Ankle fracture
| Classification according to ICD-10 | |
|---|---|
| S82 | Fracture of the lower leg, including the upper ankle |
| S82.5 | Fracture of the inner tibia, involving the upper ankle |
| S82.6 | Fracture of the outer malleolus fibula, involving the ankle joint |
| S82.8 | Fractures of other parts of the lower leg - bimalleolar fracture - trimalleolar fracture |
| S93.2 | Traumatic rupture of ligaments at the level of the ankle and foot |
| ICD-10 online (WHO version 2019) | |
The ankle joint fracture ( Latin - anat. Malleolar fracture ) is a bone fracture of the upper ankle joint ( ankle ). It is the most common lower extremity fracture in adults .
anatomy
The ankle of the human (there is also a lower ankle [USG] below the ankle bone ) consists of the fibula ( fibula ), the tibia ( tibia ) and the ankle bone ( talus ). Tight ligaments hold the cartilage-coated ends of these bones together to form a joint : the anterior and the stronger posterior syndesmosis ligament connect the calf and shin bones to form the ankle joint; the shaft of the fibula and tibia, the lower leg above are by functionally equivalent area between bone band ( interosseous membrane associated). The ankle bone, which is fitted into the ankle joint , is kept flexible but stable by the outer or collateral ligaments ( ligamentum fibulotalare anterius , ligamentum fibulocalcaneare and ligamentum fibulotalare posterius ) and the roughly triangular inner ligament ( ligamentum deltoideum ). The load is transferred from the foot to the lower leg exclusively via the ankle bone and the lower horizontal joint surface of the shin bone. The ankles only serve to guide the joint laterally. The inner malleolus is an integral part of the broad, lower end of the shinbone, while the outer malleolus represents the tip of the fibula that is covered with cartilage on the joint side.
Because the ankle bone is not a simple, uniform bone roll, but rather represents a cylinder segment with different circular radii on the inside and outside, the movement of the upper ankle joint in flexion and extension does not form a mere hinge movement, but a so-called jaw clip movement.
Functional anatomy
Despite the individually differently pronounced wedge shape of the ankle roll, the fork of the upper ankle joint guides the ankle as closely as possible in all functional states. The outer and inner ankles show a convergence of the joint surfaces corresponding to the wedge shape. Plantar flexion does not result in a comprehensibly expanded mobility of the ankle bone in the fork, nor does dorsiflexion lead to a more than slight broadening of the outer fork dimensions. An attempt was made to explain such perfect joint mechanics by means of a moving axis of motion.
The range of motion of the ankle joint can be described for practical use with a joint axis that does not, however, intersect the inner ankle perpendicularly: When moving from plantar flexion to dorsiflexion, the ankle bone turns inwards and the fibula turns in the same direction around its longitudinal axis. This was confirmed by American students who screwed drill wires into the fibula in a self- experiment and were able to demonstrate the range of motion of the rotation in dorsiflexion / plantar extension by almost 20 °. In addition, in the strongest dorsal position, the fibula is slightly bent laterally (to the side) and the anterior syndesmosis is tensioned by its lateral and dorsal displacement. The different information on the joint closure in dorsiflexion or plantar flexion result from the special examination situation of anatomists and pathologists: Here the examinations are carried out on corpses lying on the dissection table and thus relieved extremities. On the other hand, under body load when walking, the joint closure of the malleolar cheeks is considerably tighter, the syndesmoses are given a clear pretension, and the deflection of the fibula under the hinge movement is reduced.
In addition, too little attention is paid to the functional aspects of the so-called “posterior” or third “malleolus”: The dorso-lateral tibia edge, which extends far beyond the talus roll with the tight posterior syndesmosis as the joint lip, represents an essential contact point of the joint, especially in plantar flexion: the The term ankle joint fork, which is common in German-speaking countries, does not do justice to either anatomical or physiological facts. The shape of the ankle surface of the tibia and fibula is therefore more appropriately referred to in English as mortise and in French as mortaise .
A bowl or pan is a functional Germanization.
Accident mechanism
The fracture of the upper ankle is always caused by a more or less severe dislocation (subluxation or dislocation ) of the joint, i. H. a loosening of the bones of the joint from their normal articulated connection with rupture of at least the outer malleolus and possible bony and ligamentous accompanying injuries. Therefore, the injury is basically called a dislocation fracture ( dislocation fracture ). An ankle fracture is shown in the dislocated position for illustration. The fractures usually reposition themselves due to the elasticity of the soft tissue covering, or they are repositioned by paramedics or sports trainers at the scene of the accident, so that such X-rays are rarely taken in clinics. The injury, popularly known as "twisting an ankle", is usually due to a pronation trauma or a supination (both indirect trauma ). This basic pattern is supplemented by rotation components (e.g. eversion, adduction ) of the foot. The ankle fracture can also be caused by twisting the lower leg against the stationary foot. Often the effects of compression are also effective, such as B. by jumping off a wall. According to Lauge-Hansen, the radiological fracture pattern can be assigned to a typical development mechanism (= causal classification).
Diagnosis
In addition to the history ( anamnesis ) and the clinical (physical) examination, the diagnosis requires an X-ray examination . It is made in the ap ( anterior-posterior ) beam path with 20 ° internal rotation and in the lateral beam path. With oblique images at an angle of 45 °, tears at the syndesmosis attachment of the tibia (French: Tubercule de Chaput Tillaux ) can be recognized. In case of doubt, a long exposure must always be made to rule out a high fibula fracture ( Maisonneuve fracture ). The injuries to the ligaments, which are invisible in the X-ray image, are revealed by an X-ray image converter examination after the anesthesia has been initiated , but before the actual surgical procedure begins.
In the case of skeletal anomalies and old fractures, but especially if the lower load-bearing joint surface of the tibia is involved, an additional computed tomography (digital X-ray layer examination) can provide clarity about the course of the fracture. Ligament damage and cartilage damage e.g. B. on the talus can be examined very precisely with a digital magnetic resonance tomography .
classification
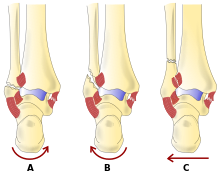
At present, the fractures for surgical treatment are preferably categorized anatomically according to Danis or derived from Weber , depending on the height of the fibula fracture in relation to the connective tissue connection between the fibula and tibia ( syndesmosis ). This classification was adopted by the Working Group for Osteosynthesis Questions ( AO ) in its classification and further differentiated:
| Type | Fracture localization | Syndesmosis Injury |
|---|---|---|
| A. | Fracture below the syndesmosis | Syndesmosis always intact |
| B. | Fracture at the level of the syndesmosis | Syndesmosis often injured as well |
| C. | Fracture above the syndesmosis | Syndesmosis always hurt too |
The extent of joint damage increases from A to C. Concomitant injuries such as the medial malleolus fracture and the posterior tibial fragment ( Volkmann's triangle ) can increase the extent of the joint damage.
This classification refers exclusively to the local position of the fibula fracture. From the assignment, one can approximately deduce the expected accompanying lesion of the fork-supporting ligaments of the syndesmosis region and the interosseous membrane .
The Lauge-Hansen classification is used less frequently. This classification is based on the position of the foot and the direction of movement of the talar roll at the time of the accident:
| Order of frequency |
classification | abbreviation | Position of the foot |
Direction of talar movement |
Common terminology |
|---|---|---|---|---|---|
| 1 | Supination / external rotation | SL | inversion | External rotation | External rotation injury without diastasis |
| 2 | Pronation / abduction | PA | Eversion | Abduction | Abduction injury |
| 3 | Pronation / external rotation | PL | inversion | External rotation | External rotation injury with diastasis |
| 4th | Supination / adduction | SA | inversion | Adduction | Adduction injury |
| 5 | Pronation / dorsiflexion | PD | Eversion | Dorsiflexion | Vertical compression fracture |
Accompanying injuries
As accompanying injuries, in addition to the always existing lesion on the outer ankle, there are also inner ankle fractures and, in the case of Weber B and C fractures, also lesions of the load-bearing lower shin surface. This is because the respective syndesmosis tape attaches to it at the back and front, so that when the fork tension is high, at the moment of the break with simultaneous load on z. B. the rear (triangular) hinge edge this is injured in the form of a combined tear-off break. This postero-lateral edge of the tibia, the so-called Volkmann triangle (after Richard von Volkmann 1872), is a prognostic indicator of a severe variation of a Weber B or C hernia, because a large amount of compression is necessary for its formation, the additional one Causes damage to the cartilage.
Syndesmosis lesion and Volkmann's triangle

The instability of the ankle joint fork is a result of the typical fracture mechanism, which principally tilts the ankle bone ( talus ) out of the fork. If this results in a fracture of the outside ankle below the syndesmosis , the fork stability is of course always unchanged ( Weber A fracture ). If, during the fracture origin for a fracture of the fibula ( fibula ) in the amount of Syndesmose, these will tear. Since this type of fracture ( Weber B fracture ) is an oblique fracture, the anterior syndesmosis tears while the rear (more stable) one remains connected to the fragment and opens outwards with the fragment like a door hinge. In Weber C fractures , tilting the ankle bone causes the syndesmosis region to explode before the remaining force breaks the fibula.
The syndesmosis can be damaged in two ways: Either both syndesmosis ligaments tear (and parts of the interosseous membrane up to the level of the fibular fracture). Much more often, however, the anterior, weaker syndesmosis ligament tears, and the posterior (more stable) one remains; instead, the ligament attachment tears over a wide area on the lower shin bone. Compression forces of the talus against the distal tibial joint surface contribute to this. This avulsion fracture, called Volkmann's triangle (or Volkmann's triangle), is possible in Weber B and very common in Weber C fractures and is the cause of complete fork instability of the upper ankle (see illustration).
forecast
In the case of fracture of the ankle joint, the extent of the joint cartilage damage generally determines the prognosis. This damage occurs either immediately in the accident through the fracture ends, the dislocation (see above) or through a compression component (fracture of the rear Volkmann triangle ). On the other hand, a poor joint position or instability after the fracture has healed also leads to increased wear and tear of the articular cartilage. Already about a year after the injury, signs of wear and tear (secondary or post-traumatic osteoarthritis ) with pain, restricted mobility and a tendency to swell appear on the upper ankle joint due to the pronounced strain . These changes are then largely irreversible, i.e. H. Corrective interventions carried out now can no longer eliminate the osteoarthritis.
treatment
Immediate action
If an ankle fracture is suspected, the leg should be immobilized and elevated to avoid additional pain and to minimize swelling. If the skin is intact, the ankle should be cooled to further reduce the swelling. An early treatment of the swelling is not only pain-relieving, but also enables an early operation, since if the swelling is severe, the operation usually has to be postponed until the soft tissue swelling has subsided. In the case of an open fracture, the wound must be covered aseptically in order to avoid infection of the wound and, in particular, a protracted bone infection.
A misalignment ( dislocation ) of the ankle should be corrected ( repositioning ) by medical specialists as soon as possible after the administration of painkillers and, if necessary, sedatives ( analgesia ). The ankle joint is straightened by strong, even pulling on the foot and then ideally immobilized with a vacuum splint. Early reduction in the case of a misaligned ankle fracture is useful in order to minimize the risk of pressure lesions on the thin skin over the inner and outer ankle. If the blood supply to the foot is interrupted due to the misalignment or nerves are damaged, an emergency surgical treatment must be carried out after rough repositioning in order to avoid permanent damage.
Conservative
A prerequisite for a good result is an anatomical (i.e. completely normal) restoration of the bone shape and stable joint guidance. Only unshifted fractures below the syndesmosis ( Weber A fractures) or minimally displaced Weber B fractures should therefore be treated conservatively without surgery using external stabilization (e.g. plaster of paris). In patients with circulatory disorders, for example due to age, vascular diseases , chronic nicotine abuse or diabetes mellitus , dislocated hernias should also be treated surgically either conservatively or minimally invasively. The fractures must be set up under anesthesia and the result of the reduction held with drill wires inserted percutaneously (through the skin) and the joint plastered. Open operations with exposure of the fragments have the great disadvantage of wound healing disorders, which considerably worsen the clinical result and can even ultimately lead to the amputation of the operated lower leg.
Operational
Osteosynthesis of the fibula
For all other fractures with displaced bone fragments and for injuries to the fork ligaments, an open operation with bone screwing ( osteosynthesis ) and ligament stabilization is usually necessary. The simplest and most biomechanically stable restoration is done with at least two to three lag screws, depending on the length of the oblique fracture of the fibula (Fig.). Solitary screw osteosynthesis is only possible in the case of simple spiral or oblique fractures, multiple fragment fractures are combined with single screws to form larger fragments, which are then stabilized with a plate that is screwed lengthways onto the fibula. In the other case shown, a lag screw and a 6-hole 1/3 tube plate were used as a so-called neutralization plate on the outer ankle and a tension strap on the inner ankle. Both restorations are stable during exercise; a plaster immobilization can be dispensed with. The patient is allowed to walk on forearm crutches with a light contact load .
Internal malleolus osteosynthesis
The medial malleolus fracture is usually an avulsion fracture. Conservative treatment is not possible here. Therefore, the inner malleolus must be exposed via a longitudinal incision. In the fracture gap that is always periosteum taken hindering the anatomical reduction. After moving the periosteum aside, the fracture can easily be anatomically reduced. The fragment is fixed with drill wires or with drill wire and lag screw (Fig.). The inner malleolus fragment rarely consists of several parts that can be fixed by several wires and possibly also a wire cerclage. A screw fixation is not possible with such multiple fragment fractures.
Stabilization of the joint fork
In the case of fork instability with rupture of the syndesmosis, the anterior syndesmosis must be inspected and, if necessary, sutured. The posterior Volkmann triangle with the posterior syndesmosis attached is a broad-based bony fragment of the posterior lower tibial articular surface. Flat fragments spontaneously heal reliably and reliably and can be neglected in the treatment of fractures. Larger fragments of more than 10% of the distal tibial articular surface must be anatomically fitted securely into the joint. To do this, they must be set up surgically and fixed with one or more screws.
The fibula-tibia ligament connection must be secured with a set screw. The purpose of the adjustment screw is to fit the initially stable fibula into the joint on the shinbone ( incisura fibularis ) and to adjust it there at the correct distance (hence adjustment screw). The screw must not exert a compression effect. For this reason, a thread must be created in both bones involved (fibula and tibia) for the implantation. Since the ankle joint fork must not become absolutely stable, but only elastically stable in order to enable the rotational movement of the fibula in the ankle joint, the adjusting screw is always removed six weeks after the ligament has healed. Adjusting screws that have remained for a long time or regularly loaded adjusting screws break and are then only very difficult to remove.
Aftercare
During these six weeks, it is essential to avoid the full load on an operated leg with an ankle fracture in order not to endanger the healing of the syndesmosis and to prevent the set screw from breaking. The relief is carried out with forearm crutches. If the osteosynthesis is carried out in a stable manner, so-called sole contact or rolling using forearm crutches is useful. Thrombosis prophylaxis with heparin must be carried out until the full load is reached after about six weeks . The osteosynthesis material used to stabilize the fracture should be removed from the ankle after about a year at the earliest. Simple lag screws can also remain.
Complications
The often very thin skin, together with the connective tissue damage caused by swelling and bony malalignment, easily lead to pressure necrosis of the skin, which occasionally even makes premature metal removal necessary. Particularly critical in this respect is the situation in which the joint remains in the dislocated position after the (dislocated) fracture, because the skin over the broken inner ankle is usually under massive tension. Here only the fastest possible rough repositioning (reduction) by pulling the heel longitudinally - if necessary also by laypersons (e.g. sports trainers) - can prevent the worst.
If the load is too early (insufficient compliance ), there is a risk of the osteosynthesis material being displaced or even erupting, resulting in failure of the fracture to heal or the formation of the false joint ( pseudarthrosis ). This complication occurs particularly frequently in older patients, whose bones offer little support for the osteosynthesis material due to osteoporosis and who also have problems with the safe implementation of the fracture relief using forearm crutches due to their older age. Therefore, special orthotic shoes are often used for this group of people .
Deep wound infections can lead to bone infection ( osteomyelitis ) and / or early massive osteoarthritis of the ankle. Surgical stiffening of the joint is often the only possible definitive measure to enable pain-free walking.
Immobilizing or relieving a leg leads to a significant increase in the risk of developing deep vein thrombosis , especially after operations . For prophylaxis , injections of low molecular weight heparin are performed daily .
Complications are particularly common in patients with circulatory disorders (e.g. heavy smokers) or in diabetics. This fact must urgently be taken into account when assessing the need for surgery (i.e. the indication ). This risk profile also has an influence on the surgical procedure: To avoid wound edge necrosis and possible subsequent wound infections, the operation should not be carried out with tourniquet.
In addition, inadequate reduction of the bone fracture can lead to incorrect healing ( malunion ) and painful functional restrictions up to post-traumatic osteoarthritis . Shortening or shifting (translation) of the distal outer malleolus fragment by 2 mm or tilting or rotating it by 5 ° leads to a significant change in the biomechanics and to the risk of instability and premature osteoarthritis - which is why an exact intraoperative reduction is necessary. Classically, in the case of a fracture of the outer malleolus, the distal fragment is displaced outwards (laterally) and then the talar roll tilts outwards (valgization). In rare cases, a corrective osteotomy is necessary.
An exact reduction is most likely to be seen in a correct X-ray of the ankle joint (ap with 20 ° internal rotation, so-called mortise view according to Weber). The joint gap is evenly wide inside, outside and above, an imaginary boundary line of the ankle joint shows only a small gap ( soft spot ) between the tibia and fibula, but no step formation. At the level of this soft spot , on the inside of the fibula, there is also a small thorn as an attachment to the anterior syndesmosis, which corresponds to the proximal end of the cartilage of the upper ankle and is displaced proximally when it is shortened. In addition, a circle can normally be imagined exactly in the distal contour of the tip of the outer malleolus and the lateral delimitation of the processus fibularis tali , but not in the case of a shortening of the outer malleolus. If the outer malleolus fragment is twisted, the congruence between the malleolus lateralis and the incisura fibularis tibiae is lost on the CT .
See also
literature
- Burghard Breitner, Franz Gschnitzer, Ernst Kern, Leonhard Schweiberer : Traumatology . In: Surgical operation theory . 2nd Edition. tape VIII , no. 1 . Urban & Schwarzenberg, Munich / Vienna / Baltimore 1987, ISBN 3-541-14482-3 , Conservative and operative fracture treatment.
- Burghard Breitner, Franz Gschnitzer, Ernst Kern, Leonhard Schweiberer: Traumatology . In: Surgical operation theory . 2nd Edition. tape XI , no. 4 . Urban & Schwarzenberg, Munich / Vienna / Baltimore 1987, ISBN 3-541-14512-9 , lower extremity.
- N. M. Meenen et al: Ankle fracture . Trauma surgery guidelines. 2nd Edition. Thieme, Stuttgart / New York 1998, ISBN 3-13-110262-4 .
- N. M. Meenen, D. E. Lorke, M. Westerhoff, M. Dallek, K. H. Jungbluth: Isolated fracture of Volkmann's triangle - a unique injury . In: Trauma Surgery . tape 19 , no. 2 , 1993, ISBN 3-13-110262-4 , pp. 98-107 .
- Michael Wagner, Klaus Dann: Ankle . In: Axel Rüter, Otmar Trenz, Michael Wagner (eds.): Trauma surgery . 1st edition. Urban & Schwarzenberg, Munich / Vienna / Baltimore 1995, ISBN 3-541-17201-0 , chap. 29 , p. 851 ff .
- B. G. Weber: The injury to the upper ankle joint . Hans Huber, Bern / Stuttgart 1966.
Web links
- Ankle fracture , Gesundheitsinformation.de , IQWiG health portal , April 4, 2018
- S1 guidelines for ankle fractures of the German Society for Trauma Surgery . In: AWMF online (June 2008)
- Guideline for malleolar fractures of the German Society for Orthopedics and Orthopedic Surgery and the Professional Association of Doctors for Orthopedics. In: AWMF online (as of April 2002)
Individual evidence
- ^ NM Meenen, DE Lorke, M. Westerhoff, M. Dallek, KH Jungbluth: The isolated fracture of the Volkmann triangle - an independent injury picture . In: Trauma Surgery , 19, 1993, pp. 98-107
- ↑ a b Wagner, Then; 1995, p. 854
- ^ Wagner, Then; 1995, p. 853
- ^ R. McRae, M. Esser: Practice of fracture treatment . 4th edition. Urban & Fischer bei Elsevier, Stuttgart / Munich 2009, ISBN 3-437-24850-2 , injuries in the area of the ankle, p. 382 ( books.google.de [accessed on January 23, 2011]).
- ↑ Ankle fracture . In: Guidelines of the German Society for Trauma Surgery . AWMF guidelines register No. 012/003, development stage: 1, AWMF online
- ↑ drk.de
- ↑ R. K. Marti, L. F. B. Raaymakers, S. Rammelt: Reconstruction of incorrectly healed ankle fractures. In: Foot & Ankle , 7, 2009, pp. 78–87.
- ^ BG Weber: Lengthening osteotomy of the fibula to correct a widened mortice of the ankle after fracture. In: Int Orthop , 4, 1981, pp. 289-293, PMID 7014480