Amoebic dysentery
| Classification according to ICD-10 | |
|---|---|
| A06.0 | Acute amoebic dysentery |
| ICD-10 online (WHO version 2019) | |
The amoebic dysentery or amoebic dysentery , a form of amebiasis is associated with abdominal pain, bloody mucous diarrhea and tenesmus accompanying infection of the intestine through the amoeba Entamoeba histolytica , a unicellular organism ( protozoan ). With around 50 million cases of disease worldwide every year, it is one of the most common protozoal infections in humans.
Word origin
The word Ruhr was derived from the old Germanic verb “ rüeren , ruoren ”. The noun later specifically referred to the violent movement in the abdomen.
Pathogen
Amebiasis is an infectious disease caused by an amoeba of the species Entamoeba histolytica . The protozoon was first described in 1875 as "Amöba coli" by Fedor Loesch in connection with a dysentery case , identified in 1883 by Stephanos Kartulis in 150 cases of dysentery and scientifically named Entamoeba histolytica as a pathogenic species in 1903 by Fritz Schaudinn .
The pathogens live in the food pulp of the human colon and reproduce asexually through cell division . In addition to mononuclear vegetative forms, the trophozoites , which mainly colonize the upper large intestine , the pathogen can also form very resistant permanent forms of cysts in the lower large intestine, which are typically quadrangular. It can remain in the colon - possibly for years without causing any signs of illness. It is eliminated with the stool, primarily in the form of cysts - up to 500 million per day. The infected person is thus also a carrier . In contrast to the vegetative form, the excreted permanent form can remain infectious in the outside world for months .
The smaller “minute form” of the trophozoites, which does not lead to the clinical picture of amoebic dysentery , is to be distinguished from the pathogenic “magna form” which is up to 50 micrometers in size and can phagocytize erythrocytes. For reasons unknown up to now, the pathogens can change and, in addition to changed DNA , show a changed enzyme pattern . As a result of various pathogenicity factors such as certain surface receptors, pore-forming enzymes and cysteine proteases, which decompose the extracellular matrix of the colon , the amoebic dysentery is complete. In rare cases, a chronic granulomatous inflammatory reaction can lead to pressure-sensitive tumors in the intestinal wall, a so-called amoeboma.

infection
The pathogens usually enter the large intestine as cysts, through oral ingestion of contaminated water , unwashed fruit or vegetables, or via an anal route.
Infection does not cause any symptoms in 90 percent of people, but as a symptom-free host they can excrete and transmit the pathogens.
Disease symptoms
Symptoms of the disease only appear in some of those infected with Entamoeba histolytica . After an incubation period of 1 to 7 days, the amoebic dysentery manifests itself in abdominal pain , diarrhea , tenesms and a bloody and slimy “raspberry jelly- like” stool . The symptoms often develop gradually over one to three weeks, usually without a fever. Serious illnesses, on the other hand, are febrile and associated with strong tenesms and up to 20 bloody stools per day.
These intestinal symptoms are signs of invasive amebiasis, in which trophozoites pass from the intestinal lumen into the lining of the large intestine. This leads to inflammation of the large intestine ( colitis ), which is ulcerated with circumscribed tissue defects ( ulcerations ). When the amoeba penetrate the vascular system through the intestinal mucosa, they can be transported further with the blood . This means that (extraintestinal) settlements of amoeba can form in other organs outside the intestine, and then abscesses there . Liver abscesses are by far the most common complication, the central nervous system , heart , spleen or urinary organs are rarely affected. These extraintestinal manifestations of invasive amebiasis can occur without prior amoebic dysentery, sometimes years after infection, and are life threatening.
Incidence of the disease
The amoebic dysentery is widespread worldwide, but occurs especially in tropical and subtropical areas, e.g. B. Kenya , Bangladesh , Indonesia , Thailand , India and Vietnam .
Unpeeled fruits and vegetables, ice cubes, and ice should be avoided in these areas. To brush your teeth, travelers in tropical countries should only use mineral water or water that has been boiled for at least five minutes. Conventional drinking water disinfection by chlorination is not enough to kill the amoeba.
Diagnosis and treatment
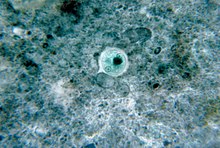
The pathogens can be identified through a microscopic examination of the feces. Note the possibility of confusing the Minuta form with the closely related amoeba Entamoeba dispar , which only causes diarrhea.
Diarrhea with blood or mucus should always be examined and diagnosed by a doctor, as other serious infections can also be responsible. Both the cyst shape and the magna shape can be detected in the stool. However, since the Magnaform is very sensitive and can be destroyed quickly, fresh stool must be examined. Amoebic dysentery is mainly treated with antibiotics (especially metronidazole ). Asymptomatic carriers are treated with paromomycin or diloxanide furoate . If taken in time, the disease heals quickly. However, if abscesses have already occurred in the liver or the like, medication (metronidazole, followed by paromomycin or diloxanide furoate) must be taken over a longer period of time. Surgery may also be required. Abscesses or organ involvement can be detected by sonography or computed tomography .
Reporting requirement
In Austria, communicable dysentery (amoebic dysentery) is a notifiable disease in accordance with Section 1 (1) of the 1950 Epidemic Act . The reporting obligation relates to suspected cases, illnesses and deaths. Doctors and laboratories, among others, are obliged to report this ( Section 3 Epidemics Act).
literature
- S1 guideline for diagnosis and therapy of amoebic dysentery of the German Society for Tropical Medicine and International Health (DTG). In: AWMF online (as of 2006)
- Karl Wurm, AM Walter: Infectious Diseases. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 9–223, here: pp. 140–142 ( Amöbenruhr ) and 145.
Individual evidence
- ↑ a b c d G. Burchard, E. Tannich: Epidemiology, diagnosis and therapy of amebiasis. In: Deutsches Ärzteblatt , Volume 101, No. 45, 2004, pp. 3036–3040 (A), online .
- ↑ Ruhr . Duden , 2016.
- ↑ Duden - The dictionary of origin . 4th edition. Mannheim / Leipzig / Vienna / Zurich 2006, ISBN 978-3-411-04074-2 .
- ↑ Karl Wurm, AM Walter: Infectious Diseases. 1961, p. 140.
- ↑ Werner Köhler : Infectious diseases. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 667-671, here: p. 670.
- ^ David Grove: Tapeworms, Lice, and Prions: A Compendium of Unpleasant Infections. Oxford University Press, Oxford 2014, ISBN 978-0-19-964102-4 , p. 108 f. books.google.de
- ^ Marianne Abele-Horn: Antimicrobial Therapy. Decision support for the treatment and prophylaxis of infectious diseases. With the collaboration of Werner Heinz, Hartwig Klinker, Johann Schurz and August Stich, 2nd, revised and expanded edition. Peter Wiehl, Marburg 2009, ISBN 978-3-927219-14-4 , p. 289.
