reliable, but further diagnostic imaging with CT or magnetic resonance imaging is rarely useful for a surgeon: During the surgery, which is absolutely necessary, all individual fragments can be openly identified and treated accordingly.
The patellar fracture can also be easily visualized with sonography . The kneecap lies just below the skin and is clearly identified by the total sound reflection on its front surface. You can see the fragments that have diverged and the massive effusion. During bone healing, ultrasonography can be used to detect increasing callus .
Classification of patellar fractures
after Speck and Regazzoni (1994)
| Type A longitudinal fractures | Type B transverse fractures | Type C multiple fragment fractures |
|---|---|---|
| A1 not displaced longitudinal fracture | B1 Pole demolition without joint involvement | C1 multi-fragment fracture without dislocation |
| A2 displaced longitudinal fracture | B2 simple transverse fracture | C2 multi-fragment fracture (dislocation <2 mm) |
| A3 longitudinal fracture with additional fragment | B3 transverse fracture with additional fragment or double transverse fracture | C3 multi-fragment fracture with bursting (dislocation> 2 mm) |
Differential diagnoses
Rarely does the radiological delimitation of the patellar fracture from a patella partita (Latin: two-part kneecap), i.e. a lack of fusion of the bone nuclei during development, cause diagnostic difficulties. While fractures are sharp-edged, the patella partita has rounded edges; the “fragments” are not congruent with one another. The patella partita usually lacks the typical clinical findings of a patellar fracture, and there is no loss of function.
Another possible differential diagnosis can be differentiated during the physical examination : If the knee extension function fails completely and the patella is palpable and radiologically detectable, there may also be a complete tear of the patellar tendon between the kneecap and the attachment point on the tibial head (tuberosity). The even rarer complete tear of the quadriceps tendon leads to the inability to stretch, like the patellar fracture and the patellar tendon rupture. The kneecap is not high here, however, as it remains attached to the shinbone with the kneecap tendon. Both types of tendon ruptures must also be surgically sutured back to the kneecap. For this purpose, the suture is fixed through holes drilled in the kneecap (transosseous suture) or the suture material is fixed to the bone with a suture anchor. The use of fluoroquinolones ( ciprofloxacin ) is a possible cause of the spontaneous quadriceps tendon rupture (and rumbling of other large tendons), especially in older patients.
Differential diagnosis of the bipartite patella : In contrast to the longitudinal fracture (see below), the fragments have rounded edges
Differential diagnosis of rupture of the patellar tendon : Signs on the X-ray: elevated patella.
therapy
The principle of treatment is to restore the entire knee extensor apparatus. In addition, as with any joint fracture, the joint surface of the kneecap must be restored with millimeter precision. In addition, the reserve extensor must be sutured to the side of the kneecap. An exercise-stable supply must be carried out in order to allow an early functional follow-up treatment. Only all of these individual measures lead to the result of bone healing of the fracture with full functionality of the knee joint.
Conservative (non-surgical) therapy
The classic patellar fracture is a dislocated transverse fracture with wide divergence of the fragments. Conservative therapy (without surgery) is only possible for a patellar fracture if the fracture is definitely not displaced (undislocated). Such fractures can only exist if the reserve extensor apparatus ( retinaculum patellae ) is preserved. In addition, fractures of the kneecap can occur as a result of particular impact on the front surface in the form of longitudinal fractures. In principle, these longitudinal fractures differ very little, as no muscle pulls across the kneecap. Such fractures are suitable in large numbers for conservative therapy. In the case of longitudinal fractures without any dislocation (in this case the very strong periosteum is usually completely intact), immobilization can even be dispensed with from the outset and an early functional treatment can be performed with pain-adapted full load .
The treatment consists of a temporary immobilization in a plaster or plastic sleeve over the knee joint, which prevents the fragments from moving apart. For a limited time, the injured leg should not be fully loaded. The healing of the kneecap is checked with the help of X-rays. Thrombosis prophylaxis with heparin injections must be provided while the injured leg is being subjected to reduced stress .
Operative therapy (principle)
Any dislocated fracture with divergence of the fragments must be treated surgically open. The fibers of the stretching apparatus can be removed from the fracture area under sight, and the fragments can be adapted and put together. The joint surface, which cannot be seen from the front during the operation, is restored smoothly by pressing the surgeon's finger. The position of the individual fragments is checked with a mobile X-ray device during the operation . In order to fix the assembled patella, an osteosynthesis (bone union) must be carried out, which allows a functional follow-up treatment ( exercise treatment ). This osteosynthesis on the kneecap must above all be stable against the muscle strength of the quadriceps and at the same time securely hold the reconstruction of the joint surface.
Open patellar fractures, i.e. fractures with damage to the skin surface, must be surgically treated as an emergency procedure within 6 hours before the bacteria that may have penetrated can settle and cause an infection . Due to the involvement of the kneecap, the infection can also spread to the entire knee joint. The osteosynthesis implants are no different from the typical closed (covered) patellar fracture. As an infection prophylaxis, these patients must receive antibiotics during and after the operation . In addition, the tetanus vaccination protection must be clarified.
surgery
Operations on the knee are performed under general or spinal anesthesia . It can be a to reduce blood loss and better operational visibility tourniquet is applied. The tourniquet must be dispensed with in smokers and patients with circulatory disorders as well as tissue tears in the skin in order to avoid possible wound edge necrosis .
Tension band osteosynthesis
The basic principle of osteosynthesis on the kneecap is best achieved with the tension strap . This process developed from the wire seam process under the engineering aspect of prestressed concrete : Here steel bars are used for tensile stability, while the concrete ensures pressure stability. The established bone of the kneecap is pressure-stable, while a wire loop, which is placed on the front surface of the knee at the base (quadriceps tendon) and the tip (patellar tendon), creates tensile stability. The wire loop is advantageously guided as an O-loop, which prevents strangulation of the tendon attachments. Other surgeons guide the loop in the shape of an 8, which, however, leads to a narrowing of the tendon attachments when the tension of the wire increases. The advantage of the tension belt is that the stability in the movement of the knee joint and thus changing tension is maintained. The compressive stress on the joint side of the kneecap increases with increasing flexion of the joint and the anterior tensile stress on the wire increases. When the knee joint is fully extended, however, the pressure on the articular surface of the kneecap is low: the fragments may even gape. That is why the pure tension band is supplemented by two axial drill wires with the aim of axial stability of the osteosynthesis even in extension (see below). This arrangement of the osteosynthesis material ensures fracture healing in terms of flexion, extension and function.
The method is particularly attractive due to the low and cost-effective cost of materials and the reliability of the results. Steel wire made of stainless steel is used, which is fed with a bushing along the bone edges of the kneecap (see illustration on the right). The ends of the wire loop are then twisted with pliers and shortened with a wire cutter. Another advantage of the procedure is that the patient is allowed to move his leg during the entire follow-up treatment, the functional stress is even a prerequisite for a good result.
Since the necessity of metal removal after osteosynthesis with wire burdens the patient and generates costs, attempts have been made to use absorbable suture loops for tensioning straps. Since these materials are not inert like wire, but rather open-pored cords and therefore can absorb liquid from the wound edges, they pose a risk of infection. In addition, when they biodegrade, large concentrations of organic acids ( polylactic acid , polymalic acid) are released which affect the surrounding tissue Damage due to the changed acidic pH value . The risks outlined above neutralize the advantages of unnecessary material removal, so that such procedures are no longer carried out today.
Tension band osteosynthesis with additional axial drill wires
The goal of the tension band is only achieved if the bone substance of the kneecap and the type of fracture ensure compression stability and rotational stability. If there are any doubts about the stability, this can be achieved by additionally inserting strong axial drilling wires ( Kirschner wires |). After the fracture has been reduced, the drill wires are drilled into the kneecap from the upper edge, cross the fracture line and leave the kneecap again at the insertion of the patellar tendon. The wires should be drilled parallel about 2 cm apart. In this case, the wire loop of the tension belt is not only placed around the tendon irradiation into the kneecap, but also over the drill wire ends, which improves the attachment. A decisive side effect of this variation of the operation is that a guaranteed position of the articular surface is achieved even when the tension of the cerclage is reduced when the knee is in extension. This effect is so important that the operation of the patellar strap is now very often performed in this variation.
Tension band osteosynthesis for multiple fragment fractures
With increased force (e.g. car accident) and increased bone fragility ( osteoporosis ), multiple-fragment fractures can occur. The basic principle of the treatment of such fractures (all multi-fragment breaks) consists in the construction of two main fragments from the several fragments. The best and easiest way to do this is by open adaptation of the individual fragments under view, with the decisive reduction in the joint level (articular cartilage). No errors can be accepted here. The fragments are connected by short drill wires or screws that run parallel to the articular surface of the kneecap. The direction of the drill wires must be perpendicular to the respective fracture line. If all the small fragments are combined into a large main fragment above (quadriceps tendon attachment) and below (patellar tendon attachment), these two main fragments can be combined in the sense of a classic tension band with two axial drill wires and a cerclage. Sometimes, however, an enclosing cerclage running around the equator of the kneecap is also necessary to hold the fragments together in the form of a kneecap. In principle, this fracture treatment should also be exercise-stable like all tension straps. But if the kneecap consists of many individual fragments that z. In some cases, if you have suffered partial loss of substance, especially of the cancellous bone, this goal cannot be achieved and a temporary immobilization of the extremity with a cast is indicated. In some cases, if the substance is lost, an autologous bone transplant or bone substitute material must be used.
Lateral cable osteosynthesis (Labitzke)
For this modification of a wire loop osteosynthesis, the so-called "rope osteosynthesis system Labitzke" is used. As with a tension band with additional axial drill wires, a primary fragment fixation is achieved by means of drilled longitudinal wires. Around the bent ends of the wires at the base of the quadriceps tendon and the patellar tendon, a wire loop on the patella is not passed in front of the kneecap, but on the side and tightened. The wire loop is not a monofilament (single-thread) wire, but a thin polyfilament (multi-thread) wire rope . Such a rope cannot be twisted or knotted, but is closed with a tail piece. The advantage of the lateral procedure is said to be the continuous application of pressure to the ends of the fracture. Other authors see the thin wire ropes as problematic "sawing" implants that cause damage to the substance of the patella during functional post-treatment. The procedure is currently seen more as a reserve procedure.
Screw fixation
Smooth transverse fractures in young patients with good bone substance and the rare longitudinal fractures can be stabilized with lag screws after anatomical reduction . Two of these are usually inserted parallel to the drill wires from the reinforced tension band. In the case of longitudinal fractures, transverse to the knee axis. There is no relevant advantage of screw osteosynthesis over tension belts. However, biomechanical measurements under laboratory conditions allow higher tensile stresses in screw processes compared to wire cerclages. Screws are a static osteosynthesis which, in contrast to dynamic tension belts, cannot use the muscle and tendon forces to generate pressure on the ends of the fracture.
Plate fixation
For transverse fractures, but also particularly star fractures and debris fractures, plates of different shapes are suitable for osteosynthesis. The plates are applied to the patella from the front (star plate) or from the edges (bilateral plate). The anchoring screws are to be inserted at a stable angle . The advantage is an implantation that is gentle on the soft tissue and without manipulation of the tendon attachments, as is necessary with cerclages and tension belts. In particular, the stability of the plate process is higher than that of the wire process. Comparative studies have to show whether plate fixation will bring better results than tension banding for all types of fractures. In addition to the stability of the supply, the biology of fracture healing plays a decisive role.
Partial patellectomy
Preserved stable bone structure of the fragments is a basic requirement of any osteosynthesis. If part of the kneecap is significantly destroyed as part of the fracture, so that both the bone substance and the joint surface have suffered substantial damage, instead of reconstruction, it may be necessary to partially remove the kneecap in precisely the destroyed area. After the destroyed substance has been removed, the preserved tendon attachments of different sizes (patella and quadriceps tendons) can be made into two fragments, each with straight fracture edges. These can then be combined with tension straps or screws to form a functional residual patella.
With frequent destruction of the lower patellar pole, the patellar tendon is fixed to the remaining patella. Tendon sutures with bone anchors are used for this. For temporary protection of the tendon suture, a wire loop is pulled through the attachment point of the patellar tendon at the head of the tibia (McLaughling cerclage).
Total patellectomy
Primarily when first treating a fracture, complete removal of the kneecap is only indicated in the case of massive, possibly open destruction of the kneecap. Clinical studies have shown that the clinical results of such primary kneecap removal are poor. In principle, the reconstruction of the fragments should be attempted and achieved. Patellectomies can only be useful and effective if the healing results with osteoarthritis of the joint surfaces of the patella and femoral plain bearings are very poor.
Aftercare
The principle of the tension band requires functional post-treatment of the patellar fractures. After short-term postoperative immobilization on the positioning rail, the patient can be mobilized with the aid of forearm crutches. Rolling off the operated extremity makes sense. A knee that has been operated on with tension belts can only be loaded about 6 weeks after the operation at the earliest, because the tension on the fracture treatment under load would overwhelm the stability of the osteosynthesis. Due to the relief of the leg, thrombosis prophylaxis with subcutaneous heparin syringes must be carried out in the follow -up treatment . This measure can only be ended when the extremity is almost completely stressed.
Results
The quality of the restoration of the joint surface and the stable bone fracture healing are decisive for the result. If the formation of steps remains, osteoarthritis (premature joint wear) will develop , which can cause pain and restricted mobility. Smooth transverse fractures of the kneecap can lead to good to excellent results after fitting with classic tension belts. In more than ¼ of the patients, however, there are movement restrictions and pain, for which an indication cannot always be found in the X-ray image. These problematic cases with classic tension belts give rise to the use of other osteosynthesis methods. But even with screw osteosynthesis and a very rarely performed nailing procedure, a percentage of poor results remain.
There is a risk of impaired wound healing in patients with circulatory disorders , smokers and diabetics . The skin in the injured area is severely damaged by the direct knee impact and the resulting fracture. The operation and preparation of the tissue can be expected to cause additional damage to the blood flow. Since the kneecap and the osteosynthesis material are very close under the skin, there is a risk of an infection spreading deeply and thus also to the fracture and osteosynthesis material in the case of wound edge necrosis .
For the outcome of an operation, it is of central importance to make the decision to partially or completely resect the patella (patellectomy) at an early stage, if possible at the first operation, and then to carry out the resection immediately. A late implementation, e.g. B. after no healing or in the case of symptoms due to cartilage damage no longer leads to an improvement in the clinical result.
prophylaxis
Especially with fashion sports such as inline skating and skateboarding , but also with ice skating and cycling , there is a risk of a patellar fracture due to direct knee impact with increased muscle tension in the knee extensors. It is recommended to wear knee protectors because this prevents the direct traumatic impact on the bone structure of the kneecap. In vehicle construction, by modifying the edge of the dashboard and making it mandatory to wear seat belts, it was possible to achieve a significant reduction in the so-called dashboard injuries that were previously very common .
Patellar fracture in animals
Patellar fractures are a rare bone fracture in animals. They are most often seen in domestic dogs . They almost always have to be treated surgically. In veterinary medicine, tension belts ( cerclage ) are mainly used , possibly together with Kirschner drill wires, and tension screws are also used for longitudinal fractures. If the tip of the kneecap is torn off ( apex patellae ), partial removal may also be indicated , and for complex fragment fractures a total removal may be indicated. The osteosynthesis procedures show a fairly high rate of complications, especially in the form of a break or loosening of the wire loops. The total removal of the kneecap hardly leads to a functional impairment of the affected leg in dogs. All forms of therapy may (chronic changes of the knee joint osteoarthritis , Gonotrochlose of, calcifications patellar ligament not stop) altogether.
Literature and Sources
- I. Klute, N. Meenen: The fracture of the kneecap - Modern tension band osteosynthesis in a historical context. (Booklets for the magazine Der Unfallchirurg 269). Springer-Verlag, Heidelberg 1998, ISBN 3-540-63590-4 .
- DW Aitken: Subcutaneous Suture of Fractured Patella. In: British Medical Journal , Volume 2, Number 1647, July 1892, pp. 177, ISSN 0007-1447 . PMID 20753814 . PMC 2420779 (free full text).
- E. Albert: Textbook of surgery and operating theory. Urban & Schwarzenberg, Vienna / Leipzig 1891, pp. 404-410.
- WL Axford: A method of wiring fractures of the patella. In: Annals of Surgery . 8, 1888, pp. 1-5.
- W. Axhausen, G. Schultze: For the treatment of comminuted fractures of the patella. In: Zentralbl Chir. , (14) 84, 1959, pp. 534-537.
- R. Babayan, K.-H. Jungbluth, J. Thunich: Patellar fractures. Treatment methods and results. In: Nude Traumatology. 5, 1975, pp. 27-30.
- F. Baumgartl: The knee joint: diseases, injuries and their treatment. Springer, Berlin / Göttingen / Heidelberg 1964, pp. 296-318.
- L. Böhler: The technique of bone fracture treatment. 12. u. 13th edition. Vol. 2/2, Wilhelm Maudrich Verlag, Vienna 1957, pp. 1586–1617.
- V. Bühren, O. Trentz, Henneberger: The operative treatment of the patellar fracture . In: surgeon. 60, 1989, pp. 723-731.
- MJ Curtis: Internal fixation for fractures of the patella. In: J Bone Joint Surg. (Br), 72-B, 1990, pp. 280-282.
- R. Labitzke: Surgical technique and treatment results after lateral tension belts on the patella and olecranon. In: Accident Medicine. 83, 1980, pp. 450-456.
- F. Magerl: The patello-femoral joint. Causes, forms and accompanying injuries of the patellar fracture. In: Hefte Unfallheilkd. 120, 1975, pp. 45-59.
- M. Müller, M. Allgöwer, R. Schneider, Hans Willenegger: Manual of osteosynthesis - AO technology. 3. Edition. Springer, Berlin / Heidelberg / New York 1988, pp. 1-3, 44-45, 226-228, 565-568.
- F. Pauwels: Surprising success through the use of a tension belt in the patellar fracture. 83rd conference In: Langenbecks Arch Klin Chir. 316, 1966, pp. 221-224.
- A. Rüter, C. Burri: Patellar fractures. Discussion and recommendations. In: magazines accident medicine. 120, 1975, pp. 91-98.
Web links
Individual evidence
- ^ A. Paré: Wundt-Artzney. German by Peter Uffenbach. Fischer, Frankfurt, Lib. XIV, cap. 22, 1601.
- ^ Marco Aurelio Severino: De Efficaci Medicina . 1646.
- ^ M. Speck, P. Regazzoni: Classification of patellar fractures. In: Z Unfallchir Versicherungsmed. , 1994, 87, pp. 27-30.
- ^ AP Fortis, Z. Milis, V. Kostopoulos, S. Tsantzalis, P. Kormas, N. Tzinieris, Th. Boudouris: Experimental investigation of the tension band in fractures of the patella. In: Injury. 2002, 33 (6), pp. 489-493.
- ^ R. Labitzke: Tension straps - right and wrong using the example of the patellar fracture. In: The surgeon. Volume 68, number 6, pp. 638-642, doi: 10.1007 / s001040050245 .
- ↑ J. Gehr, W. Friedl: Problems of the tension belt osteosynthesis of patellar fractures and their consequences for further implant developments. The XS nail. In: Chirurg , 2001, 72, pp. 1309-1318.
- ^ Leo Brunnberg et al. a .: On injuries to the patella and the patella ligament in dogs and cats. 1. Patellar fracture. In: Small Animal Practice. 36: 547-559 (1991).