Cruciate ligament retention
Under cruciate ligament maintenance and cruciate ligament healing , various therapy methods are added up that are applied immediately after a cruciate ligament tear with the aim of preserving the torn ligament and allowing it to heal stably. These methods were developed in the 1990s and 2000s, and there are only a few positive studies, but still no larger or comparative studies and no long-term results, they are not yet a generally recognized standard. Rather, this is cruciate ligament surgery.
background
As with other ligaments , the anterior cruciate ligament also has a strong intrinsic healing potential after an acute tear , so that it is possible for the cruciate ligament to heal by itself. Without therapy, however, it usually happens that the two ligament stumps do not heal together, but that the anterior portion of the torn anterior cruciate ligament is scarred directly on the posterior cruciate ligament , which is referred to as "Lambda / Wittek healing". This unwanted biological connection at the wrong point of attachment is mostly inadequate and not sufficiently stable. When preserving the cruciate ligament, the existing biological potential should therefore be used specifically to heal and restore the ligament continuity in order to achieve acceptable knee stability. As a result, this therapeutic approach differs significantly from cruciate ligament replacement through cruciate ligament surgery, in which the torn cruciate ligament is removed and replaced with an endogenous tendon or ligament.
Methods are also being developed to preserve the posterior cruciate ligament after an acute tear and to bring it to a stable healing.
History of the cruciate ligament suture
The basic idea of cruciate ligament retention is based on an old method, the results of which were not convincing at the time. In the 1980s it was common practice to sew torn cruciate ligaments directly together. Some patients showed good clinical results, but many cruciate ligaments did not heal together with sufficient stability or tore again. One of the main reasons for this was that the cruciate ligament did not always have sufficient tension, as would have been necessary during the healing phase. The knee joint lacked biomechanical stability . Because depending on the stretched or bent position of a knee, the respective tensile load changes constantly. As a result, the sutured cruciate ligament stumps pulled apart again and again when the knee joint was moved through, so that no stable scarring could take place.
Forms of therapy
If the aim is to preserve the anterior cruciate ligament after a tear ( rupture ), various therapeutic options are available.
Conservative therapy (without surgery)
It is a treatment approach without surgery, in which the natural healing process and muscle building through specific training are in the foreground. By wearing a movement- limiting orthosis , the injured cruciate ligament can be relieved and protected for its self-healing. In addition, physical therapy is used to strengthen the thigh and lower leg muscles in order to stabilize the affected knee joint as much as possible. If patients do not achieve full functionality as they did before the knee injury, they reduce their level of physical activity and switch to knee-friendly sports. If the knee stability is not sufficiently provided for a conservative therapy carried out at the end, then, a cruciate ligament replacement operation by tendons - graft be performed.
Another non-surgical approach is pursued with a special orthosis that was developed for injuries to the anterior cruciate ligament. Patients have to wear this orthosis (ACL Jack Brace) consistently for 13 weeks day and night and for a further 4 weeks during the day. With a set force of 7 kg, the knee is constantly pressed into a so-called rear drawer so that the torn cruciate ligament can grow back in the anatomically correct place.
Surgical procedures that preserve the cruciate ligament
Band-preserving surgical procedures must be performed as quickly as possible, within 3 weeks of the injury. Because the biological healing potential in the knee decreases rapidly and the natural ligament structure begins to shrink or retreat. The fact that such an early operation time significantly increases the risk of knee joint inflammation ( arthrofibrosis ) is now considered obsolete based on various studies.
Only special patients are eligible for cruciate ligament retention, so the decision for or against such a procedure mainly depends on the following factors: injury pattern, tear type & tear location, level of sport, age , gender, compliance .
Clinical experience with surgical cruciate ligament retention in children and adolescents is still very limited. The challenge here is to reposition the torn ligament and avoid damaging the still open growth plate.
In the ideal healing process, the injured cruciate ligament structure is stably scarred again, the nerve fibers can perform their function again and the important depth sensitivity is retained. The preparation of a tendon graft from the same leg is not required without exception; The associated complications at the extraction point cannot consequently occur. Depending on the study, the results so far seem to be comparable to those of a cruciate ligament replacement surgery or to show a slightly higher failure rate. The use of additional biological factors (e.g. platelet-rich plasma ) can potentially accelerate the healing process and improve the result of the hoped-for, stable scarring .
The absence from work is significantly shorter and the patients are able to work again after 3–4 weeks with light physical work.
In general, when preserving the cruciate ligament, a distinction can be made between unyielding, rigid procedures and dynamically based augmentation. Biomechanical studies show that only a dynamically augmented stabilization of the injured cruciate ligament - with individual pre-tensioning - achieves the natural kinematics of an intact cruciate ligament. The tests measured the anterior translation in relation to different knee flexion angles (see drawer test ) for available systems of cruciate ligament retention. Both the sole suture (Marshall suture) and the rigid augmentation (InternalBrace) show strikingly significant deviations from a natural condition of the cruciate ligament.
Healing Response Technique
This technique was developed by surgeon Richard Steadman (Vail / Colorado). By freshening the cruciate ligament (microfracture) at its tear-off point on the thigh - with a sharp awl - the body's own healing mechanisms are stimulated. The torn cruciate ligament is returned to the anatomically correct position without resorting to a fixing suture. The knee joint is stretched in an orthosis for around 6 weeks . The medical procedure must take place within a few days of the injury .
Dynamic Intraligamentary Stabilization (DIS)
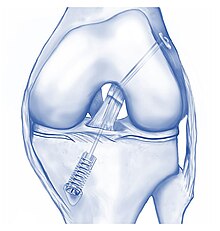
The dynamic intraligamentary stabilization (DIS) was developed by S. Eggli in Switzerland in 2009 and was awarded the innovation prize of the German Society for Trauma Surgery (DGU). It is based on a dynamically stabilized augmentation of the ligament with an implant called Ligamys . The manufacturer is Mathys AG .
Within three weeks after the accident, the torn cruciate ligament can be pulled and attached to the naturally correct attachment point in an operation ( arthroscopy ) with targeted sutures. These sutures completely resorb after a few weeks. In addition, a thin makes polyethylene - thread the necessary stability in the knee joint. This high-tech thread is particularly tear-resistant and well tolerated by the human body.
The thread is locked in a metallic spring element in the shin . Depending on the patient's body weight, an individual preload (60–80 Newtons ) is set, which is similar to the intact cruciate ligament. During bending and stretching movements, the dynamic suspension ensures that the regenerating ligament is relieved and can heal for several months. The tear strength of the polyethylene tape is over 2,000 Newtons . This dimensioning relates to the conditions in the intact cruciate ligament, the maximum tensile load of which was shown in biomechanical tests to be approx. 2,200 Newtons. Intact cruciate ligaments in men can withstand higher tearing forces than those of women. As with the healing response technique, a microfracture is performed around the point of attachment of the cruciate ligament on the thigh to promote healing. Due to the respective flexion of the knee, an angle-dependent change in length of up to 6.7 mm is found in the anterior cruciate ligament. The spring mechanism of a dynamic stabilization accordingly enables an adaptive, reversible expansion of up to 8 mm. In contrast to this, rigid augmentation methods have no possibility of such a flexible length adjustment.
Clinical data on the dynamic intraligamental stabilization in more than 15 peer-reviewed - articles of medical journals published .
Refixation: InternalBrace & Primary Repair
This philosophy is based on a rigid refixation of the cruciate ligament in its original position. The stabilization of the joint is primarily ensured by an implanted plastic band and an external orthosis . The surgical techniques for this are different. The manufacturer is Arthrex . The first variant uses a TightRope RT with a FibreTape ( polyethylene UHMWPE) for the splint and a SwiveLock anchor for the fixation in the lower leg . The injured cruciate ligament is repositioned using non-absorbable sutures. The maximum tear strength of the FibreTape is 217-315 Newtons .
A second possibility is to attach the injured cruciate ligament to the femur with two SwiveLock anchors (Ø 4.75 mm) and a FiberWire suture. The maximum tear strength of this implant system is 712 Newtons .
There is also a third version in which the injured cruciate ligament is fixed directly to the thighbone using FiberWire and PushLock anchors. The maximum tear strength of a PushLock anchor is given in the literature as 254 Newtons .
In all three variants, the knee joint is stabilized in a rigid manner and without reversible dynamics. A patient-specific preload can not be set on the implant . A microfracture is carried out during the operation. Patients wear an orthosis with restricted mobility for six weeks . For reattachment using Internal Brace technique are published three peer review - professional articles available.
Bridged-Enhanced ACL Repair (BEAR)
This treatment method was developed in America and is still being tested ( clinical study ). The injured cruciate ligament is repositioned with a suture and at the same time the tear site is covered with a blood-soaked, collagen sponge (scaffold). There is no internal knee stabilization to protect the healing ligament. Patients must wear an orthosis with restricted mobility for six weeks .
further reading
- D. Kohn: knee - expertise in orthopedics and trauma surgery. Thieme Verlag, 2016, ISBN 978-3-13-175001-3 , p. 237.
- W. Petersen, M. Herbort: Arthroscopy on the knee joint. The practice book of techniques and indications. Schattauer Verlag, ISBN 978-3-7945-3217-9 .
- MJ Strobel, T. Zantop: Arthroscopic surgery. Part I: knee joint. Volume 3: Anterior cruciate ligament (ACL). VKB: -revision. ISBN 978-3-642-41552-4 .
- R. Siebold, D. Dejour, S. Zaffagnini: Anterior Cruciate Ligament Reconstruction. A Practical Surgical Guide. Springer Verlag, 2016, ISBN 978-3-662-51083-4 .
Web links
- Diagnosis of the knee ligament apparatus: AGA committee knee ligament
- Innovations in Orthopedics: Anterior Cruciate Ligament (ACL) Treatment
Individual evidence
- ↑ M. Costa-Paz, MA Ayerza, I. Tanoira et al: Spontaneous Healing in Complete ACL Ruptures: A Clinical and MRI Study. In: Clin Orthop Relat Res. Volume 470, No. 4, Apr 2012, pp. 979-985. PMID 21643922 doi: 10.1007 / s11999-011-1933-8 .
- ↑ M. Deie, M. Ochi, Y. Ikuta: High intrinsic healing potential of human anterior cruciate ligament. In: Acta Orthop Scand. Volume 66, No. 1, Feb 1995, pp. 28-32. PMID 7863763 doi: 10.3109 / 17453679508994634 .
- ↑ GA Malanga, J. Girardi, SF Nadler: The spontaneous healing of a torn anterior cruciate ligament. In: Clin J Sport Med. Volume 11, No. 2, Apr 2001, pp. 118-120. PMID 11403112 Clinical Journal of Sport Medicine .
- ↑ EH Crain, DC Fithian, EW Paxton et al .: Variation in anterior cruciate ligament scar pattern: Does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? In: Arthroscopy. Volume 21, No. 1, Jan 2005, pp. 19-24. PMID 15650662 doi: 10.1016 / j.arthro.2004.09.015 .
- ↑ a b C. Kösters, M. Herbort, B. Schliemann et al .: Dynamic intraligamentary stabilization of the anterior cruciate ligament. Operative technique and short-term clinical results. In: trauma surgeon. Volume 118, No. 4, Apr 2015, pp. 364-371. PMID 25835209 doi: 10.1007 / s00113-015-2745-1 .
- ↑ CH Henry, W. Schmölz, R. Mayr include: Biomechanical evaluation of a novel dynamic posterior cruciate ligament brace. In: Clin Biomech (Bristol, Avon). Volume 33, Mar 2016, pp. 20-25. PMID 26896691 doi: 10.1016 / j.clinbiomech.2016.02.001 .
- ^ A b T. Lind, HV Johannsen, J. Lauritzen: Results after primary suture of rupture of the anterior cruciate ligament. A 4-5 year follow-up. In: Ugeskr Laeger. Vol. 152, No. 10, Mar 5, 1990, pp. 670-672. PMID 2181749 .
- ↑ a b L. Engebretsen, P. Benum, S. Sundalsvoll: Primary suture of the anterior cruciate ligament. A 6-year follow-up of 74 cases. In: Acta Orthop Scand. Volume 60, No. 5, Oct 1989, pp. 561-564. PMID 2603656 .
- ↑ JP Laboureau, A. Cazenave: Recent ruptures of the anterior cruciate ligament. Suture technique on a reinforcement ligament. Results of a 5 years' experience. In: Rev Chir Orthop Reparatrice Appar Mot. Volume 77, No. 2, 1991, pp. 92-102. PMID 1829253
- ↑ P. Lobenhoffer, M. Blauth, H. Tscherne: Resorbable augmentationplasty and functional after care in fresh rupture of the anterior cruciate ligament. An improved treatment concept. In: Z Orthop your Grenzgeb. Volume 126, No. 3, May-Jun 1988, pp. 296-299. PMID 3145653 doi: 10.1055 / s-2008-1040206
- ↑ G. Hehl, W. Strecker, M. Richter et al .: Clinical experience with PDS II augmentation for operative treatment of acute proximal ACL ruptures - 2-year follow-up. In: Knee Surg Sports Traumatol Arthrosc. Volume 7, No. 2, 1999, pp. 102-106. PMID 10223532 doi: 10.1007 / s001670050130
- ↑ a b H. H. Paessler, J. Deneke, LE Dahners: Augmented repair and early mobilization of acute anterior cruciate ligament injuries. In: Am J Sports Med. Volume 20, No. 6, Nov-Dec 1992, pp. 667-674. PMID 1456360 doi: 10.1177 / 036354659202000607
- ^ WG Clancy, JM Ray, DJ Zoltan: Acute tears of the anterior cruciate ligament. Surgical versus conservative treatment. In: J Bone Joint Surg Am. Volume 70, No. 10, Dec 1988, pp. 1483-1488. PMID 3198673
- ↑ M. Odensten, P. Hamberg, M. Nordin: Surgical or conservative treatment of the acutely torn anterior cruciate ligament. A randomized study with short-term follow-up observations. In: Clin Orthop Relat Res. Volume 198, Sep 1985, pp 87-93. PMID 3896609
- ↑ T. Strand, LB Engesaeter, AO Mølster et al.: Knee function following suture of fresh tear of the anterior cruciate ligament. In: Acta Orthop Scand. Vol. 55, No. 2, Apr 1984, pp. 181-184. PMID 6711285
- ↑ a b M. F. Sherman, L. Lieber, JR Bonamo et al: The long-term followup of primary anterior cruciate ligament repair. Defining a rational for augmentation. In: Am J Sports Med. Volume 19, No. 3, May-Jun 1991, pp. 243-255. PMID 1867333 doi: 10.1177 / 036354659101900307
- ↑ N. Kaplan, T. Wickiewicz, RF Warren: Primary surgical treatment of anterior cruciate ligament ruptures. A long-term follow-up study. In: Am J Sports Med. Volume 18, No. 4, Jul-Aug 1990, pp. 354-358. PMID 2206080 doi: 10.1177 / 036354659001800404
- ↑ G. Blatter, R. Tissi: Does the suturing of the ruptured anterior cruciate ligament make sense without augmentation? In: Trauma Surgery. Volume 17, 1991, p. 232. PMID 1949360 doi: 10.1007 / BF02588692
- ↑ A. Harilainen, P. Myllynen: Treatment of fresh tears of the anterior cruciate ligament. A comparison of primary suture and augmentation with carbon fiber. In: Injury. Volume 18, No. 6, Nov 1987, pp. 396-400. PMID 3334238
- ↑ H. Boszotta, R. Wendrinsky, G. Sauer: A new technique for arthroscopic reinsertion and augmentation of the freshly torn anterior cruciate ligament. In: Trauma Surgery. Volume 14, 1988, p. 46. PMID 3070755 doi: 10.1007 / BF02807975
- ^ SA Taylor, MM Khair, TR Roberts et al: Primary Repair of the Anterior Cruciate Ligament: A Systematic Review. In: Arthroscopy. Volume 31, No. 11, Nov 2015, pp. 2233-2247. PMID 26165465 doi: 10.1016 / j.arthro.2015.05.007
- ↑ CL Ardern, NF Taylor, JA Feller et al .: Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. In: Br J Sports Med. Volume 48, 2014, pp. 1543-1552. PMID 25157180 doi: 10.1136 / bjsports-2013-093398
- ↑ M. Jacobi, N. Reischl, K. Rönn et al: Healing of the Acutely Injured Anterior Cruciate Ligament: Functional Treatment with the ACL-Jack, a Dynamic Posterior Drawer Brace. In: Adv Orthop. 2016. PMID 28053787 doi: 10.1155 / 2016/1609067
- ↑ E. Herbst, C. Hoser, P. Gföller et al .: Impact of surgical timing on the outcome of anterior cruciate ligament reconstruction. In: Knee Surg Sports Traumatol Arthrosc. Volume 25, No. 2, Feb 2017, pp. 569-577. PMID 27549214 doi: 10.1007 / s00167-016-4291-y
- ^ TO Smith, L. Davies, CB Hing: Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. In: Knee Surg Sports Traumatol Arthrosc. Volume 18, No. 3, Mar 2010, pp. 304-311. PMID 19838672 doi: 10.1007 / s00167-009-0965-z
- ↑ B. Li, Bai L. Fu Y. et al: Effect of Timing of Surgery in Partially Injured ACLs. In: Orthopedics. Volume 35, No. 5, May 2012, pp. 408-412. PMID 22588397 doi: 10.3928 / 01477447-20120426-08
- ↑ P. Henle, KS Bieri, M. Brand et al .: Patient and surgical characteristics that affect revision risk in dynamic intraligamentary stabilization of the anterior cruciate ligament. In: Knee Surg Sports Traumatol Arthrosc. 2017. PMID 28523340 doi: 10.1007 / s00167-017-4574-y
- ↑ a b c d e G. S. DiFelice, C. Villegas, S. Taylor: Anterior Cruciate Ligament Preservation: Early Results of a Novel Arthroscopic Technique for Suture Anchor Primary Anterior Cruciate Ligament Repair. In: Arthroscopy. Volume 31, No. 11, Nov 2015, pp. 2162-2171. PMID 26542201 doi: 10.1016 / j.arthro.2015.08.010
- ↑ a b c d e f A. Achtnich, E. Herbst, P. Forkel et al .: Acute Proximal Anterior Cruciate Ligament Tears: Outcomes After Arthroscopic Suture Anchor Repair Versus Anatomic Single-Bundle Reconstruction. In: Arthroscopy. Volume 32, No. 12, Dec 2016, pp. 2562-2569. PMID 27324969 doi: 10.1016 / j.arthro.2016.04.031
- ↑ LE Stanley, ZY Kerr, TP Dompier: Sex Differences in the Incidence of Anterior Cruciate Ligament, Medial Collateral Ligament, and Meniscal Injuries in Collegiate and High School Sports: 2009-2010 Through 2013-2014. In: Am J Sports Med. Volume 44, No. 6, Jun 2016, pp. 1565-1572. PMID 26940226 doi: 10.1177 / 0363546516630927
- ^ CC Prodromos, Y. Han, J. Rogowski et al: A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. In: Arthroscopy. Volume 23, No. 12, Dec 2007, pp. 1320-1325.e6. PMID 18063176 doi: 10.1016 / j.arthro.2007.07.003
- ↑ M. Bigoni, D. Gaddi, M. Gorla: Arthroscopic anterior cruciate ligament repair for proximal anterior cruciate ligament tears in skeletally immature patients: Surgical technique and preliminary results. In: Knee. Volume 24, No. 1, Jan 2017, pp. 40-48. PMID 27815015 doi: 10.1016 / j.knee.2016.09.017
- ↑ JO Smith, SK Yasen, HC Palmer et al .: Pediatric ACL repair reinforced with temporary internal bracing. In: Knee Surg Sports Traumatol Arthrosc. Volume 24, No. 6, Jun 2016, pp. 1845-1851. PMID 27141865 doi: 10.1007 / s00167-016-4150-x
- ↑ D. Bagsby, G. Gantsoudes, R. Klitzman: Intrinsic Healing of the Anterior Cruciate Ligament in an Adolescent. In: Am J Orthop (Belle Mead NJ). Volume 44, No. 8, Aug 2015, pp. E294-E297. PMID 26251948 The American Journal of Orthopedics
- ↑ P. Faunø, L. Rømer, T. Nielsen et al: The Risk of Transphyseal Drilling in Skeletally Immature Patients With Anterior Cruciate Ligament Injury. In: Orthop J Sports Med. Volume 4, No. 9, Sep 6, 2016. PMID 27648453 doi: 10.1177 / 2325967116664685
- ↑ B. Sonnery-Cottet, C. Bazille, C. Hulet et al .: Histological features of the ACL remnant in partial tears. In: Knee. Volume 21, No. 6, Dec 2014, pp. 1009-1013. PMID 25112212 doi: 10.1016 / j.knee.2014.07.020
- ^ J. Haus, Z. Halata: Innervation of the anterior cruciate ligament. In: Int Orthop. Volume 14, No. 3, 1990, pp. 293-296. PMID 2279838
- ↑ HJ Kim, JH Lee, DH Lee: Proprioception in Patients With Anterior Cruciate Ligament Tears. In: Am J Sports Med. Dec. 1, 2016. PMID 28060536 doi: 10.1177 / 0363546516682231
- ↑ K. Bali, MS Dhillon, RK Vasistha et al .: Efficacy of immunohistological methods in detecting functionally viable mechanoreceptors in the remnant stumps of injured anterior cruciate ligaments and its clinical importance. In: Knee Surg Sports Traumatol Arthrosc. Volume 20, No. 1, Jan 2012, pp. 75-80. PMID 21541706 doi: 10.1007 / s00167-011-1526-9
- ↑ JM Konrath, CJ Vertullo, BA Kennedy et al .: Morphologic Characteristics and Strength of the Hamstring Muscles Remain Altered at 2 Years After Use of a Hamstring Tendon Graft in Anterior Cruciate Ligament Reconstruction. In: Am J Sports Med. Volume 44, No. 10, Oct 2016, pp. 2589-2598. PMID 27432052 doi: 10.1177 / 0363546516651441
- ↑ KS Bieri, SM Scholz, S. Kohl, E. Aghayev, L. Staub: Dynamic intraligamentary stabilization versus conventional ACL reconstruction: A matched study on return to work. In: Injury. Volume 48, No. 6, Jun 2017, pp. 1243-1248. PMID 28318538 doi: 10.1016 / j.injury.2017.03.004
- ↑ R. Stößlein, F. Reuther: 1 year Ligamys - our own results, examples and problems with this innovative new procedure in anterior cruciate ligament surgery. In: The Orthopedic Journal of Sports Medicine. Volume 4, No. 3 (suppl 2), 2016, doi: 10.1177 / 2325967116S00054
- ↑ a b L. Büchler, D. Regli, DS Evangelopoulos et al: Functional recovery following primary ACL repair with dynamic intraligamentary stabilization. In: Knee. Volume 23, No. 3, Jun 2016, pp. 549-553. PMID 26972809 doi: 10.1016 / j.knee.2016.01.012
- ↑ I. Dallo, J. Chahla, JJ Mitchell include: Biologic Approaches for the Treatment of Partial Tears of the Anterior Cruciate Ligament: A Current Concepts Review. In: Orthop J Sports Med. Volume 5, No. 1, Jan 25, 2017. PMID 28210653 doi: 10.1177 / 2325967116681724
- ↑ B. Di Matteo, M. Loibl, L. Andriolo et al .: Biologic agents for anterior cruciate ligament healing: A systematic review. In: World J Orthop. Volume 7, No. 9, Sep 18, 2016, pp. 592-603. PMID 27672573 doi: 10.5312 / wjo.v7.i9.592
- ↑ CE da Silveira Franciozi, SJ Ingham, GC Gracitelli: Updates in biological therapies for knee injuries: anterior cruciate ligament. In: Curr Rev Musculoskelet Med. Volume 7, No. 3, Sep 2014. PMID 25070265 doi: 10.1007 / s12178-014-9228-9
- ↑ L. Fallouh, K. Nakagawa, T. Sasho et al .: Effects of autologous platelet-rich plasma on cell viability and collagen synthesis in injured human anterior cruciate ligament. J Bone Joint Surg Am. Volume 92, No. 18, Dec 15, 2010, pp. 2909-2916. PMID 21159991 doi: 10.2106 / JBJS.I.01158
- ↑ J. Menetrey, Ch. Kasemkijwattana, Ch. S. Day et al .: Direct-, Fibroblast- and Myoblast-Mediated Gene Transfer to the Anterior Cruciate Ligament. In: Tissue Eng. Volume 5, No. 5, Oct 1999, pp. 435-442. PMID 10586099 doi: 10.1089 / ten.1999.5.435
- ↑ M. Bierbaum, O. Schöffski, B. Schliemann et al: Cost-utility analysis of dynamic intraligamentary stabilization versus early reconstruction after rupture of the anterior cruciate ligament. In: Health Econ Rev. Volume 7, No. 1 Dec 2017, p. 8. PMID 28168633 doi: 10.1186 / s13561-017-0143-9
- ↑ a b B. Schliemann, M. Herbort, S. Lenschow and others: Dynamic intraligamentary stabilization of fresh ruptures of the anterior cruciate ligament (Ligamys) - Rethinking cruciate ligament surgery? In: Trauma Occupational Illness. Volume 18, (Suppl 3), 2016, p. 254. doi: 10.1007 / s10039-015-0080-y
- ↑ MM Murray, BM Flutie, LA Kalish et al: The Bridge-Enhanced Anterior Cruciate Ligament Repair (BEAR) Procedure: An Early Feasibility Cohort Study. In: Orthop J Sports Med. Volume 4, No. 11, Nov 21, 2016. PMID 27900338 doi: 10.1177 / 2325967116672176
- ↑ JL Marshall, RF Warren, TL Wickiewicz: Primary surgical treatment of anterior cruciate ligament lesions. In: Am J Sports Med. Volume 10, No. 2, Mar-Apr 1982, pp. 103-107. PMID 7081522 doi: 10.1177 / 036354658201000208
- ↑ AG Roy, RAG Hoogeslag, RW Brouwer, RH Veld: Improved control of knee laxity after 'dynamic' augmentation of ACL suture repair: Biomechanical comparison of three ACL suture repair techniques in the human cadaveric knee. In: ISAKOS Congress, ePoster. # 1071, Shanghai, June 2017. (isakos.com)
- ↑ a b c B. Schliemann, S. Lenschow, C. Domnick et al: Knee joint kinematics after dynamic intraligamentary stabilization: Cadaveric study on a novel anterior cruciate ligament repair technique. In: Knee Surg Sports Traumatol Arthrosc. Volume 25, No. 4, Apr 2017, pp. 1184-1190. PMID 26239862 doi: 10.1007 / s00167-015-3735-0
- ↑ a b c J. Häberli, P. Henle, YP Acklin and others: Knee joint kinematics with dynamic augmentation of primary anterior cruciate ligament repair - a biomechanical study. In: J Exp Orthop. Volume 3, No. 1, Dec 2016, p. 29. PMID 27783350 doi: 10.1186 / s40634-016-0064-2
- ↑ a b c d e J. R. Steadman, LM Matheny, KK Briggs et al .: Outcomes following healing response in older, active patients: a primary anterior cruciate ligament repair technique. In: J Knee Surg. Volume 25, No. 3, Jul 2012, pp. 255-260. PMID 23057146 Journal of Knee Surgery
- ↑ a b J. Jorjani, D. Altmann, R. floodplain include: Medium- to long-term follow-up after anterior cruciate ligament rupture and repair in healing response technique. In: Z Orthop accident. Volume 151, No. 6, Dec 2013, pp. 570-579. PMID 24347411 doi: 10.1055 / s-0033-1350874
- ↑ a b J. Wasmaier, R. Kubik-Huch, C. Pfirrmann: Proximal anterior cruciate ligament tears: the healing response technique versus conservative treatment. In: J Knee Surg. Volume 26, No. 4, Aug 2013, pp. 263-271. PMID 23258320 doi: 10.1055 / s-0032-1329720
- ↑ S. Eggli, H. Kohlhof, M. Zumstein et al: Dynamic intraligamentary stabilization: novel technique for preserving the ruptured ACL. In: Knee Surg Sports Traumatol Arthrosc. Volume 23, No. 4, Apr 2015, pp. 1215-1221. PMID 24651979 doi: 10.1007 / s00167-014-2949-x
- ↑ a b P. Henle, C. Röder, G Perler: inter alia: Dynamic Intraligamentary Stabilization (DIS) for treatment of acute anterior cruciate ligament ruptures: case series experience of the first three years. In: BMC Musculoskelet Disord. 16, Feb 13, 2015, p. 27. PMID 25813910 doi: 10.1186 / s12891-015-0484-7
- ↑ a b c S. Eggli, C. Röder, G. Perler et al .: Five year results of the first ten ACL patients treated with dynamic intraligamentary stabilization. In: BMC Musculoskelet Disord. 17, Feb. 27, 2016, p. 105. PMID 26920141 doi: 10.1186 / s12891-016-0961-7
- ↑ Ph. Henle: ligament-retaining surgical technique with Ligamys. A new option for treating anterior cruciate ligament rupture. In: Jatros. November 26, 2015. Universimed - medicine in focus
- ↑ M. Herbort, C. Kösters: Dynamic intraligamentary stabilization for the treatment of a fresh ACL rupture (Ligamys): OP technique - first experiences and results. In: DKG Newsletter. 1/2015 German Knee Society (DKG)
- ↑ M. Hirschmann: Alternative to Reconstruction. Suturing the anterior cruciate ligament - useful for which patients? In: Medicalsports Network. No. 07, 2014 Medicalsports Network
- ^ B. Rieger, MT Hirschmann: Arthrofibrosis after biologically augmented primary ACL suture repair - what do we know? In: Sports Orthop. Traumatol. 31, 2015, pp. 309-315. Sports Orthopedics and Traumatology
- ↑ C. Kösters: Dynamic intraligamentary stabilization of the anterior cruciate ligament vs. Reconstruction using a semitendinosus tendon. New cruciate ligament retention technique has comparable results after twelve months. In: DKOU Congress Program. No. 10, 2016. German Congress for Orthopedics and Trauma Surgery
- ↑ NJ Rowden, D. Sher, GJ Rogers et al: Anterior cruciate ligament graft fixation. Initial comparison of patellar tendon and semitendinosus autografts in young fresh cadavers. In: Am J Sports Med. Volume 25, No. 4, Jul-Aug 1997, pp. 472-478. PMID 9240980 doi: 10.1177 / 036354659702500409
- ↑ SL Woo, JM Hollis, DJ Adams et al .: Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. In: Am J Sports Med. Volume 19, No. 3, May-Jun 1991, pp. 217-225. PMID 1867330 doi: 10.1177 / 036354659101900303
- ↑ N. Chandrashekar, H. Mansouri, JR Slauterbeck et al .: The mechanical properties of human anterior cruciate ligament are depending on sex. In: 52nd Annual Meeting of the Orthopedic Research Society. 03/2006 - Paper No. 0076 Orthopedic Research Society
- ↑ AM Krismer, L. Gousopoulos, S. Kohl et al .: Factors influencing the success of anterior cruciate ligament repair with dynamic intraligamentary stabilization. In: Knee Surg Sports Traumatol Arthrosc. Feb 17, 2017. PMID 28210790 doi: 10.1007 / s00167-017-4445-6
- ↑ DS Evangelopoulos, S. Kohl, S. Schwienbacher et al.: Collagen application reduces complication rates of mid-substance ACL tears treated with dynamic intraligamentary stabilization. In: Knee Surg Sports Traumatol Arthrosc. Nov 12, 2015. PMID 26564213 doi: 10.1007 / s00167-015-3838-7
- ^ S. Kohl, DS Evangelopoulos, MO Schär et al .: Dynamic intraligamentary stabilization: initial experience with treatment of acute ACL ruptures. In: Bone Joint J. Volume 98-B, No. 6, Jun 2016, pp. 793-798. PMID 27235522 doi: 10.1302 / 0301-620X.98B6.35040
- ↑ JH Lubowitz: Anatomic ACL reconstruction produces greater graft length change during knee range-of-motion than transtibial technique. In: Knee Surg Sports Traumatol Arthrosc. Volume 22, No. 5, May 2014, pp. 1190-1195. PMID 24077671 doi: 10.1007 / s00167-013-2694-6
- ↑ a b c G. M. Mackay, MJ Blyth, I. Anthony: A review of ligament augmentation with the InternalBrace ™: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. In: Surg Technol Int. Volume 26, May 2015, pp. 239-255. PMID 26055016
- ^ JP Van der List, GS DiFelice: Gap formation following primary repair of the anterior cruciate ligament: A biomechanical evaluation. PMID 27955813 doi: 10.1016 / j.knee.2016.10.009
- ↑ RW Liu, PH Lam, HM Shepherd et al .: Tape Versus Suture in Arthroscopic Rotator Cuff Repair: Biomechanical Analysis and Assessment of Failure Rates at 6 Months. In: Orthop J Sports Med. Volume 5, No. 4, Apr 17, 2017. PMID 28451619 doi: 10.1177 / 2325967117701212
- ↑ NA Viens, CA Wijdicks, KJ Campbell et al: Anterior talofibular ligament ruptures, part 1: biomechanical comparison of augmented Broström repair techniques with the intact anterior talofibular ligament. In: Am J Sports Med. Volume 42, No. 2, Feb 2014, pp. 405-411. PMID 24275864 doi: 10.1177 / 0363546513510141
- ^ FA Barber, MA Herbert, RC Beavis: Suture anchor materials, eyelets, and designs: update 2008. In: Arthroscopy. Volume 24, No. 8, Aug 2008, pp. 859-867. PMID 18657733 doi: 10.1016 / j.arthro.2008.03.006
- ^ R. Burgess, S. Elder, R. McLaughlin et al .: In vitro biomechanical evaluation and comparison of FiberWire, FiberTape, OrthoFiber, and nylon leader line for potential use during extraarticular stabilization of canine cruciate deficient stifles. In: Vet Surg. Volume 39, No. 2, Feb 2010, pp. 208-215. PMID 20210968 doi: 10.1111 / j.1532-950X.2009.00637.x
- ^ FA Barber, O. Hapa, JA Bynum: Comparative Testing by Cyclic Loading of Rotator Cuff Suture Anchors Containing Multiple High-Strength Sutures. In: Arthroscopy. Volume 26 (9 Suppl), Sep 2010, pp. S134-S141. PMID 20810088 doi: 10.1016 / j.arthro.2010.03.007