Cruciate ligament tear
| Classification according to ICD-10 | |
|---|---|
| S83.50 | Not designated in more detail cruciate ligament Incl .: cruciate ligament NOS |
| S83.53 | Rupture of the anterior cruciate ligament Including: partial or complete tear |
| S83.54 | Rupture of the posterior cruciate ligament Including: partial or complete tear |
| ICD-10 online (WHO version 2019) | |
A cruciate ligament tear , also called cruciate ligament rupture , is an incomplete (partial) or complete (complete) tear (rupture) of one or both cruciate ligaments . In most cases, the anterior cruciate ligament (ligamentum cruciatum anterius) is affected. The cause of a cruciate ligament tear is that the tear strength of the ligament is exceeded .
Cruciate ligament tears usually occur without any external influence through sudden changes of direction when running or jumping. They are the most common clinically relevant injuries in the knee joint area . Cruciate ligament tears can be diagnosed with relative certainty on the basis of their symptoms , the description of the injury process and with the help of simple palpatory examinations . Magnetic resonance tomography and arthroscopy can further confirm the diagnosis. Untreated cruciate ligament ruptures can lead to severe degenerative damage to the knee. The therapy can be conservative as well as surgically ( minimally invasive by means of arthroscopy). Which therapy is carried out when and in which variant is the subject of controversial discussions. What is undisputed, however, is that currently no form of therapy can qualitatively restore the original condition of an uninjured cruciate ligament. A long-term consequence of a cruciate ligament tear is the significantly increased likelihood of developing knee osteoarthritis - regardless of the type of treatment. A large number of studies have come to the conclusion that special preventive exercises can significantly reduce the risk of a cruciate ligament tear.
In the Anglo-American specialist literature, the term anterior cruciate ligament injury is used for injuries to the anterior cruciate ligament . Cruciate ligament rupture is correctly translated as cruciate ligament rupture . Injuries to the posterior cruciate ligament (ligamentum cruciatum posterius) are referred to as posterior cruciate ligament injury .
Types of cruciate ligament ruptures
Cruciate ligament tears are rarely isolated injuries. The ruptures are usually accompanied by other lesions of other ligaments and the menisci . There are two types of cruciate ligament tears:
- Anterior or posterior cruciate ligament tear with sagittal instability, that is, from anterior to posterior, and positive drawer phenomenon
- Combination injury with drawer phenomenon when the foot is turned inwards or outwards:
- Anteromedial rotational instability ( AMRI , anterior- centered rotational instability ): anterior cruciate ligament tear, tear of the medial meniscus and the mediodorsal capsule, often an additional tear of the inner ligament ( usually pointing towards the middle) (so-called unhappy triad ).
- Anterolateral rotational instability ( ALRI , anterior-lateral rotational instability ): tear of the posterior cruciate ligament, the outer ligament and the dorsolateral capsule.
- Posterolateral rotational instability ( PLRI , posterior-lateral rotational instability ): tear of the outer ligament and the posterior cruciate ligament with posterior-central or posterior-lateral rotational instability.
Injury Mechanisms
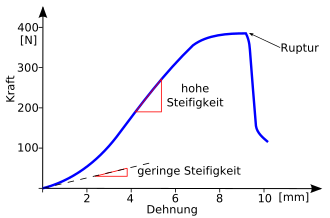
With low load (= force ). the curve is flat because the ligament is stretched without increasing the intraligamentary force (low stiffness). The stiffness of the belt increases with increased load. There is initially a largely linear rise (high rigidity). In this area, the collagen fiber bundles of the tape behave elastically because they are aligned parallel. If a further force is applied, irreversible changes take place in the band, so that it can no longer relax to its original length. If the force increases even further, individual fiber bundles tear (the curve becomes flatter). Since not all fiber bundles are exposed to the same high load, the load can increase even after the first cracks (the stiffness decreases again). Above a certain maximum force, the tape breaks suddenly, which can be seen in a sudden drop in the curve.
Anterior cruciate ligament
The anterior cruciate ligament injury typically results from a change in direction. Often there is an outward rotational position of the lower leg with valgus flexion stress or an inward rotational position with varus flexion stress . Excessive stretching or bending movements ( hyperextension or hyperflexion) can also be a trigger. The majority of the cases are sports injuries. Such injuries ( trauma ) occur particularly frequently in so-called “stop-and-go” sports (e.g. tennis or squash ) and in team sports (e.g. soccer , football , handball , hockey or basketball ) - often also less External influence - on. Even when skiing - especially when the valley ski turns outwards, but the body remains fixed above the mountain ski - ruptures of the anterior cruciate ligament are a common type of injury. The injury mechanism that involves the valgus and internal rotation position when skiing is also known as the “phantom foot mechanism”. A tear can also be caused by a dislocation of the kneecap ( patellar luxation ) with a sudden loss of stability of the knee joint.
The failure ( insufficiency ) of the anterior cruciate ligament disrupts the function of one of the two central passive guide elements (primary stabilizers) of the knee joint. This results in a pathological freedom of movement of the tibial head forwards ( ventrally ), the so-called " tibia advance". The joint capsule, collateral ligaments, posterior cruciate ligament and menisci are increasingly used to slow down the tibia advancement. The ligament structures are overstretched. Cartilage damage occurs as the tibial advance increases. These are due, among other things, to the fact that the cartilage is exposed to significantly higher loads. In such a case, higher stress means premature wear with the development of osteoarthritis . Injuries to the menisci and cartilage accompanying the anterior cruciate ligament tear increase the risk of osteoarthritis.
Posterior cruciate ligament
Tears of the posterior cruciate ligament are less common. They arise because the posterior cruciate ligament has exceeded the maximum possible stretch; usually by external force. In most cases, not only the posterior cruciate ligament is affected by a posterior cruciate ligament tear. The injuries are therefore usually much more complex and usually affect the entire knee joint. The main cause of a rupture of the posterior cruciate ligament are traffic accidents or, more generally, so-called rapid trauma . This is due to the fact that the knee is bent when sitting in the car. The rear cruciate ligament tears when the lower leg hits the dashboard . This mechanism is therefore also called dashboard injury (literally translated from the English: dashboard injury ). However, this type of injury is relatively rare and its incidence has decreased more and more over the years. In a study carried out in Germany with over 20,000 accident victims in car accidents, only 5 cases of dashboard injury were found.
In sports that involve physical contact, such as American football , force acting from the front and center can lead to an injury of the posterior cruciate ligament due to excessive extension. Often the anterior cruciate ligament and the posterior joint capsule are injured as well.
frequency
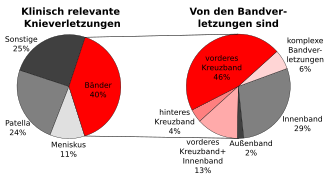
The proportion of injuries to the knee ligaments in all clinically relevant knee injuries is around 40%. Of these 40%, about two thirds of the injuries are caused by cruciate ligament tears - 46% only the anterior cruciate ligament and 4% only the rear. Mixed injuries or more complex injuries involving the cruciate ligaments account for 19%. Statistically speaking, the anterior cruciate ligament ruptures about ten times as often as the posterior one. The main cause of the significantly lower incidence of ruptures of the posterior cruciate ligament is on the one hand its larger diameter and the resulting comparatively higher load capacity and on the other hand its different function. In the United States the ratio of ruptures of the anterior cruciate ligament to the posterior one is about 9 to 10: 1, in Germany it is about 14: 1.
Around one million cruciate ligament tears occur worldwide each year. Recreational athletes are mostly affected. The tear of the anterior cruciate ligament is not only the most common knee ligament injury, but also the most common clinically relevant knee injury. The incidence is around 0.5 to 1 anterior cruciate ligament rupture per thousand population ( USA , Central Europe ) and year. In the United States, there are approximately 80,000 to 100,000 ruptures of the anterior cruciate ligament each year. The incidence is highest between the ages of 15 and 25 years. The annual cost is around $ 1 billion.
In Germany in 2002 the medical costs in hospitals for the treatment of "internal damage to the knee joint" - the main part of which is caused by cruciate ligament tears - amounted to 359.3 million euros. Statistically speaking, a cruciate ligament ruptures every 6.5 minutes in Germany. In about every third person, a meniscus is also damaged. In Switzerland, the estimates for the annual costs of cruciate ligament ruptures are between 200 and 250 million francs. Of this total, 40% are medical costs, 47% daily allowances , 2% capital benefits, such as integrity compensation ( social security compensation for pain and suffering ) and 12% disability pensions (capital values). For each cruciate ligament tear, this is almost 21,000 francs, with an average medical cost share of 8350 francs.
The Swiss accident statistics (UVG), which cover around half of all Swiss citizens, report 6350 injuries of the anterior cruciate ligament per year (period 1997 to 2001). The extrapolation for Switzerland assumes 10,000 to 12,000 cases. Of the 6350 injuries recorded, 73% are caused by “sport and play”, 10% are occupational accidents and 17% are attributable to other activities such as commuting accidents, staying in houses or other leisure activities.
Women and girls have a two to eight times higher injury rate than men who do the same sport. Various studies show that these injuries are mainly caused without contact. Here, a functional valgus position of the knee joint when landing after a jump plays a key role. According to a study, female basketball players are four times more likely to have a knee injury, knee surgery or anterior cruciate ligament surgery than male basketball players. For female soccer players, this factor is 3.41. The cause of the increased incidence in women is still largely unclear. Anatomical differences, such as greater play in the knee joint, hormones and training techniques are discussed.
The proportion of individual sports in the frequency of cruciate ligament ruptures depends very much on local preferences for the respective sport. In the USA, for example, basketball players (20%), followed by soccer (17%) and American football players (14%), have the highest proportion of cruciate ligament ruptures, while in Norway the order of soccer players (42%), handball players (26th %) and alpine skiers (10%). In Germany, the most common cruciate ligament tears occur in soccer, handball and skiing (alpine). This is followed by road traffic and work accidents . More than 70% of the tears in the anterior cruciate ligament occur without any external influence when landing after a jump, when braking or when suddenly changing direction.
The number of cruciate ligament ruptures diagnosed annually has been increasing for years. In addition to the improved diagnostic possibilities - with which cruciate ligament ruptures are more often recognized as such - the increase in sporting activities in the leisure society is also to blame for this tendency. Without some specific sports, cruciate ligament ruptures would be a relatively rare trauma.
Risk factors
In addition to the factors sport and gender already described under the heading Frequency, other risk factors also play a role in cruciate ligament rupture. Due to the frequency of the injury, extensive statistical data and a large number of studies derived from it are available. The etiology of an anterior cruciate ligament tear without external influence is very complex, and a number of factors, some of which are very different, influence the risk of a rupture. To date, it cannot be fully explained why individuals are at higher risk for this injury than others. For example, it is unclear why, if the anterior cruciate ligament of one knee is injured, there is an increased likelihood of the same injury to the other knee within the next few years. German soccer players who have already had a cruciate ligament rupture are more than five times more likely to have a new cruciate ligament rupture than players who have previously been spared this type of injury. In terms of risk factors, a distinction is made between intrinsic (personal) and extrinsic (external) factors. The intrinsic factors include, for example, genetic predisposition or anatomy, fitness level , neuromuscular effects or hormonal factors. On the other hand, the nature of the ground, the weather or the sports shoes are extrinsic risk factors.
Knowledge of the risk factors for cruciate ligament ruptures is an important starting point for preventive measures .
Intrinsic Risk Factors
Anatomical factors are among the risk factors that have long been suspected. The tear resistance of a cruciate ligament is directly related to its width, which in turn can vary from person to person. In an anthropometric study, the anterior cruciate ligaments of the uninjured contralateral knee of patients with a cruciate ligament rupture were compared with those of a control group with the same mean body mass. The volumes of the cruciate ligaments were determined by means of magnetic resonance imaging. In the group with cruciate ligament tears, the volume of the contralateral cruciate ligament averaged 1921 mm³, while it was 2151 mm³ in the control group. The authors of the study conclude from this that anthropometric differences in the volume - and, derived from this, the width - of the cruciate ligament have a direct influence on the probability of a cruciate ligament tear without external influence. A correlation between a narrow cruciate ligament cavity (intercondylar notch), which is in turn related to a narrow cruciate ligament, with an increased risk of a cruciate ligament rupture was found in previous studies . However, there is no scientific consensus on this as other studies come to different results. Women have a narrower cruciate ligament cavity than men, which is why this anatomical difference is an explanatory model for the higher incidence of cruciate ligament ruptures in women.
Deficits in proprioception , i.e. the perception of one's own body movement and position in space, as well as neuromuscular fatigue symptoms in the lower extremities and central fatigue symptoms when landing after a jump, are seen as risk factors for an anterior cruciate ligament rupture. One study found that patients with a cruciate ligament tear had significant deficits in neurocognitive abilities. Other risk factors include dynamic valgus stress on the knee joints, a lack of hip and trunk control, and poor knee flexion when landing after a jump. It also increases a so-called quadriceps dominance, i.e. H. a predominance of the strength of the quadriceps muscle over the hamstring muscles, the risk of an anterior cruciate ligament injury.
Extrinsic Risk Factors
The coefficient of friction between the sole of the sports shoe and the ground is a factor in causing a cruciate ligament tear. A high coefficient of friction correlates with an increased risk of injury. In a study over two seasons in the top three Norwegian handball leagues, the friction coefficient between the sports shoe and the flooring played a role in 55% of cruciate ligament tears. In American football, fewer players are injured by cruciate ligament ruptures in colder months than in warmer months. One of the reasons discussed here is the reduced grip in the cooler months.
A study of cruciate ligament ruptures in Australian football also described an association with weather conditions and the injury rate. The injury rate on dry playing fields was significantly higher than on wet ones. The cause is suspected to be a softer surface after rainfall, which reduces the power transmission between the shoe and the surface.
A relationship with soil quality was also found in Australia. In the Australian Football League, for example, fewer cruciate ligaments tore on ryegrass than on dog-tooth grass . The cause here is assumed to be a reduced adhesion of the sports shoes in interaction with the ryegrass, as a result of which the force transmission that is destructive for the cruciate ligament is lower than on the dog-tooth grass with higher adhesion.
Symptoms
If a cruciate ligament is torn, this usually leads to significant swelling of the knee joint and, as a result, to pain due to the capsular expansion of the joint. A bloody joint effusion ( hemarthrosis ) is the normal case in a cruciate ligament tear. It occurs in 95% of cases and very quickly restricts the mobility of the knee joint. Together with the instability of the knee joint, hemarthrosis is a leading symptom of a cruciate ligament rupture. Conversely, a cruciate ligament tear is responsible for about 50 to over 75% of all hemarthrosis. These symptoms were already described in 1879 by the French Paul Ferdinand Segond (1851–1912): Violent pain inside the knee and rapid bleeding with corresponding swelling of the joint. The cause of these symptoms are the nerve fibers and blood vessels that run in the cruciate ligament. The former cause the pain when torn, and the latter cause bleeding into the joint.
Often the tearing is associated with an audible bang ("plop"). The tearing is followed by a brief pain. The affected person notices the instability in the knee immediately after the first pain has subsided. The joint effusion usually only sets in during the day. As a rule, the practiced sport has to be stopped. An exception are skiers, who can often still manage the descent - but with considerable pain. If all of these symptoms are true, then there is a 90 percent certainty that the anterior cruciate ligament tears (or both). The knee can usually no longer be fully extended and is held in a slightly bent position ( relieving posture ). In this flexed position, you can pull the lower leg bone forward by about 5–10 mm against the thigh bone without feeling a stop, while with a healthy knee only a few millimeters (2–3 mm) are possible and then you feel a stop (positive Lachman test ).
After about a week, the symptoms of an anterior cruciate ligament tear will subside. Some patients start exercising again after two weeks. The degree of instability of the knee joint is strongly dependent on the secondary knee joint stabilizers and their training status. Secondary knee joint stabilizers are other peripheral ligaments and muscle tendons. They can partially take over the function of the anterior cruciate ligament to stabilize the knee joint. Many patients are largely symptom-free for three to six months. After that, the secondary stabilizers can usually no longer absorb the forces acting on the knee joint. Damage to the menisci and collateral ligaments as well as an increased incidence of giving way are the result.
Accompanying injuries
Isolated anterior cruciate ligament tears are rather the exception. Up to 80% of all cruciate ligament tears are accompanied by other injuries. Injuries to the menisci are extremely common. In an extensive study of acute cruciate ligament tears, a tear of the medial meniscus was diagnosed in 42% of the cases and a tear of the outer meniscus in 62%. Another study found a tear of the medial meniscus in 60% of patients and a tear in the outer meniscus in 49% of cruciate ligament tears in the chronic interval (when a ligament was performed). If the injured meniscus is removed, the instability of the affected knee increases. The severely limited shock absorption also leads to an increased frequency of secondary arthrosis. Undamaged menisci have a positive effect on the outcome of a cruciate ligament surgery. For this reason it is recommended - if the tear of the meniscus permits - a refixation of the same. Ideally, this should be done together with the reconstruction of the cruciate ligament.
Another common accompanying injury is a tear in the inner and / or outer ligament of the knee joint. If the inner ligament, inner meniscus and anterior cruciate ligament are affected, one speaks of an unhappy triad . The anterolateral (front and side) bony capsule tear on the tibia plateau, the so-called Segond fracture, is rather rare . According to recent findings, this represents the bony avulsion of the anterolateral ligament (ALL). This is an important stabilizer against forced internal rotation of the knee. Only a tear in this tape allows a positive pivot shift test . In a retrospective study by the Belgian working group, which first described the ligament anatomically in 2013, it was found in 206 of 351 MRI scans of knees with a subsequently operated anterior cruciate ligament tear, which is made more difficult by the fact that the ligament runs at an angle to the standard layers of magnetic resonance imaging. An ALL tear was found in 162 (79%) of the knees, a bony tear ( Segond fracture ) in three cases (2%).
Injuries to the joint cartilage (traumatic chondropathies ) are involved in 16 to 46% of all ruptures of the anterior cruciate ligament.
Rarely, and mostly undetected, is the tear in the posterior, outer capsule shell, especially the tendon of the popliteal muscle (deep calf muscle). If left untreated, this injury leads to considerable knee joint instability with a visibly impaired gait.
Diagnosis
In many cases, the diagnosis is made with a considerable delay, even if the patient consulted a doctor immediately after the injury. Some studies indicate a median period of 2 to 21 months that elapses between the time of injury and the correct diagnosis. In many cases, it is also necessary to visit several doctors before the correct diagnosis is made. Typical misdiagnoses are especially meniscus tear and " sprain ". It is therefore assumed that cruciate ligament ruptures are underdiagnosed. This means that they actually happen more often than they are correctly diagnosed.
Clinical findings
If the anterior cruciate ligament tears, the so-called anterior drawer phenomenon occurs : when the knee is bent, the lower leg can be pushed forward from the back. If, on the other hand, the posterior cruciate ligament is torn, the posterior drawer phenomenon occurs : with the knee bent, the lower leg can be pushed from the front to the back.
The initial diagnosis is carried out using a drawer and Lachman test (rarely the pivot-shift test ). Due to the anatomy of the anterior cruciate ligament (two ligament parts = fascicle bundle), a clinical diagnosis is often difficult if only one bundle is torn. Here, for example, there is a negative drawer phenomenon in 90 ° flexion of the knee joint, but a positive Lachman test in 15 ° flexion.
Failure (insufficiency) of the posterior cruciate ligament can in some cases be assessed by observing ( inspecting ) the knee joint, which is bent at 90 °, from the side with the patient lying down. If the tibia head has sunk back, an injury to the ligament should be considered. This phenomenon can be intensified by additionally tensing the so-called hamstring muscles (rear thigh muscles). The posterior drawer is opened by subsequent quadriceps muscle contraction ( contraction ).
The loss of stability occurs with increasing flexion in the knee joint and is not present when the knee is extended. This explains the surprisingly low level of discomfort with isolated cracks. Complaints are mainly reported when climbing stairs or when lifting weights behind the kneecap (retropatellar) (increased pressure of the thigh bone on the kneecap).
The instability that results from a cruciate ligament tear causes overloading of the cartilage and the inner and outer meniscus. If the instability is not compensated by the musculature or removed by an operation, a meniscus tear and / or cartilage damage with osteoarthritis often occurs.
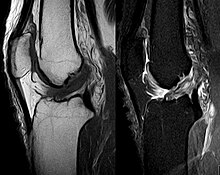
Imaging procedures

The diagnosis can be confirmed with imaging methods - namely magnetic resonance imaging (MRI, "nuclear spin"). It should be noted, however, that the interpretation of the MRI in the diagnosis of a cruciate ligament rupture provides 20 percent incorrect diagnoses . This depends on the so-called sectional images and the appropriate positioning of the knee joint during the MRI examination. The radiologist should know the exact history of the injury and also have experience examining an injured joint to avoid misjudgments. Compared to MRI, the error rate in the Lachman test, which is much easier to perform, is only 10 percent. MRI is therefore usually less sensitive and less specific for diagnosing an anterior cruciate ligament tear than clinical findings by a qualified orthopedic surgeon . The result of an MRI only rarely has an influence on clinical decision-making and should not be a substitute for a careful history and palpation. Several studies have come to the conclusion that an MRI is only useful for more complicated, unclear knee injuries - and more likely to make a diagnosis of exclusion.
X-rays do not make a direct contribution to the diagnosis of a cruciate ligament rupture. Both cruciate ligaments - whether torn or not - are not visible in the X-ray. If X-rays are taken, however, this can be used to diagnose possible concomitant bony injuries.
Diagnostic arthroscopy

Diagnostic arthroscopy ( arthroscopy ) offers the highest diagnostic reliability. This procedure is the gold standard for diagnosing a cruciate ligament tear . Although the procedure is minimally invasive , it always represents a surgical intervention in the patient's knee that involves certain risks. However, since the surgical treatment of a cruciate ligament tear is usually arthroscopic ( therapeutic Arthroscopy ), there is the possibility of carrying out the therapy, for example in the form of a partial cruciate ligament resection (in the event of a tear) or a reattachment of the torn ligament, immediately after the diagnostic arthroscopy. With the increasing spread of magnetic resonance tomographs, the number of purely diagnostic arthroscopies has decreased significantly in recent years. However, diagnostic arthroscopy is still the method of choice for the reliable clarification of the diagnosis of a cruciate ligament rupture - in the case of unclear clinical findings and an unclear MRI.
Late signs of undiagnosed anterior cruciate ligament tear
If a cruciate ligament rupture is not diagnosed and consequently not treated, the so-called giving way can result. This means that the knee joint is unstable. The patient has the impression that z. B. when walking downstairs the lower leg is not under control. Athletic loads with rotational movements of the knee joint are not possible or are avoided. Recurrent swelling tendencies due to joint effusions can occur. The consequence of such an unstable knee, which is decisive for the fate of the injured knee, is the almost inevitable meniscus lesions . These occur due to the instability-related sagittal movement (giving way) beyond the rear edge of the tibial joint surface, with overrolling of the meniscus.
Therapy options
Clinical studies show that acutely injured cruciate ligaments have a natural self-healing potential, that is, a spontaneous tendency to grow back on by itself biologically. The decisive factor for the later, adequate knee stability, however, is that this scarring occurs at the anatomically correct attachment point. If a freshly torn anterior cruciate ligament grows together with the posterior cruciate ligament, it is a phenomenon known as lambda or Wittek healing.
A cruciate ligament rupture should always be treated according to the diagnosis. An untreated rupture can lead to degeneration of the hyaline articular cartilage and thus to meniscus damage. A large number of studies have shown that failure to take therapeutic interventions leads to progressive destruction of the joint structures and that there is a high risk of re-injury.
The treatment options can be divided into two groups: surgical therapy (operation) and conservative therapy . Which form of treatment is used is usually coordinated individually with the patient according to his needs. There are different approaches and treatment concepts for both forms, some of which are controversial. In principle, the course of chronic cruciate ligament damage varies greatly from person to person. It is generally accepted that not every patient needs surgical treatment. However, studies show that younger and, above all, physically active patients benefit from surgical restoration of the kinematics and stability of the knee joint by maintaining or replacing the torn cruciate ligament. Conservative therapy is based on physiotherapeutic muscle building, which should serve to stabilize the knee joint externally. The aim of surgical therapies is the anatomical and biomechanical restoration of the torn cruciate ligament in its original function.
Neither conservative nor surgical treatment of a torn cruciate ligament can completely restore the knee to its original condition.
Conservative treatment
Not every torn cruciate ligament needs surgery. In each case, the decision is made individually, depending on the patient's age, activity, sports ability, willingness and everyday ability. Therefore, the therapy decision requires a detailed discussion with the patient. Conservative treatment is an alternative to surgery, especially for patients with an anterior cruciate ligament rupture without accompanying injuries, limited sporting activity, and older people. An increased frequency of osteoarthritis was found in active, conservative patients compared to operated patients. Several studies have shown a significant advantage of the surgical intervention, especially for athletes who practice sports such as soccer, handball or basketball - that is, sports with high rotational and hyperextension stress on the knee joint. There are some older studies that conclude that conservative treatment of a torn cruciate ligament - even in athletes - has no negative effects. A new study also shows that in young patients with uncomplicated cruciate ligament rupture, prompt surgery within 10 weeks, in contrast to wait-and-see conservative treatment with the option of later surgery in the event of instability or the patient's request, has no advantages.
In conservative therapy, early functional movement treatment tries to compensate for knee joint instability through consistent muscle building training and thus to restore the lack of stability. Another goal is to improve the proprioceptive abilities of the (periarticular) elements around the knee joint. Sufficient stability is often achieved by splinting the knee joint in an orthosis (knee brace) for six weeks and accompanying physiotherapy.
With targeted and appropriate orthopedic treatment, the majority of patients with a rupture of the anterior cruciate ligament can in principle resume their sporting and professional activity without restriction. The patients treated in this way are able to work again after an average of seven weeks and can lead a normal life after about eleven weeks. These times are usually shorter than with a surgical procedure. About 80% of the patients can be active again after four months. However, this is essentially limited to sports without direct body contact and without pivoting movements that stress the knee. Many patients with conservative treatment of the cruciate ligament tear develop a feeling of fear while exercising in the situations that led to the original injury. One of the main reasons for this is the noticeable loss of knee stability for the affected person. This uncertainty is felt by around 30% of patients 18 months after the injury and almost 80% after four years. In contrast, it only interferes with about 10% in daily life. Most patients are pain-free in everyday life. In certain situations, for example after long periods without movement or changes in humidity, around half complain of pain after four years. Joint effusion , often together with a meniscus lesion, can be diagnosed in up to 30% of patients after four years . The latter is usually a consequence of accidents resulting from the instability of the joint. Regular monitoring of the affected knee joint is necessary for the early detection of possible complications in conservative therapy. Surgical treatment is then possible at any time.
For complex knee ligament injuries (e.g. unhappy triad ), bony tears of the anterior cruciate ligament, additional lesions in the meniscus, lack of muscular compensation after intensive physiotherapy, as well as for younger performance-oriented athletes, surgical treatment is usually carried out.
Surgical treatment of the anterior cruciate ligament tear
In the 1970s to 1980s, the age limit for anterior cruciate ligament reconstruction surgery was around 35 years. This was due to the still limited surgical options using arthroscopy and minimally invasive instruments as well as the implants available at the time. Today there is no longer an age limit. The condition of the affected knee, the demands of the patient and his or her motivation are the main factors influencing the decision for or against surgical treatment. In most cases, from a medical point of view, a cruciate ligament rupture does not have an immediate need for immediate surgical intervention. A fresh rupture is operated on for cruciate ligament replacement after a physiotherapy cycle - this is usually around six to eight weeks after the injury. The knee is then usually completely swollen again. If a cruciate ligament retention method is considered, the operation must be performed within three weeks of the accident. In some cases, surgical treatment is not performed until several months after the cruciate ligament rupture. For example, when initially only a slight instability of the affected knee leads to symptoms in the patient. In the Scandinavian countries of Norway, Denmark and Sweden, the mean time between rupture and operation is seven, nine and ten months, while in the United States it is 2.4 months. The interquartile range is from 1.2 to 7.2 months in the USA and from 4.2 to 17.8 months in Norway.
Some recent studies have come to the conclusion that degenerative symptoms can be observed on the menisci of the affected knee as early as six months after a cruciate ligament rupture without surgical intervention, so that the authors recommend reconstruction within one year to reduce the risks.
The absolute indication for an operation is instability of the knee joint. Without a stabilization operation, this leads to meniscus damage and ultimately to secondary arthrosis of the joint. It is mainly people who are active in sport at a younger age who are affected, although in recent years the generation over 50 has seen an increase in cruciate ligament sports injuries in Germany. Furthermore, if the person concerned has an occupational restriction (e.g. craft trades), the operation is also necessary here.
The clinical results of the surgical treatment of smokers are significantly worse than those of patients who refrain from tobacco consumption.
The following techniques all relate to the preservation or reconstruction of the anterior cruciate ligament. Operations on the posterior cruciate ligament are comparatively rare. They are listed at the end of this paragraph.
The standard procedure is still cruciate ligament surgery with the use of a tendon or allograft implant, which replaces the cruciate ligament as anatomically precise as possible.
Cruciate ligament surgery
The most common surgical techniques used are reconstruction of the torn cruciate ligament. The remnants of the severed tape are largely removed and replaced with a new tape. The new ligament can be made from the body's own tissue ( autologous ) or from the tissue of the deceased ( allogeneic ) or from another species ( xenogenic ) .
While in the 1980s an operation was usually performed immediately or at least shortly after the injury, the “ two-stage ” procedure has been preferred since the 1990s . After a clinical examination, often supported by the findings of a magnetic resonance tomography (MRT), the arthroscopy is performed with resection of the torn cruciate ligament and treatment of any meniscus injuries in preparation for the second operation (cruciate ligament plasty). The arthroscopy is followed by a physiotherapeutic treatment to reduce the swelling of the knee and strengthen the muscles. After the symptoms have subsided, the actual cruciate ligament operation is performed around six weeks after the first arthroscopy.
This two-stage method is still preferred by many surgeons to this day, since a higher rate of arthrofibrosis and thus massive restrictions on movement was observed after the operation in the "immediate operations" .
In recent years, however - thanks to more standardized methods, but also for the purpose of possible shortening the treatment process - more and more "one-time" operations have been performed again. The stumps of the torn cruciate ligament are usually only partially removed; often just enough to prevent the stump from becoming trapped in the joint. Clinically proven cruciate ligament injuries can be treated immediately after the injury , especially in high-performance and professional athletes , as long as the knee is still largely free of inflammation.
All reconstruction techniques try to restore the properties of the original cruciate ligament as well as possible. The anterior cruciate ligament has a multiaxial fiber structure. None of the currently used grafts achieve this structure. All reconstructions also lack proprioception . A healthy cruciate ligament has mechanoreceptors that the grafts lack. On the mechanoreceptors can afferent signals to the spinal cord led and motor neurons via the γ-loop spindle unloaded. This control loop influences the sense of movement, force and position of the knee joint and is an important factor for its stability. The entire proprioception of the affected knee is significantly worsened by the loss of the sensory system. For this reason, no currently known surgical technique achieves the quality of the uninjured ligament after reconstruction of the cruciate ligament. There is a controversial debate about which technology or which transplant comes closest to the properties of an uninjured cruciate ligament.
Graft selection
In the case of the graft materials used to replace the torn anterior cruciate ligament, essentially the body's own (autologous) grafts have become popular since the 1980s. At the moment, the kneecap ligament , the quadriceps tendon and the semitendinosus tendon are mainly used. The choice of graft has been the most discussed topic in knee surgery for years in specialist circles.
Strips from the iliotibial tract or the fascia of the gastrocnemius muscle are rarely used . Due to the morbidity and invasiveness of the body's own tendon grafts, synthetic ligament replacement materials or cadaverous grafts could be an obvious alternative. The guidelines of the German Society for Trauma Surgery recommend free multi-strand tendon grafts from the pes anserinus group (semitendinosus tendons or semitendinosus and gracilis tendons ) as well as from the patellar tendon and its bone attachments.
According to a study in the United States in 2006, around 46% of all anterior cruciate ligament surgery was performed using BTB, 32% using a hamstring and 22% using allograft. In Europe, however, reconstructions were performed in 84–90% of operations with hamstring tendons and in only 10–14% of operations with the patellar tendon; the use of allografts or artificial ligaments plays no role with approx. 1.4%.
Kneecap tendon
The kneecap tendon (technically: patella (r) tendon , ligamentum patellae ) is a very large and strong tendon, so in many cases it is the method of choice. However, it is only half as elastic as the natural one Cruciate ligament. In the reconstruction of the cruciate ligament by autologous transplantation of the patella tendon this is with attached bone parts ( engl. : Bone tendon bone = bone-tendon-bone ; BTB-technology) removed and pulled through widened channels (8-10 mm diameter) in the tibia or femur . The length of the upper and lower bone blocks are each about 20 mm. The most stable anchoring of the bone ends of autologous graft (ger .: graft = transplants without blood supply, which is why both here and in the further explained in the following section Semitendinosustechnik of autograft is spoken, with Greek αὐτός = itself ) is the fixation with the so-called interference screws achieved . This is particularly important with regard to an early functional mobilization.
The support after the operation with an orthopedic splint ( orthosis ) is often not necessary, so that the risk of muscle atrophy is lower than with other procedures. This advantage is particularly interesting for athletes who want an early return to old performance.
Since the kneecap tendon is only half as flexible as the actual cruciate ligament, it can take up to 18 months before you can participate in so-called "stop-and-go" sports again.
Semitendinosus tendon
The half-tendon muscle ( semitendinosus muscle ) pulls from the knee joint to the thigh bone on the side facing the middle and is part of the so-called "goose foot" Pes anserinus superficialis , which is also formed from the tendons of the gracilis muscle and sartorius muscle .
The tendon (transplant) is removed through a middle cut on the shin, just below the knee, using a so-called tendon stripper or ring stripper (tendon cutter , also harvester from to harvest = 'to harvest'). Depending on the length, the tendon is folded three or four times with a certain thread technique, twisted, fixed and guided through a hole through the lower leg to the thigh and also fastened there. Since the beginning of the 21st century, a minimally invasive technique for easier and faster removal of the tendon from the hollow of the knee with better cosmetic results has been available.
The semitendinosus tendon is four times stronger than the kneecap tendon. This technique was equivalent to the patella tendon technique until around 2003. Since then, this technique has established itself as the so-called "gold standard", since the removal site in particular heals less painfully. If the semitendinosus tendon is too short or too thin, the gracilis tendon is also removed (STG technique; semitendinosus and gracilis tendons). However, this does not make the transplant more resilient. Some surgeons always remove both tendons. Both the semitendinosus and Gracillis tendons are required in particular for the plastic of the posterior cruciate ligament, which makes removal from the opposite side necessary, especially in the case of an additional external ligament instability that needs to be treated.
The most modern surgical technique is the double bundle technique . Two bundles (anteromedial and posterolateral) are inserted into the knee using four bone canals. Better mimicking of the anatomy gives more stable results. However, this procedure is technically demanding and is currently (2010) only carried out in specialized centers. The fixation of the two grafts takes place exclusively extra-articularly using endobuttons .
Quadriceps tendon
Following the principle mentioned above, a part of the tendon of the four-bellied thigh muscle including a kneecap bone cylinder is removed from above the kneecap and implanted as a cruciate ligament as shown above. As a so-called press-fit method, it is used without additional screwing. The advantage is that the tendons are stronger than the gracilis tendon. Compared to the patellar tendon, there is significantly less pain when kneeling, since the pressure does not put on the scar. The disadvantage is that muscle wasting of the quadriceps femoris muscle often occurs after the operation . The quadriceps tendon has so far only been used by relatively few surgeons to reconstruct the cruciate ligament.
Allograft
A so-called allograft is a corpse transplant. In addition to the three previously mentioned tendons, prepared Achilles tendons and the tibialis anterior tendon can also be used for this. A positive effect of using an allograft is that there is no morbidity with regard to removal . Further advantages are the shorter operation time, smaller operation scars and reduction of postoperative pain. Originally, allografts were only used for revision surgery and for the reconstruction of the posterior cruciate ligament. In the meantime, allografts are also increasingly used for the primary reconstruction of the anterior cruciate ligament.
Untreated frozen grafts are used. The originally used methods of sterilization ( radiation or ethylene oxide ) damaged the biomechanical properties of the transplant or led to rejection reactions . With the untreated transplants, however, the HIV problem arises . The allografts transplanted in Germany come mainly from the clinic's own stocks or from Eurotransplant , as the trade and distribution of organ parts is prohibited by law in Germany. The brain-dead living donors are examined for the HI virus, among other things. The risk of infection of the recipient is thus limited to the period of the " diagnostic gap " and is classified as very low.
The frozen allografts do not trigger a rejection reaction. A number of studies confirm that the allografts have similar values to the autologous transplants, both in the short and long term. In terms of quality, allografts are in no way inferior to autologous transplants. Whether an autologous or an allogeneic transplant is used to reconstruct a cruciate ligament is ultimately a decision made by the doctor and the patient. A major problem is that there are far too few dispensers for allografts to even come close to meeting the demand.
Synthetic reconstruction materials
Synthetic cruciate ligament prostheses, i.e. implants made from carbon fibers , polyester , polypropylene , Gore-Tex or bovine collagen , for example , were used primarily in the 1980s. They are no longer used because of their inadequate biomechanical properties and an increased number of intra-articular complications. These complications were mostly joint effusions and reactive synovitis (inflammation of the inner layer of the joint capsule). The complications were mainly caused by abrasion particles that lead to foreign body reactions in the joint . The failure rate for these synthetic cruciate ligament prostheses was between 40 and 78 percent.
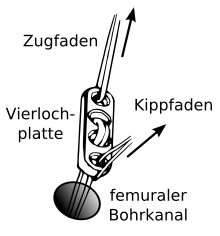
Attachment of the graft
In the early 1990s, the kneecap tendon transplants were fixed with so-called titanium interference screws as fixation at both ends of the transplant, sometimes only screwed on one side, and attached to the thighbone with a so-called endobutton that is “threaded” through the transplant. The Endobutton consists of a loop made of a non-resorbable thread material with a titanium tilt button (four-hole plate), which is tilted after being passed through the bone canal. Later, the titanium screws were replaced by the so-called bio- screws ("bio-screws", which are auto-resorbable interference screws) that are used today , which make a renewed intervention to remove material unnecessary. These screws are made of degradable polymers, such as poly- L -lactide (PLLA) or poly- ( L -co- D / L -lactide) (PLDLLA). A hybrid technique of bio-screw (as intra-articular fixation) and femoral / tibial endobuttons (as extra-articular fixation) can also be used. With the so-called " Press-Fit-Technique-Fixation ", which appeared around 1995, the screw fixation with the BTB technique (bone-tendon-bone technique) can be completely dispensed with. Here, the bone ends are trimmed conically so that a firm tilting in the drill channels is guaranteed. From 1996 surgical robots appeared that automatically generated the drilling channel with a diamond milling head. They could not assert themselves because they did not produce any clearly better operational results and caused high costs (intensive in terms of personnel and equipment).
In the case of semitendinosus and gracilis transplants (STG), bio- screws are usually used for fastening. Implant-free fixation has also been possible here since the late 1990s. With this technique, the end of the semitendinosus and gracilis tendon graft is tied and the femoral canal is drilled about 4 mm narrower in the direction of the joint than at the point remote from the joint. The graft is inserted into the joint through the femoral hole. The knot of the transplant sits in front of the narrower part of the canal. Measurements have shown that joint stiffness and maximum load are similar to other techniques. By knotting the tendon ends, interference screws (implants) are unnecessary. The protagonists of implant-free fixation see this as a cost advantage. Since no implants are used, no problems can arise with these materials. The disadvantage, however, is the considerably larger canal in the thigh bone.
When fixing the grafts with interference screws, it is important to avoid the so-called " bungee effect " and the " windshield wiper effect " that the fixation is close to the joint surfaces.
Graft harvest morbidity and invasiveness
The quality and technology of the reconstructed cruciate ligaments has been steadily improved since the first cruciate ligament surgery in 1917 and today has very high success rates. The high success rates of around 90% change the patient's expectations. A secondary aspect of autologous transplants is therefore becoming increasingly important: the morbidity and invasiveness of the transplant removal. It now has a significant influence on patient satisfaction, which is primarily determined by pain and mobility.
The removal of the patellar tendon is often more painful than that of the other autologous tendons. Up to 60% of patients complain of pain when kneeling. Patellar tendon transplants are therefore usually not recommended for patients with frequent kneeling activities. The pain in the knee causing the patellar tendinitis , patellar tendinitis , patellofemoral crepitus and infrapatelläre contractures. The frequency of these symptoms varies and ranges from 4 to 40% of patients depending on the study. A major cause of the complications are apparently injuries to the Hoffa fat pad , which can lead to a scarred contracture (shortening of the patellar tendon) and fibrosis . This in turn leads to limited mobility of the patellar tendon and its sticking to the leading edge of the shin bone. A number of studies have shown that the patellar tendon shortens after the transplant has been removed. The shortening can be in the range between 2 and 7 mm. Too much shortening of the patellar tendon can lead to patellofemoral osteoarthritis. Fissures of the kneecap have been observed in individual cases , which can lead to a fracture of the bone under high stress . The risk of a patellar fracture is in the range of 0.1 to 3%. It can be further minimized by carefully removing the graft. If, for example, a hollow milling cutter is used to remove the patellar bone block, the risk of the formation of predetermined breaking points is also avoided. Removal of the patellar tendon increases the likelihood of a patellar tendon rupture.
Removing a semitendinosus tendon (hamstring) to reconstruct the anterior cruciate ligament can also lead to complications. For example, the flexion strength of the hamstring muscles is reduced in the first few months after the tendon is removed. Some patients also complain about the occurrence of patellofemoral pain with this transplant method . The causes of the pain are obviously a disturbed patellofemoral movement in the affected knee, as well as the shortening of the quadriceps muscles due to the removal of the hamstring. Pain caused by harvesting the semitendinosus tendon is rather rare and then only of short duration. The simultaneous removal of the semitendinosus and gracilis tendons can disrupt the internal rotation of the knee joint in the long term. According to individual examiners, the hamstring tendons can largely regenerate completely after the transplant has been removed. However, they usually change their position and are then a little closer to the body (proximal).
The proportion of operations in which the quadriceps tendon is used to reconstruct the cruciate ligament is still quite low. The data on the morbidity of harvesting this tendon are correspondingly poor. In the existing studies, the results are sometimes very contradicting. Some authors report a significantly lower removal morbidity compared to the removal of the patellar tendon , while others write of a functional impairment and significant pain.
Typical sequence of an anterior cruciate ligament reconstruction
This example describes the process of reconstructing the anterior cruciate ligament by transplanting an autologous semitendinosus and gracilis tendon. In the 1980s, the classic open cruciate ligament operation via the Payr access was initially replaced by the mini-arthrotomy . Almost all cruciate ligament reconstructions are now carried out using minimally invasive arthroscopy. Open surgery is only performed in exceptional cases, for example in the case of very complex knee injuries.
anesthesia
The procedure can be performed under general anesthesia ( general anesthesia ) or under regional anesthesia . Both procedures have advantages and disadvantages for the patient. Spinal anesthesia , epidural anesthesia (PDA, spinal cord anesthesia ) and combined spinal and epidural anesthesia (CSE) are possible regional procedures . Another form of regional anesthesia that is often used in addition to the aforementioned forms of anesthesia is the femoral catheter. In this way, the pain in the affected knee after the operation (postoperatively) can be suppressed ( femoral nerve block ). For this purpose, a local anesthetic is brought into the vicinity of the pain-conducting nerve, the femoral nerve, with the help of a catheter . A complete blockage of the knee is not possible with this alone. The fibers of the femoral nerve run from the lumbar spine to the knee joint. A tube as thin as a hair transports the pain medication in the groin area to the femoral nerve via a small dosing unit . Blocking the femoral nerve not only numbs the pain, but also limits the feeling, strength and mobility of the leg. The catheter is removed three to five days after the operation. The combination of femoral catheter and thigh tourniquet during cruciate ligament reconstruction has described disorders of the thigh muscle function.
Arthroscopy
The actual procedure begins with the introduction of the arthroscope into the patient's knee. The diagnosis of a "cruciate ligament tear" can thus be confirmed again. Other injuries, particularly the meniscus, can be treated prior to the reconstruction of the cruciate ligament.
Removal and preparation of the tendon
The first surgical procedure is to remove the transplant tendon . An approximately 4 cm long skin incision on the inner tibial head, above the pes anserinus , enables the removal of the body's own (autologous) semitendinosus or gracilis tendon or both tendons. The tendons are removed with a so-called "tendon stripper" and are about 28 cm long. The tendons are pre-tensioned on a special device and sewn together as a multiple strand, for example a “quadruple”, four times. The length of the graft is then about 7 cm and has a diameter of at least 7 mm. The transplant is fixed to the fixation devices provided (e.g. Endobutton) using a special thread. The special thread is not bioabsorbable.
Removal of the cruciate ligament
remnants and drilling of the bone canals Arthroscopically, the remnants of the torn anterior cruciate ligament are removed. A motor-driven suction cutting tool ( shaver ) and / or a high-frequency (HF) ablation device is used for this purpose. It is advisable to leave a remnant of the stump on the tibial head in order to preserve some proprioception and to minimize the penetration of synovial fluid into the tibial canal. With the help of a targeting device, the position for drilling a canal through the head of the tibia is sighted and then drilled. The diameter of the drill channel is adapted to the diameter of the graft. A targeting device for the drilling is attached to the femur through the canal of the tibia, or more precisely today through an additional anteromedial arthroscopic access. With the help of this aiming device, a canal is drilled into the femur. This channel can taper upwards (blind hole) and has a length of about 35 mm. The wider part of the channel is for receiving the graft, the narrower part for pulling through the graft suspension.
Pulling in the graft
The graft is pulled into the drill channels from bottom to top using two pull cords. The transplant is attached to the femur with the help of a hollow screw (transfix screw). The end protruding from the end of the tibial canal is pretensioned and fixed with an interference screw (delta screw) by clamping. Finally the wounds are sutured. The duration of the operation is typically in the range of 45 to 90 minutes.
After the operation,
positioning in the extended position immediately after the operation is decisive for the definitive function. This should be observed for 24 hours. This positioning prevents a postoperative stretching deficit, which otherwise often develops and which can require weeks of physiotherapy to eliminate it. The day after surgery, drains are usually removed from the knee wounds. The operated leg may only be partially loaded up to the fifth week after the operation, as the transplant must grow into the bones in the drill channels. A knee brace is used to protect the sensitive graft during this period . Rehabilitation can usually begin after the fifth week.
Possible complications after reconstruction of the anterior cruciate ligament
As with any surgical intervention, reconstruction of the cruciate ligaments with the two transplants commonly used today (patellar tendon and hamstring) can lead to complications. In addition to the general risks associated with operations, such as bleeding , wound infections , impaired wound healing , thromboses , injuries to blood vessels or nerves, there are specific complications. Depending on the author, different complication rates of up to 26 percent are given. The most common complications are the failure of the transplant, for example due to tearing, re-rupture or loosening, and above all restricted movement of the knee joint.
The previously shown morbidity of the transplant removal can also be added to the complications.
- Loss of movement

Cyclops is secondary arthrofibrosis and a possible complication of cruciate ligament reconstruction. In around 2 percent of all patients, after a cruciate ligament reconstruction, a cyclops is the cause of a loss of mobility when extending the knee joint.
Loss of movement is a serious complication after anterior cruciate ligament reconstruction. By definition, it is present when the leg does not fall below an angle of 10 ° when the leg is extended and an angle of 125 ° cannot be exceeded when the leg is bent. The loss of the ability to stretch the joint is more common than that of the ability to bend and is also more serious for the patient. The cause of loss of movement is usually an inflammation-related increase in connective tissue - a fibrosis , more precisely arthrofibrosis .
Graft Failure
The incidence of graft failure is around 4.3%. The causes of failure of a transplant can be divided into three groups:
- surgical errors,
- biological failure, due to insufficient healing of the transplant and
- Renewed cruciate ligament rupture.
In one study, 52 percent of transplant failures were iatrogenic , or surgical errors caused by the doctor. In 25 percent of the cases the cruciate ligament ruptured again, in 8 percent inadequate incorporation of the transplant, in 3 percent restricted mobility and in 3 percent the synthetic implants used also failed. In 9 percent of the cases of transplant failure, the cause could not be precisely assigned. In general, the surgeon's surgical ability is of great importance for the success of a reconstruction of the anterior cruciate ligament. Typical surgical errors are, for example, incorrect placement of the drill channel, inadequate fixation of the transplant, insufficient tension on the transplant and insufficient notch plastic with subsequent impingement .
The renewed rupture of the cruciate ligament can be caused, among other things, by overly aggressive rehabilitation, a lack of patient compliance or too early resumption of sporting activity with excessive stress on the implant.
- Septic arthrithis
A septic arthritis (bacterial arthritis) is a relatively rare, but very serious complication of a cruciate ligament reconstruction. The incidence rates are in the 0.3 to 1.7 percent range. Septic arthritis is associated with high morbidity, mostly lengthy hospital stays and often with poor clinical results.
In a study in the United States, the rate of serious infections after cruciate ligament reconstruction was 0.75 percent. The rate for autografts was 1.2 percent and for allografts 0.6 percent. The administration of antibiotics is mandatory after postoperative infections.
In Germany, patients are prescribed prophylactic antibiotics in 62 percent of all arthroscopies in order to avoid infections such as septic arthritis.
Other complications
Postoperative thrombosis has an incidence of 1.2 percent. Malignant neoplasms (malignant tumors) that develop after cruciate ligament surgery are extremely rare . So far (as of June 2010) only three cases have been described in the literature.
Cruciate ligament suture
- → see also the section on medical history
Until the 1980s, the primary suture method was preferred, for example for intraligamentous tears. In the case of the primary suture, the severed ends of the cruciate ligament were sewn back together for repair . This therapeutic approach was first carried out in 1895. The study results at that time on the primary suturing of cruciate ligament tears were not satisfactory. The failure rates in the first five years after the operation were over 20 percent, depending on the study. In the following years, the primary suturing of the cruciate ligament without augmentation was more and more abandoned as a therapy in favor of the reconstruction of the anterior cruciate ligament. Other subsequent long-term studies have shown a deterioration in the results over longer periods of time, which is why the sole primary suture in the surgical technique used at that time is no longer a therapeutic option today. The cause of the poor results was insufficient biomechanical stability of the knee joint during the healing process. As a result, in many cases no functionally adequate scar tissue could develop to ensure the required knee stability.
A further variant of the cruciate ligament suture was the reinforcement of the healing cruciate ligament through so-called augmentation. Various synthetic tape materials or the body's own tissue were used for the augmentation. The reinforcement can take place intra-articularly (inside the joint) or also extra-articularly (outside the joint). These procedures at the time are also generally viewed as outdated.
Special case of a bony avulsion
The bony tear or avulsion of the anterior cruciate ligament from the bone (tibia or femur) is much rarer than its intraligamentary rupture and is by definition not a cruciate ligament tear. This special case occurs more often in children, especially in the area of the cruciate ligament attachment on the shin eminentia intercondylica and has a generally good chance of completely healing again by re-fixing the tear - for example with screws or wire sutures. During the arthroscopic refixation of the cartilage-bone scales that support the cruciate ligament, a good overview is of decisive importance in order to avoid the trapping of the transverse ligament (between the menisci ) under the fragment. Otherwise the mini-open technology is preferable. In general, care should be taken not to block the growth plate with the implants ( screws or wire sutures) .
Cruciate ligament-preserving operations
- → see also article cruciate ligament retention
Surgical methods that preserve the cruciate ligament are still young procedures that do not require a replacing tendon graft . They can only be used within the first three weeks after a cruciate ligament tear. This time limit is due to the fact that the existing healing capacity of a cruciate ligament is to be used, which wears off fairly quickly. The desired natural scarring process of the cruciate ligament is achieved through biomechanical stabilization of the knee joint, an anatomical reduction of the injured ligament structure and a microfracture ( healing response ).
Two methods are currently used: a first treatment approach is dynamic (spring mechanism) based, the second is based on rigid, inflexible stabilization of the knee joint. In the dynamic method , the cruciate ligament is repositioned with bioresorbable sutures and the knee is stabilized with a thin, very tear-resistant implant thread. The flexible dynamics of the spring element in the shin ensure that the healing ligament is relieved during all flexion and extension movements. In the inelastic method, a rigidly fixed polyethylene tape is used to stabilize the knee, as well as non-resorbable sutures and small anchors to return the torn cruciate ligament to the original tear point until it has grown back on.
Data published so far show that good results can be achieved with a very selected indication.
Therapy prospects
In contrast to the inner and outer ligaments, the two cruciate ligaments are not able to grow together again on their own after a tear by immobilization. In the case of an inner ligament tear, for example, a support device (splint) is sufficient, which must be worn for about six weeks so that the two ends can heal and the tear heals. This is not the case with the two cruciate ligaments located inside the knee. The reason for this is not exactly known. Several factors are discussed. The synovial fluid that surrounds the cruciate ligaments may be a medium that prevents such a healing process. Changes in cell metabolism after the injury and intrinsic deficits, such as the gene expression of the cells that form the cruciate ligaments, are also held responsible for this effect.
In research, therapy concepts are aimed at activating the same abilities in the cells of the torn cruciate ligaments as, for example, in the cells of the outer and inner ligament. In principle, the cells of the cruciate ligament, such as the cells of the inner ligament, are able to proliferate and revascularize after a rupture . This was demonstrated histologically and immunohistochemically . Even one year after the rupture, the cells are still able to produce collagen within the ligament fragments. The ability to migrate cells into the wound area has also been demonstrated. Nevertheless, no support structure (scaffold) is formed in the knee for the tissue structure that connects the torn collagen fiber bundles of the cruciate ligament with one another. The ends of the torn cruciate ligament swayed aimlessly back and forth in the synovial fluid. One hypothesis assumes that the lack of extracellular matrix proteins and cytokines in the area of the wound, which are essential for building up the support structure, prevents self-healing. An indication of this is that considerable amounts of fibrinogen , fibronectin , platelet-derived growth factor A (PDGF-A), TGF-β1 , fibroblast growth factor (FGF) and von Willebrand factor (vWF) are detectable during the healing process of the inner ligament that are missing in cruciate ligament ruptures. Despite the bleeding in a cruciate ligament tear, no fibrin platelets are detectable near the injury. One possible cause is the presence of higher concentrations of the enzyme plasmin . Plasmin is able to catalyze the breakdown of fibrin ( fibrinolysis ) . It arises from the increased expression of the enzyme urokinase , which in turn catalyzes the conversion of plasminogen into plasmin.
The biological stimulation of the construction of a support structure, which enables the healing process of the torn cruciate ligament in the knee, is a potential future therapy concept. The administration of growth factors such as PDGF, TGF-β and FGF could upregulate the proliferation and migration as well as the production of collagen in vitro . In the model organism rabbits , injections of hyaluronic acid resulted in increased vascularization and increased production of type III collagen. In the domestic pig animal model , the injection of a collagen-rich hydrogel results in an improved healing process in a sutured cruciate ligament, with significantly increased ligament strength.
All related concepts of tissue engineering are still in the early stages. Initial and short-term results show that improved ligament healing can be achieved with biologically stimulating factors.
Healing-Response Technique
The American surgeon Richard Steadman developed the healing response technique in the early 1990s. This therapy method is only possible with fresh anterior cruciate ligament tears, with a tear in the thigh bone or with a tear in the synovial covering . In 80% of all ruptures of the anterior cruciate ligament, the tear occurs on the femur. The process is controversial as the results published so far are inconsistent. A comparative study showed that the results did not differ significantly from those of conservative therapy, while other studies documented the advantages of this treatment method.
The healing-response technique is based on the assumption that undifferentiated stem cells can differentiate into tendinocytes (wing cells) when subjected to mechanical stress - according to Wolff's law . Any accompanying injuries are first treated using arthroscopy. Then the bone marrow in the area of the cruciate ligament is opened with an awl in up to ten places (microfracture) so that stem cells can emerge from the marrow. It is important that there is sufficient blood leakage from the bone marrow. Then the cruciate ligament is repositioned at its attachment point in the coagulum and the knee joint is stretched. Treatment is inpatient, typically for two days. Without drainage, the knee joint is fixed with a splint for around four to six weeks in a 10 ° flexion. This is followed by intensive training. After an average of three months, the patient treated in this way is able to practice competitive sports again. The procedure must be performed within a few days of the injury. The success rate is over 80%. Failures can be treated with cruciate ligament surgery. The procedure may also be useful for treating tears of the posterior cruciate ligament.
Surgical treatment of the posterior cruciate ligament tear
The operation of the posterior cruciate ligament is considerably more difficult than that of the anterior and is rather the exception. The tendency towards healing is also quite high with conservative therapy. Surgical intervention is usually only indicated for complex knee ligament injuries . There are currently three competing surgical procedures established for posterior cruciate ligament rupture. These are:
- The anatomical reconstruction of the anterolateral main bundle in the single incision technique using hamstring tendons such as the semitendinosus muscle
- The anatomical reconstruction of both bundles
- The tibial inlay technique
Physiotherapy for rehabilitation after cruciate ligament surgery
The aim of therapy should not be the sole restoration of stability, but rather the maintenance of the entire joint function. That means stability, including the feeling of a stable knee joint, free joint movement and freedom from symptoms.
After the operation, functional exercises are carried out at an early stage (sometimes passively using a motorized movement splint) and the patient's mobility is established with forearm crutches and, under certain circumstances, with a knee orthosis. This is followed by physiotherapeutic treatment, which, depending on the type of operation and the school, should lead to full stress on the operated knee after about two weeks. It is recommended to do tension exercises. This is supposed to activate the muscle groups. From about the third week you can start cycling lightly. After about six weeks, exercises on the sports top or mini trampoline can be performed under supervision. Sports ability for light running training exists from around the third month after the operation. After about six months, loads such as jumping can be added. Overall, the rehabilitation phase lasts an average of six to nine months before full sports ability is achieved. Complete healing (remodeling phase) of the anterior cruciate ligament is only complete after one year.
The follow-up treatment after the operation essentially differs only marginally. There are fixed standards in physiotherapeutic treatment that differ only insignificantly. Clear follow-up treatment schemes should also be reflected in the treatment here, depending on the surgical method. The experience and work of the physiotherapist is therefore of decisive importance for the healing process.
forecast
Functional instability can remain in the affected knee joint even after optimal therapy. This instability can lead to incorrect loading of the joint body and thus cause consequential damage. Typical consequential damages are secondary cartilage damage, degeneration of the posterior horn of the medial meniscus and a significantly increased risk of knee osteoarthritis (gonarthrosis).
Several studies show that if the anterior cruciate ligament tears, the likelihood of developing knee osteoarthritis is significantly increased. About 50 to 70% of patients with a cruciate ligament tear show radiographic changes in the knee after 15 to 20 years . If the cruciate ligament tear is accompanied by injuries in the knee - such as a meniscus tear, for example - the likelihood of gonarthrosis increases further. During this period the osteoarthritis of the knee has reached Ahlbäck grade I to II and is usually without clinical symptoms. The progression is usually relatively slow. Older studies assume that in most cases gonarthrosis will probably only become clinically relevant 30 or more years after the rupture of the anterior cruciate ligament. Other studies report that as early as 10 to 20 years after the cruciate ligament rupture, functional limitations of the knee joint, combined with pain, caused by arthritic processes in the knee. The prognosis is generally very dependent on age, gender, genetics , body weight, muscle strength, physical activity and possible renewed knee injuries. American athletes have tears of the anterior cruciate ligament five times as often as athletes, although American athletes include American football, a sport that is not entirely harmless for the knees. Ford KR, Myer GD & Hewett TE (2003) therefore examined the landing behavior of volleyball players after jumping on both legs. They found that the differences in strength between strong and weak legs were significantly greater for women than for men, that valgus positions are significantly more common in women’s knee joints , and that there is a connection between valgus positions and the difference in strength of the legs. Since surgically treated cruciate ligament ruptures lead to a considerable risk of re-injury if the sport is continued, the Americans MV Paterno, LC Schmitt, KR Ford u. a. (2010) 56 athletes (35 women, 21 men) from sports with sudden changes of direction (including soccer and American football ) who had successfully operated on the anterior cruciate ligament were systematically tracked for a year to determine whether there are any peculiarities which can be used to predict a new cruciate ligament tear. During this period, 13 suffered new cruciate ligament injuries. For this purpose, a 3-dimensional movement analysis was carried out on all 56 of the deep jumps and the stability of the posture was measured with 4 video cameras and a Kissler force plate. The kinematics, kinetics and postural stability were determined to find out whether matching movement / posture anomalies were found to be statistically significant in the re-injured. With this method the probability of re-injury could be predicted very well. The specific parameters included an increase in the movement of the valgus, greater asymmetry in the movement of the internal knee extensors at the beginning of contact with the ground, and a deficit in postural stability when standing on one leg on the affected leg. Independent of these measurements, a contralateral hip rotation during the first 10% of the landing phase also allowed a (albeit less) good prediction of the re-injury of the anterior cruciate ligament. The Catalans Ferrer-Roca V., Balius Matas X., Domínguez-Castrillo O., u. a. (2014) examined 35 football players (professionals and semi-professionals) from Barcelona in the 1st Spanish League on 2 days at the beginning of the preparation time after the summer break with video analysis and 2 force plates in their movements with regard to possible intrinsic risk factors. The authors used the tests by Paterno et al. a. (2010), since they assumed that the athletes for whom the Americans predicted a risk of re- injury could also have a risk of first-time injury. They identified the same problems and tried to establish guidelines as to when countermeasures should be taken in training: 14.3% of the players had a valgus deviation of ≥ 20 degrees in the knee when landing in the low jump. In the literature, even ≥ 16 degrees is considered problematic. 31.4% of the players had functional (strength) deviations in the legs of more than 15%. Since this 15% is the maximum when a player can be reintegrated into team training after injuries, this is also a useful guide value, especially since there was no statistical correlation between the shooting leg and the stronger leg. Countermeasures were taken for the players who showed both discrepancies.
In the case of cruciate ligament ruptures that are not treated surgically, the risk of knee osteoarthritis after 20 years is 60 to 100% over several studies. In comparison, patients with an anterior cruciate ligament reconstruction have a 14 to 16 percent risk and with an additional meniscectomy a 37% risk of gonarthrosis.
In the long-term study of a small cohort of 19 top athletes with untreated cruciate ligament ruptures, 8 of the athletes (= 42% ) had a knee prosthesis after 35 years .
According to the VBG accident insurance , the average downtime in the top German leagues of basketball, ice hockey, football and handball in Germany was around eight and a half months. Tears in the anterior cruciate ligament accounted for 0.5 percent of all injuries, but account for up to 20 percent of downtime.
Depending on the sport, around 60 to 80 percent of athletes return to their previous level after a cruciate ligament rupture.
Prevention
A cruciate ligament tear has significant consequences for the person concerned. This type of injury is therefore one of the most feared by athletes. For professional and competitive athletes, a cruciate ligament rupture means a lengthy break from training and competitions - despite continuously improving treatment options. Until the 1990s, a cruciate ligament tore usually led to the end of a career. For professional athletes, as well as their clubs and sponsors, the result is still considerable loss of income. As a rule, after the ligaments have been restored and competitions restarted, it takes a further months for the athlete to regain their original level of performance. In the amateur and hobby area of sport, society incurs considerable costs due to lost work times, treatment and rehabilitation measures, to which the long-term costs due to premature knee osteoarthritis are added. In sport, with appropriate physiotherapy, regeneration times of nine months are expected on average.
The prevention , ie the prevention of a cruciate ligament injury, therefore plays an increasingly important role. Basically, it seems possible that certain training methods can reduce the likelihood of a cruciate ligament tear. Since a number of pathomechanisms that promote a cruciate ligament rupture have not been adequately understood for a long time, it is still largely unclear which exercises have a preventive character or even why they reduce the risk of injury. In the meantime, large research efforts are therefore being undertaken in many countries, on the one hand to elucidate the risk factors and pathomechanisms of a cruciate ligament tear and, on the other hand, to be able to counter this type of injury with appropriate measures derived from them. The most successful so far have been Paterno MV, Schmitt LC, Ford KR u. a. (2010), who were able to predict the probability of cruciate ligament tears with a 94% probability from the movement behavior during deep jumps. They showed that large differences between the strength of the two legs and a valgus position in the knee joint on landing were the greatest risk factors, but that instability of the back can also contribute to the danger. Since a valgus deviation of more than 16% and strength differences of more than 15% are viewed as problematic (and in this case rehab is not yet completed), appropriate leg strength training seems appropriate in addition to CORE training for the back.
Special exercises
So far, there are no standardized exercises to prevent cruciate ligament tears without external interference. Some studies have shown that more varied exercise programs have a greater positive effect than individual exercises. Plyometric exercises for the lower limbs, stretching exercises (stretching) , for targeted control of the hull, for gestärken perception of body movement (proprioception) and improved decision making, positive effects in the prevention seem to have. This reduces the forces when the athlete lands after a jump as well as the moments that act in varus / valgus. In addition, muscles are activated that can partially absorb moments of force that act on the knee.
In a study of more than 1,400 football players, a positive effect was due to a special warm-up (warm-up) can be achieved. Compared to the control group, the number of anterior cruciate ligament tears decreased overall by a factor of 1.7. If one only looks at the cruciate ligament tears without external influence, the frequency in the group with the special warm-up program was even lower by a factor of 3.3. The focus of the warm-up exercise is on neuromuscular control of the knee joint. In other studies, electromyography has shown that neuromuscular exercises have positive effects on the semitendinosus muscle before an athlete takes off and lands.
A study from Italy came to similarly positive results. In the mid-1990s, a total of 600 football players from 40 semi-professional and amateur teams took part. Half of the teams trained for an additional 20 minutes each day using a special sensorimotor training program that contained proprioceptive elements. The exercises were carried out , for example, with a balance board . The incidence of anterior cruciate ligament injuries was observed over three game seasons. In the participants in the special training program, the incidence of cruciate ligament injury was significantly lower than in the control group. Some authors see this study as proof of a prophylactic effect of coordinative training. Common proprioreceptive training aids are, for example, "wobble boards" and "sports tops". These give the exerciser an unstable surface, which means that he is constantly forced to keep his body in balance.
Another evidence-based study from Norway with more than 1,800 handball players aged 15 to 17 also shows that a structured warm-up program with neuromuscular exercise elements can reduce the incidence of cruciate ligament ruptures by over 50%. Among other things, balance mats were used here . A study published in 2005 by the University of Münster with over 250 German handball players also came to the conclusion that proprioceptive and neuromuscular exercises can significantly reduce the frequency of cruciate ligament ruptures.
A number of sports scientists advocate that such preventive exercise elements become an integral part of training sessions in sports with an increased incidence of cruciate ligament ruptures.
Other preventive measures
A rule change at the beginning of the 2005 season in the Australian Football League meant that the frequency of a posterior cruciate ligament tear could be reduced by more than a factor of two. The rule change was to limit the approach of the Ruckman to the nudge square.
Veterinary medicine
Of the domestic animals in particular is home dog frequently affected by ruptures of the anterior cruciate ligament. However, other, non-traumatic, pathological mechanisms play a major role here. Cruciate ligament ruptures are less common in domestic cats .
Medical history
Hippocrates of Kos described a subluxation of the knee, which he attributed to a ligament injury in the knee. Galenos described in detail the importance of the ligaments for stabilizing the knee and for normal movement when walking. Previously, it was thought that the cruciate ligaments are "nerve structures". The name genu cruciata , which is still valid today and used to describe the structures that stabilize the knee , also goes back to Galenos .
Although the knee dislocations and their treatment were described in detail well into the 19th century, the function of the ligaments in the knee was completely underestimated internally in the collective term dérangement . The Wittenberg brothers Wilhelm Eduard and Eduard Friedrich Weber described in detail in their work Mechanics of Human Walking Tools in 1835 the biomechanical relationships between the components within the knee and its periphery. In their research, they looked at the abnormal movement of the tibia in a knee without cruciate ligaments. They were the first to describe the abnormal walking sequence caused by a cruciate ligament tear.
In 1845, the French Amédée Bonnet described in his 1,300-page monograph Traité des maladies des articulations (German title from 1851: For the treatment of joint diseases ) the studies he carried out on cadavers. He found, among other things, that in most cases the anterior cruciate ligament tears at its femoral (on the thigh) insertion and the rupture is accompanied by a cracking noise. Valgus flexion stress would also tear the medial collateral ligament at its femoral attachment. Bonnet also recognized that bloody joint effusion (hemarthrosis) and pain are important symptoms of the anterior cruciate ligament tear. He saw the cause of the pain in the stretching of the ligament nerves. Regarding the incidence, he wrote that "ruptures of the ligaments are much more common than is generally assumed." Bonnet was also the first to mention the phenomenon of subluxation ("... des déplacements qui font croire à une luxation incomplète"), which was only taken up again at the beginning of the 1970s by RD Galway and DL MacIntosh as a pivot shift . In his book Traité de thérapeutique des maladies articulaires , published in 1853, Bonnet wrote that immobilizing the affected knee for too long had a negative effect on the healing process. He developed the first devices for active movement against the cartilage-damaging effects of immobilization . In his remarks on the treatment of acute injuries, he was way ahead of the times. For example, Bonnet suggested cold packs for initial treatment of the injury and early, gentle exercise. In the same book, Bonnet describes a two- hinge orthosis for patients with an anterior cruciate ligament tear.
The injury of the anterior cruciate ligament was treated for the first time in 1850 by the British J. Stark in a conservative way using a plaster cast.
The bony avulsion of the anterior cruciate ligament, in which the ligamentous structures are intact, was described by French surgeon Poncet in 1875. Poncet autopsied the body of someone who had been killed in a lintel from the third floor.
The Englishman Arthur Mayo Robson (1853–1933) performed a cruciate ligament suture for the first time in 1895 on a 41-year-old miner from Featherstone - Mayo Robson called him "JB" in his publication eight years later. The patient had injured his knee in an accident in a coal mine 36 weeks earlier. On November 21, 1895, Mayo Robson opened JB's knee. He found that both ligaments had completely torn off and fixed them with catgut . He sutured the anterior cruciate ligament to the synovium and tissue on the inner side of the outer condyle . He found the posterior cruciate ligament to be too short, so he split it up to get a sufficient length. Then he attached it to the synovial membrane and the cartilage tissue on the outer side of the inner condyle. He then closed the wound with catgut and the surface with silk gut. Almost six years later, on October 24th, 1901, a colleague of Mayo Robson visited the patient, who described his operated leg as perfectly strong and was able to fully practice his old job again. He only felt pain when he put too much strain on his knee while working. The circumference of both knees was identical. Other publications also recommended primary cruciate ligament sutures in the event of an acute rupture. The Berlin doctor H. Goetjes published the first collective statistics on 30 cases with primary cruciate ligament sutures in 1913, which came to a positive result. The first criticism of sewing the tapes came in 1916 from Robert Jones , a British military orthopedist. Jones thought the stitching of the ligaments was useless and saw the natural scarring as the only reliable repair. Regardless of this criticism, the primary cruciate ligament suture should last for another 60 years, as it has been confirmed and recommended by numerous authors.
In 1976, John A. Feagin and Walton W. Curl published the results of a five-year long-term study they conducted on soldiers at West Point Military Academy . Sixty-four cadets had an anterior cruciate ligament suture during college. The long-term results were extremely negative, so that in the following period the primary suturing of the cruciate ligament without augmentation as a therapy was more and more abandoned in favor of the reconstruction of the anterior cruciate ligament. Later studies confirmed the results of this study.
The Australian surgeon James Hogarth Pringle first described a reduction on a living person at the Glasgow Royal Infirmary in 1907 , which he had carried out in 1903: “The joint was then opened into, the blood and fluid in it washed out, and it was at once seen that the anterior crucial ligament still attached to its bone insertion had been torn off the tibia and taken the spine with it; with a little trouble this was sutured, and the wound closed. "
Also in 1903, Fritz Lange from Munich used silk threads to reinforce or replace the anterior cruciate ligament. The Swiss Eugen Bircher performed the first arthroscopy in the Aarau Cantonal Hospital in 1921 .
The first reconstruction of an anterior cruciate ligament in humans was probably carried out in 1914 by the Russian surgeon Grekow. According to Erich Hesse's description , Grekow used free strips of fascia lata , a connective tissue covering the thigh. Three years later, the British surgeon Ernest William Hey Groves (1872–1944) used a stalked strip of the iliotibial tract for cruciate ligament reconstruction. He led the strip through two drill channels that extended from the epicondyle to the intercondylic fossa and from the shin to the intercondylic eminence . In doing so, he laid the foundation for modern ligament surgery.
The first replacement of a cruciate ligament with a patellar tendon transplant took place in 1935 by the German A. Wittek, after the marine surgeon zur Verth had proposed this at the congress of the German Orthopedic Society in Mannheim three years earlier .
In 1926 Edwards described that reconstruction with the tendons of the semitendinosus and gracilis muscles was possible. In 1950, Lindemann carried out a cruciate ligament reconstruction with these tendons for the first time.
In 1963, Kenneth Jones was the first to use a distal pedicled graft of the middle third of the patellar tendon. He prepared this along with the bone block along its entire length from the patella. He pulled the graft distally without a drill channel under the Hoffa fat pad. On the proximal side, he pulled it through a drill channel in the area of the cruciate ligament cavity. The first description of a BTB transplant probably comes from the German doctor Helmut Brückner in 1966. The work of Jones and Brückner forms the basis of today's cruciate ligament surgery. In the German-speaking world, one often speaks of a Brückner or Brückner-Jones sculpture.
further reading
Reference books
- W. Petersen, T. Zantop: The anterior cruciate ligament: Basics and current practice of operative therapy. Deutscher Ärzteverlag, 2009, ISBN 978-3-7691-0562-9 restricted preview in the Google book search
- MJ Strobel, A. Weiler: Posterior cruciate ligament. Anatomy, diagnostics and surgical techniques. 1st edition. Endo Press, 2008, ISBN 978-3-89756-719-1 .
- NP Südkamp, A. Weiler: Ligamentous knee joint injuries and meniscus injuries. In: W. Mutschler, NP Haas (Hrsg.): Praxis der Unfallchirurgie. 2nd Edition. Thieme, 2007, ISBN 978-3-13-101151-0 , pp. 466-467.
- A. Hüter-Becker: Textbook on the new thinking model of physiotherapy - Volume 1 movement system. 2nd Edition. Thieme Verlag, 2006, ISBN 3-13-130142-2 limited preview in the Google book search
- A. Wilcke: Anterior cruciate ligament lesion. Verlag Birkhäuser, 2004, ISBN 3-7985-1404-6 restricted preview in the Google book search
- J. Jerosch, J. Heisel: The knee joint - rehabilitation after injuries and surgical interventions. Pflaum Verlag, 2004, ISBN 3-7905-0911-6 .
- MJ Strobel: Arthroscopic Surgery. 1st edition. Springer, 1998, ISBN 3-540-63571-8 limited preview in the Google book search
Review article (Reviews)
- O. Gorschewsky: The anterior cruciate ligament. (PDF)
- HJ Eichhorn, W. Birkner: Current trends in the reconstruction of the anterior cruciate ligament. ( Memento from September 18, 2011 in the Internet Archive ) (PDF; 1.3 MB)
- P. Renström, J. Kelm: Anterior cruciate ligament - operation and rehabilitation. (PDF). In: German magazine for sports medicine. 58, 2007, pp. 392-394.
- MM Murray: Current status and potential of primary ACL repair. In: Clinics in sports medicine. Volume 28, number 1, January 2009, pp. 51-61, doi: 10.1016 / j.csm.2008.08.005 . PMID 19064165 , PMC 2642924 (free full text) (review).
- Y. Shimokochi, SJ Shultz: Mechanisms of noncontact anterior cruciate ligament injury. In: Journal of athletic training. Volume 43, Number 4, Jul-Aug 2008, pp. 396-408, doi: 10.4085 / 1062-6050-43.4.396 . PMID 18668173 , PMC 2474820 (free full text) (review).
- TE Hewett et al .: Dynamic neuromuscular analysis training for preventing anterior cruciate ligament injury in female athletes. In: Instr Course Lect. 56, 2007, pp. 397-406. PMID 17472323
- CD Harner et al .: Anterior and posterior cruciate ligament reconstruction in the new millennium: a global perspective. In: Knee Surg Sports Traumatol Arthrosc. 9, 2001, pp. 330-336. PMID 11734868
Web links
- Overview: the anterior cruciate ligament rupture. Medical magazine
- Slideshow of a cruciate ligament reconstruction ( Memento from May 6, 2015 in the Internet Archive )
Individual evidence
- ^ A b c d e W. Petersen, T. Zantop: The anterior cruciate ligament: Basics and current practice of operative therapy. Verlag Deutscher Ärzteverlag, 2009, ISBN 978-3-7691-0562-9 . ( limited preview in Google Book search)
- ^ JC Hughston et al .: Classification of knee ligament instabilities. Part I. The medial compartment and cruciate ligaments. In: J Bone Joint Surg Am . 58, 1976, pp. 159-172. PMID 1254619
- ↑ medrapid.info: anteromedial rotational instability in the knee joint. ( Memento of May 30, 2009 in the Internet Archive ) Retrieved March 30, 2010.
- ↑ medrapid.info: anterolateral rotational instability in the knee joint. ( Memento of May 30, 2009 in the Internet Archive ) Retrieved March 30, 2010.
- ↑ medrapid.info: posterolateral rotational instability in the knee joint. ( Memento of May 31, 2009 in the Internet Archive ) Retrieved March 30, 2010.
- ↑ GL Lucas et al.: A primer of biomechanics. Verlag Springer, 1999, ISBN 0-387-98456-9 .
- ↑ a b E. Luciani: An in vitro study of the tensile forces in the anterior cruciate ligament and anterior cruciate ligament replacement (ligamentum patellae and semitendinosus plastic). Dissertation. LMU Munich, 2003.
- ↑ CF Ettlinger et al .: A method to help reduce the risk of serious knee sprains incurred in alpine skiing. In: Am J Sports Med. 23, 1995, pp. 531-537. PMID 8526266
- ↑ a b c C. J. Wirth among others: Orthopedics and orthopedic surgery. Knee. Georg Thieme Verlag, 2005, ISBN 3-13-126231-1 , pp. 153f. ( limited preview in Google Book search)
- ↑ a b c C. Fink et al.: Development of osteoarthritis after rupture of the anterior cruciate ligament. In: The trauma surgeon. 97, 1994, pp. 357-361. PMID 7939737
- ↑ a b P. Hochstein u. a .: Diagnosis and incidence of injuries to the posterior cruciate ligament. In: The trauma surgeon. 102, 1999, pp. 753-762. doi: 10.1007 / s001130050477 . PMID 10525618 .
- ↑ H. Monma, T. Sugita: Is the mechanism of traumatic posterior dislocation of the hip a brake pedal injury rather than a dashboard injury? In: Injury. 32, 2002, pp. 221-222. PMID 11240298
- ↑ AT Janousek include: Posterior cruciate ligament injuries of the knee joint. In: Sports Med. 28, 1999, pp. 429-441. PMID 10623985 (Review)
- ↑ C. Haasper et al.: Knee injuries in restrained car drivers in German road traffic accidents. In: J trauma. 65, 2008, pp. 136-141. PMID 18580510
- ↑ a b c S. Bollen: Epidemiology of knee injuries: diagnosis and triage. In: Br J Sports Med. 34, 2000, pp. 227-228. doi: 10.1136 / bjsm.34.3.227-a . PMID 10854030 .
- ↑ a b c d Health Directorate of the Canton of Zurich: Rupture of the anterior cruciate ligament: surgical or conservative treatment? (PDF) Report of June 30, 2009.
- ↑ JM Hootman et al .: Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. In: J Athl Train. 42, 2007, pp. 311-319. PMID 17710181 (Review)
- ↑ D. Gehring: Knee joint control during dynamic movements - influence of gender, fatigue and equipment (PDF; 3.1 MB) Dissertation, Albert-Ludwigs-Universität Freiburg i. Br., 2009.
- ↑ JP Nicholl et al .: Injuries in sport and exercise. Sports Council Publishing, 1991, ISBN 1-872158-71-4 .
- ↑ a b A. Wilcke: Anterior cruciate ligament lesion. Verlag Birkhäuser, 2004, ISBN 3-7985-1404-6 , p. 37. Limited preview in the Google book search.
- ↑ a b c Markus Sutera: weak point . In: Der Spiegel . No. 44 , 2019, pp. 131 ( online - October 26, 2019 ).
- ↑ K. Miyasaka et al: The incidence of knee ligament injuries in the general population. In: Am J Knee Surg. 4, 1991, pp. 3-8.
- ↑ S. Rupp, D. Kohn: Front cruciate ligament in the center of interest. In: Orthopedist. 31, 2002, p. 701. doi: 10.1007 / s001320200000 . PMID 12426747 .
- ↑ a b L. Y. Griffin et al. a. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. In: J Am Acad Orthop Surg. 8, 2000, pp. 141-150. PMID 10874221 (Review)
- ↑ a b L. J. Huston et al.: Anterior cruciate ligament injuries in the female athlete. Potential risk factors. In: Clin Orthop Relat Res 372, 2000, pp. 50-63. PMID 10738414 (Review)
- ↑ Federal Statistical Office, Bonn branch, medical expenses calculation: Medical expenses 2002 for the diagnosis M23 (internal damage to the knee joint) in the hospital facility according to gender and age.
- ↑ a b c M. B. Gothner: The influence of the rupture of the anterior cruciate ligament on the RHCL. Dissertation. Ulm University, 2006.
- ^ B. Wagner: Cruciate ligament tear: On shaky knees. In: The star. April 13, 2006.
- ^ E. Arendt, R. Dick: Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. In: Am J Sports Med. 23, 1995, pp. 694-701. PMID 8600737 (Review)
- ^ JW Powell, KD Barber-Foss: Sex-related injury patterns among selected high school sports. In: Am J Sports Med. 28, 2000, pp. 385-391. PMID 10843133
- ↑ a b C. Becker: Biomechanical investigations of different fixation methods for the tibial reinsertion of bony tears of the anterior cruciate ligament. Dissertation. Westfälische Wilhelms-Universität Münster, 2005.
- ↑ TE Hewett et al .: Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. In: Am J Sports Med. 35, 2007, pp. 659-668. PMID 17293469 (Review)
- ^ SD Barber-Westin et al .: Reducing the risk of noncontact anterior cruciate ligament injuries in the female athlete. In: Phys Sportsmed. 37, 2009, pp. 49-61. PMID 20048528 (Review)
- ↑ TE Hewitt: Predisposition to ACL Injuries in Female Athletes Versus Male Athletes. ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice. In: Orthopedics. 31, 2008, pp. 26-28. PMID 18269164
- ↑ a b R. A. Magnussen et al .: Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. In: Knee Surg Sports Traumatol Arthrosc. 18, 2010, pp. 98-105. PMID 19784630
- ↑ a b S. Kesting: Patellar tendon versus semitendinosus / gracilis tendon as replacement for reconstruction of the anterior cruciate ligament - 5-year results of a randomized group of patients - a clinical study. Dissertation, University Hospital Münster, 2008.
- ↑ a b A. Wilcke: Anterior cruciate ligament lesion. Verlag Birkhäuser, 2004, ISBN 3-7985-1404-6 , p. 38. Restricted preview in the Google book search.
- ↑ MH Lam, DT Fong, PS Yung, EP Ho, WY Chan, KM Chan: Knee stability assessment on anterior cruciate ligament injury: Clinical and biomechanical approaches. In: Sports medicine, arthroscopy, rehabilitation, therapy & technology: SMARTT. Volume 1, number 1, 2009, p. 20, doi: 10.1186 / 1758-2555-1-20 . PMID 19712449 , PMC 2744659 (free full text).
- ^ G. Hughes, J. Watkins: A risk-factor model for anterior cruciate ligament injury. In: Sports Med. 36, 2006, pp. 411-428. PMID 16646629 (Review)
- ^ A b E. Alentorn-Geli et al: Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 1: Mechanisms of injury and underlying risk factors. In: Knee Surg Sports Traumatol Arthrosc. 17, 2009, pp. 705-729. PMID 19452139 (Review)
- ↑ M. Waldén, M. Hägglund, J. Ekstrand: High risk of new knee injury in elite footballers with previous anterior cruciate ligament injury. In: British journal of sports medicine. Volume 40, number 2, February 2006, pp. 158-162, doi: 10.1136 / bjsm.2005.021055 . PMID 16432004 , PMC 2492018 (free full text).
- ↑ a b c P. Swärd et al .: Risk factors for a contralateral anterior cruciate ligament injury. In: Knee Surg Sports Traumatol Arthrosc. 18, 2010, pp. 277-291. PMID 20062970 (Review)
- ^ O. Faude et al .: Injuries in female soccer players: a prospective study in the German national league. In: Am J Sports Med. 33, 2005, pp. 1694-1700. PMID 16093546
- ↑ a b J. Orchard et al .: Intrinsic and extrinsic risk factors for anterior cruciate ligament injury in Australian footballers. In: Am J Sports Med. 29, 2001, pp. 196-200. PMID 11292045 .
- ↑ N. Pujol et al .: The incidence of anterior cruciate ligament injuries among competitive Alpine skiers: a 25-year investigation. In: Am J Sports Med. 35, 2007, pp. 1070-1074. PMID 17468379
- ↑ a b L. Salmon et al .: Incidence and risk factors for graft rupture and contralateral rupture after anterior cruciate ligament reconstruction. In: Arthroscopy . 21, 2005, pp. 948-957. PMID 16084292
- ^ O. Faude, A. Junge, W. Kindermann, J. Dvorak: Risk factors for injuries in elite female soccer players. In: British journal of sports medicine. Volume 40, number 9, September 2006, pp. 785-790, doi: 10.1136 / bjsm.2006.027540 . PMID 16825269 , PMC 2564395 (free full text).
- ↑ AM Chaudhari et al .: Anterior cruciate ligament-injured subjects have smaller anterior cruciate ligaments than matched controls: a magnetic resonance imaging study. In: Am J Sports Med. 37, 2009, pp. 1282-1287. PMID 19307330
- ^ EJ Comerford et al.: Distal femoral intercondylar notch dimensions and their relationship to composition and metabolism of the canine anterior cruciate ligament. In: Osteoarthritis Cartilage. 14, 2006, pp. 273-278. PMID 16242971 .
- ^ KD Shelbourne et al .: The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. In: Am J Sports Med. 26, 1998, pp. 402-408. PMID 9617403
- ↑ H. Lund-Hanssen et al.: Intercondylar notch width and the risk for anterior cruciate ligament rupture. A case-control study in 46 female handball players. In: Acta Orthop Scand. 65, 1994, pp. 529-532. PMID 7801756 .
- ↑ JM Uhorchak et al .: Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. In: Am J Sports Med. 31, 2003, pp. 831-842. PMID 14623646
- ↑ TO Souryal, TR Freeman: Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. In: Am J Sports Med. 21, 1993, pp. 535-539. PMID 8368414
- ↑ KD Shelbourne et al .: Radiographic and intraoperative intercondylar notch width measurements in men and women with unilateral and bilateral anterior cruciate ligament tears. In: Knee Surg Sports Traumatol Arthrosc. 5, 1997, pp. 229-233. PMID 9430572
- ↑ S. Lombardo et al .: Intercondylar notch stenosis is not a risk factor for anterior cruciate ligament tears in professional male basketball players: an 11-year prospective study. In: Am J Sports Med. 33, 2005, pp. 29-34. PMID 15610996
- ↑ MS Schickendantz, GG Weiker: The predictive value of radiographs in the evaluation of unilateral and bilateral anterior cruciate ligament injuries. In: Am J Sports Med. 21, 1993, pp. 110-113. PMID 8427350
- ↑ TJ Davis et al .: Correlation of the intercondylar notch width of the femur to the width of the anterior and posterior cruciate ligaments. In: Knee Surg Sports Traumatol Arthrosc. 7, 1999, pp. 209-214. PMID 10462209 .
- ↑ M. Dienst ua: Correlation of intercondylar notch cross sections to the ACL size: a high resolution MR tomographic in vivo analysis. In: Arch Orthop Trauma Surg. 127, 2007, pp. 253-260. PMID 16807752
- ↑ T. Friden et al: Review of knee proprioception and the relation to extremity function after an anterior cruciate ligament rupture. In: J Orthop Sports Phys Ther. 31, 2001, pp. 567-576. PMID 11665744 (Review)
- ^ AC Thomas, RM Palmieri-Smith, SG McLean: Isolated hip and ankle fatigue are unlikely risk factors for anterior cruciate ligament injury. In: Scand J Med Sci Sports. [electronic publication before printing], 2010. PMID 20136750 .
- ↑ SG McLean, JE Samorezov: fatigue induced ACL injury risk stems from a degradation in central control. In: Med Sci Sports Exerc. 41, 2009, pp. 1661-1672. PMID 19568192
- ↑ CB Swanik et al: The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. In: Am J Sports Med. 35, 2007, pp. 943-948. PMID 17369562
- ↑ Julian Mehl, Theresa Diermeier, Elmar Herbst, Andreas B. Imhoff, Thomas Stoffels: Evidence-based concepts for prevention of knee and ACL injuries. 2017 guidelines of the ligament committee of the German Knee Society (DKG) . In: Archives of Orthopedic and Trauma Surgery . tape 138 , no. 1 , January 2018, ISSN 0936-8051 , p. 51-61 , doi : 10.1007 / s00402-017-2809-5 ( springer.com [accessed May 6, 2020]).
- ↑ AV Dowling et al .: Shoe-surface friction influences movement strategies during a sidestep cutting task: implications for anterior cruciate ligament injury risk. In: Am J Sports Med. 38, 2010, pp. 478-485. PMID 9338947
- ^ G. Mykleust et al .: Registration of cruciate ligament injuries in Norwegian top level team handball. A prospective study covering two seasons. In: Scand J Med Sci Sports. 7, 1997, pp. 289-292. PMID 9338947
- ^ JW Orchard, JW Powell: Risk of knee and ankle sprains under various weather conditions in American football. In: Med Sci Sports Exerc. 35, 2003, pp. 1118-1123. PMID 12840631
- ^ J. Orchard et al .: Rainfall, evaporation and the risk of non-contact anterior cruciate ligament injury in the Australian Football League. In: Med J Aust. 170, 1999, pp. 304-306. PMID 10327970
- ↑ JW Orchard, I. Chivers, D. Aldous, K. Bennell, H. Seward: Rye grass is associated with fewer non-contact anterior cruciate ligament injuries than bermuda grass. In: British journal of sports medicine. Volume 39, number 10, October 2005, pp. 704-709, doi: 10.1136 / bjsm.2004.017756 . PMID 16183765 , PMC 1725044 (free full text).
- ↑ J. Löhnert, J. Raunest: Arthroscopic surgery of the knee joint. Scientific publishing company Regensberg & Biermann, 1985, ISBN 3-924469-10-5 .
- ^ A. Wilcke: Anterior cruciate ligament lesion. Verlag Birkhäuser, 2004, ISBN 3-7985-1404-6 , p. 75. Limited preview in the Google book search.
- ↑ P. Segond: Research cliniques et expérimentales sur les épanchements sanguins du genou par entorse. In: Prog Med. 16, 1879, pp. 297-299, 320-321, 340-341, 379-381, 400-401, 419-421.
- ↑ F. Adam: knee. In: D. Kohn (Ed.): Orthopedics and orthopedic surgery. Georg Thieme Verlag, 2005, ISBN 3-13-126231-1 , p. 62. ( limited preview in Google book search)
- ↑ a b C. Elliger-Wimber: Objective scores for replacement of the anterior cruciate ligament with patellar tendon or semitendinosus gracilis tendon. Dissertation. Westphalian Wilhelms University in Münster, 2003.
- ^ KD Shelbourne, T. Gray: Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation. A two- to nine-year followup. In: Am J Sports Med. 25, 1997, pp. 786-795. PMID 9397266
- ^ P. Aglietti et al.: Arthroscopic partial meniscectomy in the anterior cruciate deficient knee. In: Am J Sports Med. 16, 1988, pp. 597-602. PMID 3071151 (Review)
- ↑ VJ Cooley et al .: Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. In: Arthroscopy. 17, 2001, pp. 795-800. PMID 11600975
- ↑ F. Escalas et al .: T-Fix anchor sutures for arthroscopic meniscal repair. In: Knee Surg Sports Traumatol Arthrosc. 5, 1997, pp. 72-76. PMID 9228311 .
- ^ WD Cannon, JM Vittori: The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. In: Am J Sports Med. 20, 1992, pp. 176-181. PMID 1558246
- ^ FR Noyes, SD Barber-Westin: Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. In: Arthroscopy. 16, 2000, pp. 822-829. PMID 11078538
- ↑ Steven Claes, Stijn Bartholomeeusen, Johan Bellemans: High prevalence of anterolateral Ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. In: Acta Orthopædica Belgica. 2014, Volume 80, Issue 1, March 2014, pp. 45–49.
- ↑ RH Brophy et al .: Anterior cruciate ligament reconstruction and concomitant articular cartilage injury: incidence and treatment. In: Arthroscopy. 26, 2010, pp. 112-120. PMID 20117635
- ↑ N. Hartnett, RJ Tregonning: Delay in diagnosis of anterior cruciate ligament injury in sport. In: NZ Med J. 114, 2001, pp. 11-13. PMID 11243663
- ^ A b S. R. Bollen, BW Scott: Anterior cruciate ligament rupture: a quiet epidemic? In: Injury. 27, 1996, pp. 407-409. PMID 8881137 .
- ↑ FR Noyes et al. a .: Knee sprains and acute knee hemarthrosis: misdiagnosis of anterior cruciate ligament tears. In: Phys Ther. 60, 1980, pp. 1596-1601. PMID 7454786
- ^ KD Shelbourne, DA Foulk: Treatment of anterior cruciate ligament injuries. Principles and practice of orthopedic sport medicine. WE Garrett et al. a. (Editors), Lippincott Williams & Wilkins, Philadelphia, 2000, ISBN 0-7817-2578-X , pp. 743-761.
- ↑ SJ Kim, HK Kim: Reliability of the anterior drawer test, the pivot shift test and the Lachman test. In: Clin Orthop Relat Res. 317, 1995, pp. 237-242. PMID
- ^ DP König et al .: Diagnosis of anterior knee instability. Comparison between the Lachman test, the KT-1000 arthrometer and the ultrasound Lachman test. In: trauma surgeon. 101, 1998, pp. 209-213. PMID 9577218
- ^ W. Schwarz et al.: Manual ultrasound of the knee joint. A general practice method for diagnosis of fresh rupture of the anterior cruciate ligament. In: trauma surgeon. 100, 1997, pp. 280-285. PMID 9229778
- ^ KJ O'Shea et al .: The Diagnostic Accuracy of History, Physical Examination, and Radiographs in the Evaluation of Traumatic Knee Disorders. In: Am J Sports Med. 24, 1996, pp. 164-167. PMID 8775114
- ↑ HJ Gelb et al .: Magnetic resonance imaging of knee disorders: clinical value and cost effectiveness in a sports medicine practice. In: Am J Sports Med. 24, 1996, pp. 99-103. PMID 8638763
- ^ F. Rayan: Clinical, MRI, and arthroscopic correlation in meniscal and anterior cruciate ligament injuries. In: Int Orthop. 33, 2009, pp. 129-132. PMID 18297284
- ^ Y. Kocabey et al .: The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. In: Arthroscopy. 10, 2004, pp. 696-700. PMID 15346110
- ↑ S. Thomas et al: The value of magnetic resonance imaging in our current management of ACL and meniscal injuries. In: Knee Surg Sports Traumatol Arthrosc. 15, 2007, pp. 533-536. PMID 17225179
- ↑ a b R. Crawford et al. a .: Magnetic resonance imaging versus arthroscopy in the diagnosis of knee pathology, concentrating on meniscal lesions and ACL tears: a systematic review. In: Br Med Bull. 84, 2007, pp. 5-23. PMID 17785279 (Review)
- ^ N. Glynn et al .: Trends in utilization: has extremity MR imaging replaced diagnostic arthroscopy? In: Skelet Radiol. 33, 2004, pp. 272-276. doi: 10.1007 / s00256-004-0750-5 .
- ↑ K. Wörtler: MRI of the knee joint. In: The Radiologist. 47, 2007, pp. 1131-1143. doi: 10.1007 / s00117-007-1581-x . PMID 17992501 .
- ↑ a b G. S. Perrone, BL Proffen et al: Bench-to-Bedside: Bridge-Enhanced Anterior Cruciate Ligament Repair. In: J Orthop Res. 13 Jun 2017. PMID 28608618 , doi: 10.1002 / jor.23632 .
- ↑ a b D. T. Nguyen, TH Ramwadhdoebe et al: Intrinsic healing response of the human anterior cruciate ligament: an histological study of reattached ACL remnants. In: J Orthop Res. 32 (2), Feb 2014, pp. 296-301. PMID 24600702 .
- ↑ M. Costa-Paz, MA Ayerza et al: Spontaneous Healing in Complete ACL Ruptures: A Clinical and MRI Study. In: Clin Orthop Relat Res. 470 (4), Apr 2012, pp. 979-985. PMID 21643922 , doi: 10.1007 / s11999-011-1933-8 .
- ↑ E. Fujimoto, Y. Sumen et al .: Spontaneous healing of acute anterior cruciate ligament (ACL) injuries — conservative treatment using an extension block soft brace without anterior stabilization. In: Arch Orthop Trauma Surg. 122 (4), May 2002, pp. 212-216. PMID 12029510 , doi: 10.1007 / s00402-001-0387-y .
- ^ FH Fu, S. Cohen: Current Concepts in ACL Reconstruction. 1st edition. Slack Incorporated, 03/2008, p. 107, Online ISBN 978-1-55642-813-5 .
- ^ A b Wolf Petersen, Thore Zantop: The anterior cruciate ligament: Fundamentals and current practice of operative therapy; with 29 tables . Deutscher Ärzteverlag, Cologne 2009, ISBN 978-3-7691-0562-9 , p. 41 (250 p., Limited preview in Google Book search).
- ^ GA Murell et al.: The effects of time course after anterior cruciate ligament injury in correlation with meniscal and cartilage loss. In: Am J Sports Med. 29, 2001, pp. 9-14. PMID 11206263
- ^ H. Ross et al .: Osteoarthritis of the knee after injury to the anterior cruciate ligament and meniscus: the influence of time and age. In: Osteoarthritis Cartil. 3, 1995, pp. 261-267. PMID 8689461
- ↑ C. Fink et al.: Long-term results after conservative or surgical treatment of the anterior cruciate ligament rupture. In: The trauma surgeon. 99, 1996, pp. 964-969. doi: 10.1007 / s001130050081 .
- ^ A b P. P. Casteleyn, F. Handelberg: Non-operative management of the anterior cruciate ligament injuries in the general population. ( Memento of the original from January 9, 2009 in the Internet Archive ) Info: The archive link was automatically inserted and not yet checked. Please check the original and archive link according to the instructions and then remove this notice. In: Bone It Surg. 78, 1996, pp. 446-451. PMID 8636184
- ↑ a b c C. B. Frank and DW Jackson: The science of reconstruction of the anterior cruciate ligament. In: J Bone Joint Surg Am. 79, 1997, pp. 1556-1576. PMID 9378743 (Review)
- ^ R. Johnson et al: The treatment of injuries of the anterior cruciate ligament. In: J Bone Joint Surg. 74, 1992, pp. 140-151. PMID 1734005 (Review)
- ↑ F. Noyes et al: The variable functional disability of the anterior cruciate ligament-deficient knee. In: Orthop Clin N Am. 16, 1985, pp. 47-67. PMID 3881716 (Review)
- ↑ C. Andersson et al.: Knee function after surgical and nonsurgical treatment of acute rupture of the anterior cruciate ligament: A randomized study with a long-term follow-up period. In: Clin Orthop. 264, 1991, pp. 255-263. PMID 1997243
- ^ W. Clancy et al.: Acute tears of the anterior cruciate ligament. Surgical versus conservative treatment. In: J Bone Joint Surg. 70, 1988, pp. 1483-1488. PMID 3198673
- ↑ P. Neyret et al .: Partial meniscectomy and anterior cruciate ligament rupture in soccer players. A study with a minimum 20-year followup. In: Am J Sports Med. 21, 1993, pp. 455-460. PMID 8346763
- ^ H. Roos et al .: Soccer after anterior cruciate ligament injury - an incompatible combination? A national survey of incidence and risk factors and a 7-year follow-up of 310 players. In: Acta Orthop Scand. 66, 1995, pp. 107-112. PMID 7740937
- ↑ L. Rosenberg, M. Sherman: Meniscal injury in the anterior cruciate-deficient knee. A rational for clinical decision-making. In: Sports Med. 13, 1992, pp. 423-432. PMID 1615259
- ↑ M. Herbort, C. Fink: Tear of the anterior cruciate ligament. Biomechanical effects on the knee joint. In: Arthroscopy (2015) 28: 18 link.springer.com doi: 10.1007 / s00142-014-0833-9 .
- ↑ JP Zlotnicki, JH Naendrup et al .: Basic biomechanic principles of knee instability. Curr Rev Musculoskelet Med. 9 (2), Jun 2016, pp. 114-22. PMID 27007474 , doi: 10.1007 / s12178-016-9329-8 .
- ↑ a b c G. Gremion et al.: Conservative treatment of an anterior cruciate ligament tear - results. In: Orthopedic technology. 1, 2002, pp. 99-101.
- ^ WJ McDaniel, TB Dameron: The untreated anterior cruciate ligament rupture. In: Clin Orthop Relat Res. 172, 1983, pp. 158-163. PMID 6821986 .
- ↑ BD Beynnon et al.: Treatment of anterior cruciate ligament injuries, part I. In: Am J Sports Med. 33, 2005, pp. 1579-1602. PMID 16199611 (Review)
- ↑ BD Beynnon include: Treatment of anterior cruciate ligament injuries, part II. In: Am J Sports Med. 33, 2005, pp 1751-1761. PMID 16230470 (Review)
- ↑ S. Hinterwimmer et al: Operative vs. Conservative therapy of anterior cruciate ligament rupture: a systematic review of the literature. In: The trauma surgeon. 106, 2003, pp. 374-379. doi: 10.1007 / s00113-003-0596-7 (Review)
- ^ RH Wittenberg et al.: A comparison of conservative and delayed surgical treatment of anterior cruciate ligament ruptures. A matched pair analysis. In: Int Orthop. 22, 1998, pp. 145-148. PMID 9728304
- ↑ H. Seitz et al.: Long-term results after anterior cruciate ligament replacement compared to conservative therapy. In: surgeon. 65, 1994, pp. 992-998. PMID 7821082 .
- ↑ C. Andersson et al.: Knee function after surgical or nonsurgical treatment of acute rupture of the anterior cruciate ligament: a randomized study with a long-term follow-up period. In: Clin Orthop Relat Res. 264, 1991, pp. 255-263. PMID 1997243
- ↑ E. Linko et al .: Surgical versus conservative interventions for anterior cruciate ligament ruptures in adults. In: Cochrane Database Syst Rev. 2005, CD001356. PMID 15846618
- ↑ a b c d e M. Schettle: Comparison of the anterior cruciate ligament plasty by the middle third of the patellar tendon allograft with the middle third of the patellar tendon autograft in revision surgery. Dissertation. LMU Munich, 2008.
- ↑ C. Fink et al .: Long-term outcome of operative or nonoperative treatment of anterior cruciate ligament rupture - is sports activity a determining variable? In: Int J Sports Med. 22, 2001, pp. 304-309. PMID 11414676
- ^ PJ Fowler, WD Regan: The patient with symptomatic chronic anterior cruciate ligament insufficiency. In: Am J Sports Med. 15, 1987, pp. 321-325. PMID 3661812 .
- ^ TP Giove et al.: Non-operative treatment of the torn anterior cruciate ligament. In: J Bone Jt Surg. 65, 1985, pp. 184-192. PMID 6822581 .
- ^ A b R. J. Hawkins et al .: Follow up of the acute nonoperated isolated anterior cruciate ligament tear. In: Am J Sports Med. 14, 1986, pp. 205-210. PMID 3752360 .
- ↑ RB Frobell, HP Roos, Roos EM, FW Roemer, F. Ranstam, LS Lohmander: Treatment for acute anterior cruciate ligament tear: five year outcome of randomized trial. In: BMJ. 2013; 346, doi: 10.1136 / bmj.f232 .
- ↑ DJ Beard et al. a .: Proprioception enhancement for anterior cruciate deficiency. A prospective trial of two physiotherapy regimes. ( Memento of the original from January 8, 2009 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. In: Bone Surg. 76, 1994, pp. 654-659. PMID 8027158
- ↑ H. Ihara, A. Nakayama: Dynamic joint control training for knee ligament injuries. In: Am J Sports Med. 14, 1986, pp. 309-315. PMID 3728783
- ↑ P. Kannus, M. Jarvinen: conservatively Treated tears of the anterior cruciate ligament. In: J Bone Joint Surg Am. 69, 1987, pp. 1007-1012. PMID 3654691
- ^ R. Sandberg et al .: Operative vervus non-operative treatment of recent injuries. A prospective randomized study. In: J Bone Jt Surg. 69, 1987, pp. 1120-1126. PMID 3312204 .
- ^ MJ Blyth et al .: Anterior cruciate ligament reconstruction in patients over the age of 50 years: 2- to 8-year follow-up. In: Knee Surg Sports Traumatol Arthrosc. 11, 2003, pp. 204-211. PMID 12761610 .
- ↑ NK Paschos, SM Howell: treatment principles of: Anterior cruciate ligament reconstruction. EFORT Open Rev. 1 (11), Mar 13, 2017, pp. 398–408. PMID 28461919 , doi: 10.1302 / 2058-5241.1.160032 .
- ↑ a b F. Dirisamer: Patient information: Diagnostic Kreuzbandriß. (PDF) Retrieved February 4, 2010.
- ↑ LP Granån, M. Forssblad, M. Lind, L. Engebretsen: The Scandinavian ACL registries 2004-2007: baseline epidemiology. In: Acta orthopedica. Volume 80, Number 5, October 2009, pp. 563-567, doi: 10.3109 / 17453670903350107 . PMID 19916690 , PMC 2823321 (free full text).
- ↑ J. Kennedy et al .: Timing of reconstruction of the anterior cruciate ligament in athletes and the incidence of secondary pathology within the knee. In: J Bone Joint Surg Br. 92, 2010, pp. 362-366. PMID 20190306
- ↑ JC Yoo et al .: Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. In: Am J Sports Med. 37, 2009, pp. 1478-1483. PMID 19359417
- ↑ PJ Millett et al .: Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? In: Arthroscopy. 18, 2002, pp. 955-959. PMID 12426537 (Review)
- ^ DA Novikov, SJ Swensen et al.: The effect of smoking on ACL reconstruction: a systematic review. Phys Sportsmed. 44 (4), Nov 2016, pp. 335-341. PMID 27456300 , doi: 10.1080 / 00913847.2016.1216239 .
- ^ Pieter-Jan Verhelst, Thomas Luyckx: Surgical Treatment of the anterior curciate ligament rupture: where do we stand today? Acta Belgica Orthopædica 218, Volume 83, Issue 2, pp. 268-275.
- ↑ M. Krüger-Franke et al: Arthroscopic anterior cruciate ligament reconstruction - what is certain in 2009? In: Sports Orthopedics - Sports Traumatology. 25, 2009, pp. 206-211. doi: 10.1016 / j.orthtr.2009.06.002 .
- ↑ M. Schuhmacher: Changes in selected parameters of the knee joint mechanics before and after surgical replacement of the anterior cruciate ligament with different surgical techniques. ( Memento from September 3, 2014 in the Internet Archive ) (PDF; 9.7 MB) Dissertation, German Sport University Cologne, 2007.
- ↑ M. Quante, E. Hille: Proprioception: A critical analysis of the value in sports medicine. (PDF). In: Dtsch Z Sportmed. 50, 1999, pp. 306-310.
- ↑ a b c d e f g h i j k l m A. Weiler: Anatomical "hamstring tendons" anchoring with interference screws for cruciate ligament replacement. (PDF; 812 kB) Habilitation thesis. Humboldt University of Berlin, 2002.
- ↑ a b J. Höher, T. Tiling: Differentiated selection of grafts in cruciate ligament surgery. In: surgeon. 71, 2000, pp. 1045-1054. doi: 10.1007 / s001040051180 . PMID 11043122 .
- ↑ J. Brand et al .: Current concepts: Graft fixation in cruciate ligament surgery. In: Am J Sports Med. 28, 2000, pp. 761-774. PMID 11032238 (Review)
- ^ Guidelines of the German Society for Trauma Surgery: Anterior cruciate ligament rupture. Last update: 5/2008.
- ↑ TR Duquin include: Current trends in anterior cruciate ligament reconstruction. In: J Knee Surg. 22, 2009, pp. 7-12. PMID 19216345
- ↑ T. Gifstad, OA Foss et al .: Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. In: Am J Sports Med. 42 (10), Oct 2014, pp. 2319-2328. PMID 25201444 , doi: 10.1177 / 0363546514548164 .
- ↑ D. Andernord, H. Björnsson et al .: Surgical Predictors of Early Revision Surgery After Anterior Cruciate Ligament Reconstruction: Results From the Swedish National Knee Ligament Register on 13,102 Patients. In: Am J Sports Med. 42 (7), Jul 2014, pp. 1574–1582. PMID 24778266 , doi: 10.1177 / 0363546514531396 .
- ^ W. Franz, J. Ulbrich: A new technique for removing the semitendinosus tendon for cruciate ligament replacement. In: Arthroscopy. 17, 2004, pp. 104-107. doi: 10.1007 / s00142-004-0255-1 .
- ^ H. Steckel et al .: The double-bundle technique for anterior cruciate ligament reconstruction: a systematic overview. In: Scand J Med Sci Sports. 17, 2007, pp. 99-108. PMID 17076829 (Review)
- ↑ C. Chen et al .: Arthroscopic anterior cruciate ligament reconstruction with quadriceps tendon-patellar bone autograft. In: J trauma. 46, p. 1999, p. 678-682. PMID 10217233
- ↑ P. Reich: Patellar tendon third autograft versus allograft when replacing the anterior cruciate ligament. Dissertation, Ludwig Maximilians University Munich, 2007.
- ↑ D. Drez et al .: Anterior cruciate ligament reconstruction using bone-patellar tendon-bone allografts. A biological and biomechanical evaluation in goats. In: Am J Sports Med. 19, 1991, pp. 256-263. PMID 1714244
- ↑ BM Fideler et al .: Gamma irradiation: effect on biomechanical properties of human bone-patellar tendon-bone allografts. In: Am J Sports Med. 23, 1995, pp. 643-646. PMID 8526284
- ↑ D. Jackson et al .: Intraarticular reactions associated with the use of freeze-dried, ethylene oxide-sterilized bone-patellar tendon-bone allografts in the reconstruction of the anterior cruciate ligament. In: Am J Sports Med. 18, 1990, pp. 1-11. PMID
- ↑ TS Roberts et al .: Anterior cruciate ligament reconstruction using freeze-dried, ethylene oxide-sterilized bone-patellar tendon-bone allografts. In: Am J Sports Med. 19, 1991, pp. 35-41. PMID 2301680 .
- ↑ D. Jackson et al .: A comparison of patellar tendon autograft and allograft used for anterior cruciate ligament reconstruction in the goat model. In: Am J Sports Med. 21, 1993, pp. 176-185. PMID
- ↑ P. Nikolaou et al .: Anterior cruciate ligament allograft transplantation: Long-term function, histology, revsacularization and operative technique. In: Am J Sports Med. 14, 1986, pp. 348-360. PMID
- ^ JL Carey et al: A systematic review of anterior cruciate ligament reconstruction with autograft compared with allograft. In: J Bone Joint Surg Am. 91, 2009, pp. 2242-2250. PMID 19724004 (Review)
- ↑ KF Almqvist et al: A long-term study of anterior cruciate ligament allograft reconstruction. In: Knee Surg Sports Traumatol Arthrosc. 17, 2009, pp. 818-822. PMID 19421736 .
- ↑ K. Sun et al .: Anterior cruciate ligament reconstruction with bone-patellar tendon-bone autograft versus allograft. In: Arthroscopy. 25, 2009, pp. 750-759.
- ^ DA McGuire, SD Hendricks: Allograft tissue in ACL reconstruction. In: Sports Med Arthrosc. 17, 2009, pp. 224-233. PMID 19910780 (Review)
- ↑ F. Fu et al .: Graft selection for anterior cruciate ligament reconstruction. In: Instr Course Lect. 58, 2009, pp. 337-354. PMID 19385547
- ↑ K. Kumar, N. Maffulli: The ligament augmentation device: an historical perspective. In: Arthroscopy. 15, 1999, pp. 422-432. PMID 10355719 (Review)
- ^ LE Paulos et al: The GORE-TEX anterior cruciate ligament prosthesis. A long-term followup. In: Am J Sports Med. 20, 1992, pp. 246-252. PMID 1636852
- ^ L. Claes et al .: Biological response to ligament wear particles. In: J Appl Biomater. 6, 1995, pp. 35-41. PMID 7703536
- ↑ a b K. Jenson, W. Klein: Problems and complications in artificial cruciate ligament replacement. In: Arthroscopy. 3, 1990, pp. 15-23.
- ↑ W. Klein, K. Jenson: Synovitis and artificial ligaments. In: Arthroscopy. 8, 1992, pp. 116-124. PMID 1532312 .
- ↑ D. Stengel et al. a .: Resorbable screws versus pins for optimal transplant fixation (SPOT) in anterior cruciate ligament replacement with autologous hamstring grafts: rationale and design of a randomized, controlled, patient and investigator blinded trial (ISRCTN17384369). In: BMC Surgery. 5, 2005, 1st doi: 10.1186 / 1471-2482-5-1 . PMID 15723704 ( Open Access ).
- ↑ S. Fromm: Reconstruction of the anterior cruciate ligament (ACL) with a bone-tendon-bone transplant using the ENDOBUTTON CL BTB fixation system. Smith & Nephew GmbH brochure
- ^ S. Konan, FS Haddad: A clinical review of bioabsorbable interference screws and their adverse effects in anterior cruciate ligament reconstruction surgery. In: The Knee. 16, 2009, pp. 6-13. PMID 18639461 (Review)
- ↑ a b H. H. Paessler, DS Mastrokalos: Anterior cruciate ligament reconstruction using semitendinosus and gracilis tendons, bone patellar tendon, or quadriceps tendon-graft with press-fit fixation without hardware. A new and innovative procedure. In: Orthop Clin North Am. 34, 2003, pp. 49-64. PMID 12735201 (Review)
- ^ NP Südkamp, NP Haas: New ways in cruciate ligament surgery. In: The surgeon. 71, 2000, pp. 1024-1033. doi: 10.1007 / s001040051178 . PMID 11043120 .
- ↑ P. Aglietti et al .: Patellofemoral problems after intraarticular anterior cruciate ligament reconstruction. In: Clin Orthop. 288, 1993, pp. 195-204. PMID 8458134
- ↑ L. Paulos et al: Infrapatellar contracture syndrom: An unrecognized cause of knee stiffness with patella entrapment and patella infera. In: Am J Sports Med. 15, 1987, pp. 331-341. PMID 3661814 .
- ↑ J. Kartus et al. a. Complications following arthroscopic anterior cruciate ligament reconstruction. A 2-5 year follow-up of 604 patients with special emphasis on anterior knee pain. In: Knee Surg Sports Traumatol Arthrosc. 7, 1999, pp. 2-8. PMID 10024955
- ↑ a b J. Rosenberg et al .: Extensor mechanism function after patellar tendon graft harvest for anterior cruciate ligament reconstruction. In: Am J Sports Med. 18, 1990, pp. 560-565. PMID 1443318
- ↑ R. Bartlett et al. a .: Graft selection in reconstruction of the anterior cruciate ligament. ( Page no longer available , search in web archives ) Info: The link was automatically marked as defective. Please check the link according to the instructions and then remove this notice. In: J Bone Joint Surg. 83, 2001, pp. 625-634. PMID 11476294
- ^ A b I. Corry et al.: Arthroscopic reconstruction of the anterior cruciate ligament: A comparison of patellar tendon autograft and four-strand hamstring tendon autograft. In: Am J Sports Med. 27, 1999, pp. 444-454. PMID 10424213
- ↑ J. Kartus include: Factors Affecting donor-site morbidity after anterior cruciate ligament reconstruction using bone-patellar tendon-bone grafts car. In: Knee Surg Sports Traumatol Arthrosc. 5, 1997, pp. 222-228. PMID 9430571
- ↑ T. Muellner et al .: Shortening of the patella tendon after anterior cruciate ligament reconstruction. In: Arthroscopy. 14, 1998, pp. 444-454. PMID 9754477
- ↑ B. Shaffer, J. Tibone: patellar tendon length change after anterior cruciate ligament reconstruction using patellar tendon the midthird. In: Am J Sports Med. 21, 1993, pp. 633-646. PMID 8346762
- ↑ T. Järvelä et al .: The incidence of patellofemoral osteoarthritis and associated findings 7 years after anterior cruciate ligament reconstruction with a bone-patellar tendon-bone autograft. In: Am J Sports Med. 29, 2001, pp. 18-24. PMID 11206250
- ↑ a b J. Feller et al .: Early post-operative morbidity following anterior cruciate ligament reconstruction: patellar tendon versus hamstring graft. In: Knee Surg Sports Traumatol Arthrosc. 9, 2001, pp. 260-266. PMID 11685356
- ↑ A. Lipscomb et al .: Evaluation of hamstring strength following use of semitendinosus and gracilis tendons to reconstruct the anterior cruciate ligament. In: Am J Sports Med. 10, 1982, pp. 340-342. PMID 7180953
- ↑ a b K. Yasuda et al .: Graft site morbidity with autogenous semitendinosus and gracilis tendons. In: Am J Sports Med. 23, 1995, pp. 706-714. PMID 8600739
- ↑ Y. Hsieh et al .: The effects of removal and reconstruction of the anterior cruciate ligament on patellofemoral kinematics. In: Am J Sports Med. 26, 1998, pp. 201-209. PMID 9548113
- ↑ R. Viola et al .: Internal and external tibial rotation strength after anterior cruciate ligament reconstruction using ipsilateral semidentinosus and gracilis tendon autograft. In: Am J Sports Med. 28, 2000, pp. 552-555. PMID 10921649 .
- ↑ K. Eriksson et al: The semitendinosus tendon regenerates after resection: a morphologic and MRI analysis in 6 patients after resection for anterior crucaite ligament reconstruction. In: Acta Orthop Scand. 72, 2001, pp. 379-384. PMID 11580127
- ↑ K. Eriksson et al: Semitendinosus tendon regeneration after harvesting for ACL reconstruction. A prospective MRI study. In: Knee Surg Sports Traumatol Arthrosc. 7, 1999, pp. 220-225. PMID 10462211 .
- ↑ P. Papandrea et al .: Regeneration of the semitendinosus tendon harvested for anterior cruciate ligament reconstruction. Evaluation using ultrasonography. In: Am J Sports Med. 28, 2000, pp. 556-561. PMID 10921650 .
- ↑ DM Rispoldi et al .: Magnetic resonance imaging at different time periods following hamstring harvest for anterior cruciate ligament reconstruction. In: Arthroscopy. 17, 2001, pp. 2-8. PMID 11154359
- ↑ P. Simonian et al .: Assessment of morbidity of semitendinosus and gracilis tendon harvest for ACL reconstruction. In: Am J Knee Surg. 10, 1997, pp. 54-59. PMID 9131234 .
- ↑ A. Comley, J. Krishnan: Donor site morbidity after quadriceps tendon harvest for rotator cuff repair. In: Aust NZJ Surg. 69, 1999, pp. 808-810. PMID 10553971
- ↑ a b R. Becker et al.: The anterior cruciate ligament plasty - choice of graft and anchoring techniques. In: Zentralbl Chir. 127, 2002, pp. 842-849. doi: 10.1055 / s-2002-35128 . PMID 12410449 .
- ^ W. Konermann, R. Haaker: Navigation and Robotic in Joint and Spine Surgery. Verlag Springer, 2002, ISBN 3-540-43305-8 restricted preview in the Google book search.
- ↑ T. Frietsch, A. Weiler-Lorentz (Ed.): Anesthesia in traumatology and orthopedics. Verlag Elsevier, Urban & Fischer, 2009, ISBN 978-3-437-24450-6 , p. 44. Restricted preview in the Google book search.
- ↑ P. Lobenhoffer, JD Agneskirchner: Anterior cruciate ligament - what is secured? In: Arthroscopy. 18, 2005, pp. 11-14. doi: 10.1007 / s00142-004-0290-y .
- ^ J. Wang, Y. Ao: Analysis of different kinds of cyclops lesions with or without extension loss. In: Arthroscopy. 25, 2009, pp. 626-631. PMID 19501293 .
- ↑ CD Harner et al.: Loss of motion after anterior cruciate ligament reconstruction. In: Am J Sports Med. 20, 1992, pp. 499-506. PMID 1443315
- ↑ JM Marzo et al .: Intraarticular fibrous nodule as a cause of loss of extension following anterior cruciate ligament reconstruction. In: Arthroscopy. 8, 1992, pp. 10-18. PMID 1550639
- ↑ KE DeHaven et al.: Arthrofibrosis of the knee following ligament surgery. In: Instr Course Lect. 52, 2003, pp. 369-381. PMID 12690864 (Review)
- ↑ a b T. Weig: Restriction of movement after anterior cruciate ligament reconstruction (analysis of causes, therapy results). Dissertation, LMU Munich, 2002.
- ↑ a b M. Fagelman, KB Freedman: Revision reconstruction of the anterior cruciate ligament: evaluation and management. In: Am J Orthop. 34, 2005, pp. 319-328. PMID 16130349 (Review)
- ^ EW Carson et al .: Revision anterior cruciate ligament reconstruction: etiology of failures and clinical results. In: J Knee Surg. 17, 2004, pp. 127-132. PMID 15366266
- ↑ RT Burks et al .: Treatment of postoperative anterior cruciate ligament infections with graft removal and early reimplantation. In: Am J Sports Med. 31, 2003, pp. 414-418. PMID 12750136
- ^ SY Fong, JL Tan: Septic arthritis after arthroscopic anterior cruciate ligament reconstruction. (PDF; 41 kB). In: Ann Acad Med Singap. 33, 2004, pp. 228-234. PMID 15098639
- ↑ PF Indelli include: Septic arthritis in postoperative anterior cruciate ligament reconstruction. In: Clin Orthop Rel Res. 398, 2002, pp. 182-188. PMID 11964649
- ^ DR McAllister et al .: Outcomes of postoperative septic arthritis after anterior cruciate ligament reconstruction. In: Am J Sports Med. 27, 1999, pp. 562-570. PMID 10496570
- ^ R. Viola et al .: An unusual epidemic of Staphylococcus-negative infections involving anterior cruciate ligament reconstruction with salvage of the graft and function. In: Arthroscopy. 16, 2000, pp. 173-177. PMID 10705329
- ^ RJ Williams et al.: Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: diagnosis and management. In: Am J Sports Med. 25, 1997, pp. 261-267. PMID 9079185
- ↑ C. Wang et al .: Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, presentation, treatment, and cause. In: Arthroscopy. 25, 2009, pp. 243-249. PMID 19245985
- ↑ G. Mouzopoulos et al .: Septic knee arthritis following ACL reconstruction: a systematic review. In: Knee Surg Sports Traumatol Arthrosc. 17, 2009, pp. 1033-1042. PMID 19381611 (Review)
- ↑ LM Katz et al.: A retrospective comparison of the incidence of bacterial infection following anterior cruciate ligament reconstruction with autograft versus allograft. In: Arthroscopy. 24, 2008, pp. 1330-1335. PMID 19038702
- ^ D. Judd et al .: Infections following arthroscopic anterior cruciate ligament reconstruction. In: Arthroscopy. 22, 2006, pp. 375-384. PMID 16581449 .
- ↑ R. Müller-Rath, E. Ingenhoven, T. Mumme, M. Schumacher, O. Miltner: Perioperative management in outpatient arthroscopy of the knee joint. In: Z Orthop accident. 148, 2010, pp. 282-287. PMID 20135619 .
- ↑ T. Efe et al. a .: Malignant fibrous histiocytoma of the distal femur after an arthroscopic anterior cruciate ligament reconstruction: A case report and a review of the literature. (PDF; 843 kB). In: BMC Cancer. 10, 2010, 264, doi: 10.1186 / 1471-2407-10-264 ( Open Access ).
- ↑ F. Sirveaux include: pleomorphic malignant fibrous histiocytoma at the site of an arthroscopic reconstruction of the anterior cruciate ligament. A case report. In: J Bone Joint Surg Am. 87, 2005, pp. 404-409. PMID 15687167
- ^ JJ Caron et al .: Leiomyosarcoma of the distal femur after anterior cruciate ligament reconstruction. In: Clin Orthop Relat Res. 419, 2004, pp. 214-217. PMID 15021157 .
- ↑ a b J. Feagin, W. Curl: Isolated tear of the anterior cruciate ligament. 5-year follow-up study. In: Am J Sports Med. 4, 1976, pp 95-100. PMID 984289
- ↑ JL Marshall, RF Warren et al .: Primary surgical treatment of anterior cruciate ligament lesions. In: Am J Sports Med. 10 (2), Mar-Apr 1982, pp. 103-7. PMID 7081522 , doi: 10.1177 / 036354658201000208 .
- ↑ L. Engebretsen, P. Benum, S. Sundalsvoll: Primary suture of the anterior cruciate ligament. A 6-year follow-up of 74 cases. In: Acta Orthop Scand. 60 (5), Oct 1989, pp. 561-4. PMID 2603656
- ↑ a b N. Kaplan, T. Wickiewicz et al .: Primary surgical treatment of anterior cruciate ligament ruptures. A long-term follow-up study. In: Am J Sports Med. 1990 Jul-Aug; 18 (4): 354-8. PMID 2206080 , doi: 10.1177 / 036354659001800404 .
- ^ MF Sherman, L. Lieber et al.: The long-term followup of primary anterior cruciate ligament repair. Defining a rational for augmentation. In: Am J Sports Med. 19 (3), May-Jun 1991, pp. 243-55. PMID 1867333 , doi: 10.1177 / 036354659101900307 .
- ↑ F. Genelin, A. Trost et al .: Late results following proximal reinsertion of isolated ruptured ACL ligaments. Knee Surg Sports Traumatol Arthrosc. 1 (1), 1993, pp. 17-9. PMID 8535991 .
- ↑ a b c d e H. H. Pässler, A. Driessen: The history of cruciate ligament surgery. In: ATOSNews. 11, 2008, pp. 50-61.
- ↑ M. Odensten et al: Suture of fresh ruptures of anterior cruciate ligament. A 5-year follow-up. In: Acta Orthop Scand. 55, 1984, pp. 270-272. PMID 6377805
- ↑ K. Sommerlath et al .: The long-term course after treatment of acute anterior cruciate ligament ruptures. A 9-to 16-year follow-up. In: Am J Sports Med. 19, 1991, pp. 156-162. PMID 2039067 .
- ↑ a b c C. Eberhardt among others: History of surgery of the anterior cruciate ligament. In: Orthopedist. 31, 2002, pp. 702-709, doi: 10.1007 / s00132-002-0329-6 .
- ↑ a b C. Fink u. a .: Long-term results after conservative or surgical treatment of anterior cruciate ligament rupture. In: trauma surgeon. 99, 1996, pp. 964-969, doi: 10.1007 / s001130050081 .
- ↑ a b T. Grøntvedt et al: A prospective randomized study of three operations for acute rupture of the anterior cruciate ligament. Five-year follow-up of one hundred and thirty-one patients. In: J Bone Joint Surg Am. 78, 1996, pp. 159-168. PMID 8609105 .
- ↑ a b P. Hertel: Fresh and old knee ligament injuries. In: trauma surgeon. 99, 1996, ISSN 0177-5537 , pp. 686-700.
- ↑ a b H. Seiler, HR Frank: Suture on the anterior cruciate ligament - what is the method really worth? In: trauma surgeon. 96, 1993, pp. 443-450. PMID 8235679 .
- ↑ T. Strand et al .: Long-term follow-up after primary repair of the anterior cruciate ligament: clinical and radiological evaluation 15-23 years postoperatively. In: Arch Orthop Trauma Surg. 125, 2005, pp. 217-221. PMID 15875231
- ↑ HH Paessler, J. Deneke et al .: Augmented repair and early mobilization of acute anterior cruciate ligament injuries. In: Am J Sports Med. 20 (6), Nov-Dec 1992, pp. 667-74. PMID 1456360 journals.sagepub.com doi: 10.1177 / 036354659202000607 .
- ↑ T. Gomez et al .: Semitendinosus repair augmentation of acute anterior cruciate ligament rupture. In: Can J Sports Sci. 15, 1990, pp. 137-142. PMID 2383818
- ↑ G. Hehl et al .: Clinical experience with PDS II augmentation for operative treatment of acute proximal ACL reptures - 2-year follow-up. In: Knee Surg Sports Traumatol Arthrosc. 7, 1999, pp. 102-106. PMID 10223532
- ↑ W. Holzmüller et al.: Mechanical properties of PDS-augmented patellar tendon transplants for. Reconstruction of the anterior cruciate ligament. In: trauma surgeon. 95, 1992, pp. 306-310. PMID 1636112
- ↑ W. Holzmüller et al .: Histological examinations for the replacement of the anterior cruciate ligament with PDS-augmented patellar tendon grafts. In: trauma surgeon. 97, 1994, pp. 144-150. PMID 8178182
- ^ R. Kdolsky et al.: Synthetic augmented repair of proximal ruptures of the anterior cruciate ligament. Long-term results of 66 patients. In: Clin Orthop. 295, 1993, pp. 183-189. PMID 8403646
- ↑ KE Rehm, KH Schultheis:. Band replacement with polydioxanone (PDS). In: Trauma Surgery. 11, 1985, pp. 264-273. PMID 3934825
- ↑ J. Amirault et al.: Chronic anterior cruciate ligament deficiency. Long-term results of MacIntohs's lateral substitution reconstruction. In: J Bone Joint Surg. 70, 1988, pp. 622-624. PMID 3403611
- ^ R. Bray et al .: Reconstruction for chronic anterior cruciate instability. A comparison of two methods after six years. In: J Bone Joint Surg. 70, 1988, pp. 100-105. PMID 3339039
- ↑ C. Frank, D. Jackson: Lateral substitution for chronic isolated anterior cruciate ligament deficiency. In: J Bone Joint Surg. 70, 1988, pp. 407-411. PMID 3372561 .
- ^ J. Reid et al .: The Ellison iliotibial-band transfer for a torn anterior cruciate ligament of the knee: Long-term follow-up. In: J Bone Joint Surg. 74, 1992, pp. 1392-1402. PMID 1429795
- ↑ T. Vail et al .: Long-term functional results in patients with anterolateral rotatory instability treated by iliotibial band transfer. In: Am J Sports Med. 20, 1992, pp. 274-282. PMID 1636857
- ↑ a b T. Engel et al .: Interligamentary rupture and osseous avulsion of the anterior cruciate ligament. In: Arthroscopy. 13, 2000, pp. 66-68. doi: 10.1007 / s001420050122 .
- ^ SA Taylor, MM Khair et al .: Primary Repair of the Anterior Cruciate Ligament: A Systematic Review. In: Arthroscopy. 31 (11), Nov 2015, pp. 2233-2247. PMID 26165465 , arthroscopyjournal.org doi: 10.1016 / j.arthro.2015.05.007 .
- ^ B. Di Matteo, M. Loibl et al .: Biologic agents for anterior cruciate ligament healing: A systematic review. In: World J Or thop. 7 (9), Sep 18, 2016, pp. 592-603. PMID 27672573 , doi: 10.5312 / wjo.v7.i9.592 .
- ↑ GS DiFelice, C. Villegas et al .: Anterior Cruciate Ligament Preservation: Early Results of a Novel Arthroscopic Technique for Suture Anchor Primary Anterior Cruciate Ligament Repair. In: Arthroscopy. 31 (11), Nov 2015, pp. 2162-2171. PMID 26542201 , doi: 10.1016 / j.arthro.2015.08.010 .
- ↑ P. Henle, K. Bieri et al .: Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. In: Knee Surg Sports Traumatol Arthrosc. May 18, 2017. PMID 28523340 link.springer.com doi: 10.1007 / s00167-017-4574-y .
- ^ A. Achtnich, E. Herbst, P. Forkel et al.: Acute Proximal Anterior Cruciate Ligament Tears: Outcomes After Arthroscopic Suture Anchor Repair Versus Anatomic Single-Bundle Reconstruction. In: Arthroscopy. 32 (12), Dec 2016, pp. 2562-2569. PMID 27324969 , doi: 10.1016 / j.arthro.2016.04.031 .
- ↑ GM Mackay, MJ Blyth et al .: A review of ligament augmentation with the InternalBrace: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. In: Surg Technol Int. May 26, 2015, pp. 239-255. PMID 26055016 .
- ↑ P. Henle, C. Röder et al .: Dynamic Intraligamentary Stabilization (DIS) for treatment of acute anterior cruciate ligament ruptures: case series experience of the first three years. In: BMC Musculoskelet Disord. 16, Feb 13, 2015, p. 27. PMID 25813910 , doi: 10.1186 / s12891-015-0484-7 .
- ↑ a b c d M. M. Murray: Current status and potential of primary ACL repair. In: Clinics in sports medicine. Volume 28, number 1, January 2009, pp. 51-61, doi: 10.1016 / j.csm.2008.08.005 . PMID 19064165 , PMC 2642924 (free full text) (review).
- ↑ a b S. L. Woo et al: Healing and repair of ligament injuries in the knee. In: Journal of the American Academy of Orthopedic Surgeons. 8, 2000, pp. 364-372. PMID 11104400
- ↑ J. Andrish, R. Holmes: Effects of synovial fluid on fibroblasts in tissue culture. In: Clin Orthop Relat Res. 138, 1979, pp. 279-283. PMID 445911
- ↑ D. Amiel et al .: Injury of the anterior cruciate ligament: the role of collagenase in ligament degeneration. In: J Orthop Res. 7, 1989, pp. 486-493. PMID 2544709
- ↑ DB Saris u. a .: Joint homeostasis. The discrepancy between old and fresh defects in cartilage repair. In: J Bone Joint Surg Br. 85, 2003, pp. 1067-1076. PMID 14516049
- ↑ M. Wiig et al .: Type I procollagen gene expression in normal and early healing of the medial collateral and anterior cruciate ligaments in rabbits: an in situ hybridization study. In: J Orthop Res. 9, 1991, pp. 374-382. PMID 2010841
- ↑ RM Lyon et al .: Ultrastructural differences between the cells of the medical collateral and the anterior cruciate ligaments. In: Clin Orthop. 272, 1991, pp. 279-286. PMID 1934745
- ↑ CN Nagineni: Characterization of the intrinsic properties of the anterior cruciate and medial collateral ligament cells: an in vitro cell culture study. In: J Orthop Res. 10, 1992, pp. 465-475. PMID 1613622
- ↑ DS Gesink et al .: Immunohistochemical localization of beta 1-integrins in anterior cruciate and medial collateral ligaments of human and rabbit. In: J Orthop Res. 10, 1992, pp. 596-599. PMID 1377240
- ↑ PJ Schreck et al .: Integrin display increases in the wounded rabbit medial collateral ligament but not the wounded anterior cruciate ligament. In: J Orthop Res. 13, 1995, pp. 174-183. PMID 7722754 .
- ↑ J. Lee, FL Harwood, WH Akeson, D. Amiel: Growth factor expression in healing rabbit medial collateral and anterior cruciate ligaments. In: The Iowa orthopedic journal. Volume 18, 1998, pp. 19-25. PMID 9807704 , PMC 2378181 (free full text).
- ↑ K. Kobayashi et al .: Novel method for the quantitative assessment of cell migration: a study on the motility of rabbit anterior cruciate (ACL) and medial collateral ligament (MCL) cells. In: Tissue Eng. 6, 2000, pp. 29-38. PMID 10941198 .
- ↑ a b M. M. Murray et al .: Histological changes in the human anterior cruciate ligament after rupture. In: J Bone Joint Surg Am. 82, 2000, pp. 1387-1397. PMID 11057466
- ↑ C. Frank et al .: Healing of the medial collateral ligament of the knee. A morphological and biochemical assessment in rabbits. In: Acta Orthop Scand. 54, 1983, pp. 917-923. PMID 6670520
- ↑ KP Spindler et al: Expression of collagen and matrix metalloproteinases in ruptured human anterior cruciate ligament: an in situ hybridization study. In: J Orthop Res. 14, 1996, pp. 857-861. PMID 8982126 .
- ↑ MM Murray et al .: Migration of cells from human anterior cruciate ligament explants into collagen-glycosaminoglycan scaffolds. In: J Orthop Res. 18, 2000, pp. 557-564. PMID 11052491 .
- ↑ MM Murray, M. Spector: The migration of cells from the ruptured human anterior cruciate ligament into collagen-glycosaminoglycan regeneration templates in vitro. In: Biomaterials. 22, 2001, pp. 2393-2402. PMID 11511036 .
- ↑ MM Murray et al .: Enhanced histologic repair in a central wound in the anterior cruciate ligament with a collagen-platelet-rich plasma scaffold. In: J Orthop Res. 25, 2007, pp. 1007-1017. PMID 17415785
- ^ AJ Harrold: The defect of blood coagulation in joints. In: Journal of clinical pathology. Volume 14, May 1961, pp. 305-308. PMID 13711857 , PMC 480217 (free full text).
- ^ D. Rosc et al .: Post-traumatic plasminogenesis in intraarticular exudate in the knee joint. In: Medical Science Monitor. 8, 2002, pp. CR371-378. PMID 12011780 .
- ↑ ME Wiig et al .: The early effect of high molecular weight hyaluronan (hyaluronic acid) on anterior cruciate ligament healing: an experimental study in rabbits. In: J Orthop Res. 8, 1990, pp. 425-434. PMID 2324860
- ↑ MM Murray et al.: Collagen platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament. In: J Orthop Res. 25, 2007, pp. 81-91. PMID 17031861 .
- ↑ KK Middleton, V. Barro et al .: Evaluation of the effects of platelet-rich plasma (PRP) therapy involved in the healing of sports-related soft tissue injuries. Iowa Orthop J. 32, 2012, pp. 150-63. PMID 23576936
- ↑ I. Dallo, J. Chahla include: Biologic Approaches for the Treatment of Partial Tears of the Anterior Cruciate Ligament: A Current Concepts Review. In: Orthop J Sports Med. 2017 Jan 25; 5 (1). PMID 28210653 , doi: 10.1177 / 2325967116681724 .
- ^ L. Andriolo, B. Di Matteo et al .: PRP Augmentation for ACL Reconstruction. Biomed Res Int. 2015, p. 371746. PMID 26064903 , doi: 10.1155 / 2015/371746 .
- ↑ JR Steadman et al: A minimally invasive technique ("healing response") to treat proximal ACL injuries in skeletally immature athletes. In: J Knee Surg. 19, 2006, pp. 8-13. PMID 16468488
- ^ R. Steadman et al .: Healing-response treatment for ACL injuries. In: Orthop Technol Rev. 3, 2002, 3
- ↑ K. Fehske et al. a .: The Healing Response Technique - a sufficient therapy option for partial ruptures of the anterior cruciate ligament? (PDF; 816 kB) 9/2009, Leipzig, Working Group for Arthroscopy, p. 24.
- ^ A b Franziskus Hospital Linz am Rhein: anterior cruciate ligament tear / cruciate ligament insufficiency. ( Memento of the original from September 3, 2014 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Retrieved March 12, 2010.
- ↑ J. Wasmaier, R. Kubik-Huch include: Proximal anterior cruciate ligament tears: the healing response technique versus conservative treatment. J Knee Surg. 26 (4), Aug 2013, pp. 263-71. PMID 23258320 , doi: 10.1055 / s-0032-1329720 .
- ↑ JR Steadman, LM Matheny et al .: Outcomes following healing response in older, active patients: a primary anterior cruciate ligament repair technique. J Knee Surg. 25 (3), Jul 2012, pp. 255-60. PMID 23057146 .
- ↑ J. Jorjani, D. Altmann et al.: Medium to long-term follow-up after anterior cruciate ligament rupture and repair in healing response technique. In: Z Orthop accident. 151 (6), Dec 2013, pp. 570-9. PMID 24347411 , doi: 10.1055 / s-0033-1350874 .
- ^ A b D. Altmann: Operative standard for recent cruciate ligament injuries. ( Memento from February 22, 2014 in the Internet Archive ) (PDF; 247 kB). In: Trauma and Occupational Disease. 8, 2006, pp. S150-S154. doi: 10.1007 / s10039-006-1156-5 .
- ↑ University Clinic Gießen and Marburg: ( Page no longer available , search in web archives ) Latest treatment options for anterior cruciate ligament tear. (PDF). In: Newsletter. May 6, 2006.
- ^ WG Rodkey et al .: Healing of a surgically created partial detachment of the posterior cruciate ligament using marrow stimulation: an experimental study in dogs. In: J Knee Surg. 19, 2006, pp. 14-18. PMID 16468489
- ↑ P. Lobenhoffer et al.: Ruptures of the posterior cruciate ligament: current treatment status In: trauma surgeon. 99, 1996, pp. 382-399. PMID 8767134
- ↑ A. Weiler u. a .: Arthroscopically assisted posterior cruciate ligament surgery and posterolateral stabilization with semitendinosus gracilis tendons. In: trauma surgeon. 109, 2006, pp. 61-71. PMID 16385417
- ^ FR Noyes, S. Barber-Westin: Posterior cruciate ligament replacement with a two-strand quadriceps tendon-patellar bone autograft and a tibial inlay technique. J Bone Joint Surg Am 87, 2005, pp. 1241-1252. PMID 15930532
- ↑ J. Kvist: Rehabilitation Following anterior cruciate ligament injury: current recommendations for sports participation. In: Sports Med. 34, 2004, pp 269-280. PMID 15049718
- ↑ LS Lohmander u. a .: High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. In: Arthritis Rheum. 50, 2004, pp. 3145-3152. doi: 10.1002 / art.20589 . PMID 15476248 .
- ↑ H. Seitz et al.: Meniscus lesions after an isolated anterior cruciate ligament rupture. In: Wien Klin Wochenschr. 108, 1996, pp. 727-730. PMID 9157718 .
- ↑ BE Øiestad et al .: Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. In: Am J Sports Med. 37, 2009, pp. 1434-1443. PMID 19567666 (Review)
- ^ AJ Hart et al .: Assessment of osteoarthritis after reconstruction of the anterior cruciate ligament: a study using single-photon emission computed tomography at ten years. In: J Bone Joint Surg Br. 87, 2005, pp. 1483-1487. PMID 16260663
- ^ RA Magnussen et al .: Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. In: J Knee Surg. 22, 2009, pp. 347-357. PMID 19902731 (Review)
- ↑ J. Gillquist, K. Messner: Anterior cruciate ligament reconstruction and the long-term incidence of gonarthrosis. In: Sports Med. 27, 1999, pp. 143-156. PMID 10222538 (Review)
- ↑ SM Joy: Osteoarthritis after anterior cruciate ligament injury: the quadriceps question. In: Exerc Sport Sci Rev 37, 2009, p. 112. PMID 19550201
- ↑ LS Lohmander et al .: The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. In: Am J Sports Med. 35, 2007, pp. 1756-1769. PMID 17761605 .
- ↑ SL Keays et al: Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. In: Am J Sports Med. 38, 2010, pp. 455-463. PMID 20051501 .
- ^ KR Ford, GD Myer, TE Hewett: Valgus knee motion during landing in high school female and male basketball players. In: Med Sci Sports Exerc. 35 (10), 2003, pp. 1745-1750.
- ↑ MV Paterno, LC Schmitt, KR Ford and others. a .: Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. In: American Journal Sports Medicine. 38 (10), (2010), pp. 1968-1978.
- ^ V. Ferrer-Roca, X. Balius Matas, O. Domínguez-Castrillo and a .: Avaluació dels factors de risc de lesió del lligament encreuat anterior de jugadors de futbol d'alt nivell. In: Apunts: Medicina de l'esport. (49): 181 (electronic without page counting); German: Arnd Krüger : anterior cruciate ligament. In: competitive sport. 44 (2014), 2, pp. 38-39.
- ↑ a b H. Louboutin et al .: Osteoarthritis in patients with anterior cruciate ligament rupture: a review of risk factors. In: Knee. 16, 2009, pp. 239-244. PMID 19097796 (Review)
- ^ A. Friedl: Footballers live dangerously. In: Berliner Morgenpost. June 10, 2008.
- ↑ B. Engström et al .: Does a major knee injury definitely sideline an elite soccer player? In: Am J Sports Med. 18, 1990, pp. 101-105. PMID 2301681 .
- ↑ R. Bahr, T. Krosshaug: Understanding injury mechanisms: a key component of preventing injuries in sport. In: British journal of sports medicine. Volume 39, Number 6, June 2005, pp. 324-329. doi: 10.1136 / bjsm.2005.018341 . PMID 15911600 , PMC 1725226 (free full text) (review).
- ^ A b E. Alentorn-Geli et al: Prevention of non-contact anterior cruciate ligament injuries in soccer players. Part 2: a review of prevention programs aimed to modify risk factors and to reduce injury rates. In: Knee Surg Sports Traumatol Arthrosc. 17, 2009, pp. 859-879. PMID 19506834 (Review)
- ↑ MV Paterno, LC Schmitt, KR Ford and others. a .: Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. In: American Journal Sports Medicine. 38 (10), 2010, pp. 1968-1988.
- ^ Arnd Krüger : Anterior cruciate ligament. In: competitive sport. 44, 2, 2014, pp. 38-39.
- ↑ J. Gilchrist et al .: A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. In: Am J Sports Med. 36, 2008, pp. 1476-1483. PMID 18658019
- ↑ aclprevent.com: PEP Program. ( Memento from January 5, 2009 in the Internet Archive ) Prevent injury, Enhance Performance = PEP, description of the warm-up exercises
- ↑ MK Zebis et al .: The effects of neuromuscular training on knee joint motor control during sidecutting in female elite soccer and handball players. In: Clinical Journal of Sports Medicine. 18, 2008, pp. 329-337. PMID 18614884
- ↑ Science of Soccer Online: Cutting-Edge Research: ACL Injury Prevention - Neuromuscular Training. July 29, 2008, accessed March 6, 2010.
- ^ TE Hewett et al: Prevention of anterior cruciate ligament injuries. In: Curr Womens Health Rep. 1, 2001, pp. 218-224. PMID 12112973 .
- ↑ G. Cerulli et al .: Proprioceptive training and prevention of anterior cruciate ligament injuries in soccer. In: J Orthop Sports Phys Ther. 31, 2001, pp. 655-660. PMID 11720298
- ^ A. Caraffa et al .: Prevention of anterior cruciate ligament injuries in soccer. A prospective controlled study of proprioceptive training. In: Knee Surg Sports Traumatol Arthrosc. 4, 1996, pp. 19-21. PMID 8963746
- ↑ a b M. Gruber: The neuromuscular control of the knee joint before and after a specific sensorimotor training in uninjured athletes. (PDF; 4.9 MB) Dissertation, University of Stuttgart, 2001, p. 53.
- ↑ RM Biedert among others: Sensorimotor function of the knee joint. In: Sports Orthopedics - Sports Traumatology. 14, 1998, pp. 186-194.
- ↑ a b O. E. Olsen, G. Mykleust, L. Engebretsen, I. Holme, R. Bahr: Exercises to prevent lower limb injuries in youth sports: cluster randomized controlled trial. In: BMJ (Clinical research ed.). Volume 330, number 7489, February 2005, p. 449, doi: 10.1136 / bmj.38330.632801.8F . PMID 15699058 , PMC 549653 (free full text).
- ^ W. Petersen et al .: A controlled prospective case control study of a prevention training program in female team handball players: the German experience. In: Arch Orthop Trauma Surg. 125, 2005, pp. 614-621. PMID 15703919
- ^ HJ Silvers et al.: Anterior cruciate ligament tear prevention in the female athlete. In: Curr Sports Med Rep. 4, 2005, pp. 341-343. PMID 16282037 .
- ↑ H. Himmelreich et al: Prevention of sports injuries and sports damage. In: White Paper Prevention - Mobile? Verlag Springer, 2008, doi : 10.1007 / 978-3-540-77274-3_7 ISBN 3-540-77273-1 , pp. 143-151. limited preview in Google Book search.
- ^ JW Orchard, H. Seward: Decreased incidence of knee posterior cruciate ligament injury in Australian Football League after ruck rule change. In: Br J Sports Med. 43, 2009, pp. 1026-1030. PMID 19850572
- ↑ F. Povacz: history of trauma surgery. Verlag Springer, 2007, p. 244, doi: 10.1007 / 978-3-540-74845-8 ( limited preview in the Google book search).
- ↑ W. Weber, E. Weber: Mechanics of human walking tools: an anatomical-physiological investigation. Dieterichsche Buchhandlung, Göttingen, 1835 ( full text in the Google book search).
- ^ A b J. Karlsson: History of Cruciate Ligament Repair. In: Repair and Regeneration of Ligaments, Tendons, and Joint Capsule. WR Walsh (Ed.). Humana Press, 2006, ISBN 1-58829-174-X , pp. 135-142, doi: 10.1385 / 1-59259-942-7: 135 ( limited preview in Google Book Search).
- ^ A. Bonnet: Traité des maladies des articulations. Volume 2, Verlag JB Baillière, 1945 ( full text in the Google book search)
- ↑ RD Galway et al .: Privot shift: A clinical sign of symptomatic anterior cruciate insufficiency. In: J Bone Jt Surg. 54B, 1972, p. 763.
- ^ R. Galway: Lateral pivot shift injury of the knee. In: J Bone Jt Surg. 53-B, 1971, pp. 772-773.
- ^ HR Galway, DL MacIntosh: The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. In: Clin Orthop Relat Res. 147, 1980, pp. 45-50. PMID 7371314 .
- ^ A. Bonnet: Traité de thérapeutique des maladies articulaires. Verlag JB Baillière, 1853. ( full text in Google book search)
- ^ A. Bonnet: Traité de thérapeutique des maladies articulaires. Verlag JB Baillière, 1853, p. 345 ( full text in the Google book search)
- ^ FH Fu: Current Concepts in ACL Reconstruction. SLACK Incorporated, 2008, ISBN 978-1-55642-813-5 limited preview in Google Book Search.
- ↑ J. Stark: Two cases of ruptured cucial ligaments of the knee joint. In: Edinburgh Med Surg. 74, 1850, pp. 267-269.
- ↑ A. Poncet: arrachement de l'epine du tibia a l'insertion du ligament croise anterieur. In: Bull et mem Soc de chir de Paris. 1, 1875, pp. 883-884.
- ↑ Sir Arthur Mayo-Robson, KBE, CB In: Br Med J. 3798, 1933, pp. 761-762. PMID 12986638 .
- ^ AW Mayo Robson: Ruptured crucial ligaments and their repair by operation. In: Ann Surg 37, 1903, pp. 716-718. PMID 17861289 .
- ^ W. Battle: A case after open section of knee joint for irreducible traumatic dislocation. In: Clin Soc London Trans. 33, 1900, p. 232.
- ↑ H. Goetjes: About violations of the ligaments of the knee joint cruciate. In: Dtsch Z Chir. 123, 1913, pp. 221-289.
- ^ R. Jones: Disabilities of the knee joint. In: British medical journal. Volume 2, Number 2901, August 1916, pp. 169-172. PMID 20768234 , PMC 2348969 (free full text).
- ^ F. Baumgartl: Injuries to the cruciate ligaments. In: F. Baumgartl (Ed.): The knee joint. Verlag Springer, 1964, p. 149.
- ↑ M. Lange: Treatment of joint damage. In: Accident Orthopedics. M. Lange (Ed.) Verlag Enke, p. 263.
- ↑ a b K. Lindemann: About the plastic replacement of the cruciate ligaments by pedunculated tendon grafts. In: Z Orthop. 79, 1950, pp. 316-334.
- ↑ F. Lutz: Experiences and results with plastic replacement of the cruciate ligaments in the knee joint according to Niederecker. In: Arch Orthop trauma surgeon. 46, 1954, pp. 439-444.
- ↑ D. O'Donoghue: Surgical treatment of fresh injuries to the major ligaments of the knee. In: J Bone Joint Surg Am. 32, 1950, pp. 721-738. PMID 14784482 .
- ^ F. Schmid, W. Bandi: Injury to the medial collateral ligament (MSB) and the anterior cruciate ligament (ACL) on the knee joint and its operative-functional treatment according to Lemaire. In: European Journal of Trauma. 14, 1988, pp. 124-129, doi : 10.1007 / BF02806640 (currently unavailable) .
- ^ PB Roth: Fracture of the spine of the tibia. (PDF). In: J Bone Joint Surg. 10, 1928, pp. 509-518.
- ↑ W. Müller: The development of the operative treatment of the "internal knee lesions". ( Memento of August 2, 2012 in the archive.today web archive ) Retrieved on February 7, 2010.
- ↑ E. Hesse: About the replacement of the cruciate ligaments of the knee joint by free fascia transplantation. In: Verh Dtsch Ges Chir. 43, 1914, pp. 188-189.
- ^ EW Hey-Groves: Operation for repair of the crucial ligament. In: Lancet. 2, 1917, p. 674.
- ^ EW Hey Groves: The crucial ligaments of the knee joint; their function, rupture and the operative treatment of the same. In: Br J Surg. 7, 1920, pp. 505-515.
- ↑ A. Heverhagen: long-term results after anterior cruciate ligament reconstruction with patellar tendon. (PDF; 1.8 MB) Dissertation, Philipps University Marburg, 2009.
- ^ GA Snook: A short history of the anterior cruciate ligament and the treatment of tears. In: Clinical Orthopedics. 172, 1983, pp. 11-13. PMID 6336998 .
- ^ A. Wittek: Cruciate ligament replacement from the patellar ligament (after zur Verth). In: Switzerland Med Wochenschr. 65, 1935, pp. 103-104.
- ↑ On Verth: Discussion of the 27th Congress, 5.-7. September 1932, Mannheim. In: Verh Dtsch Orthop Ges. 1933, pp. 268–270.
- ^ AH Edwards: Rupture and repair of the anterior cruciate ligament. In: Br J Surg 13, 1926, pp. 432-438.
- ↑ S. Rupp et al.: Replacement of the anterior cruciate ligament with the patellar tendon transplant. In: Orthopedist. 31, 2002, pp. 751-757. PMID 12426753 (Review).
- ^ H. Brückner: A new method of the cruciate ligament plastic. In: surgeon. 37, 1966, pp. 413-414.