Femoral neck fracture
| Classification according to ICD-10 | |
|---|---|
| S72.0 | Femoral neck fracture |
| ICD-10 online (WHO version 2019) | |
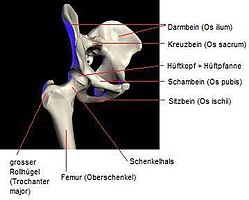
The femoral neck fracture (SHF, short for hip fracture or hip fracture ) is a hip near bone fracture (fracture) of the neck ( collum ) from the thigh bone ( femur ). This fracture is usually caused by falling on your side. It occurs particularly in old age (→ fall in old age ) and is then more common in women than in men due to osteoporosis .
Basics
hip joint
The hip joint is a ball joint with three degrees of freedom . The following ranges of motion are found in healthy people:
- Extension / flexion: 30 ° / 0 ° / 130 ° –150 °
- Abduction / expansion (abduction / adduction): 60 ° / 0 ° / 30 °
- Outward rotation / inward rotation (external rotation / internal rotation): 90 ° / 0 ° / 45 °
The joint is stabilized by a strong joint capsule. The blood flow to the joint including the femoral head is ensured in about 90% of cases by means of the medial circumflex artery and the lateral circumflex artery (both from the profunda femoris artery) and their branches radiating into the joint capsule. In about 15% of cases, the femoral head is additionally supplied via the femoral head artery (from the obturator artery), which extends to the femoral head in the capitis femoris ligament and radiates in via the femoral capitis fossa (in the joint socket).
Blood supply
The blood supply to the femoral neck and the femoral head is primarily taken over by the deep femoral artery ( Arteria profunda femoris ) with its branches - the Arteria circumflexa femoris lateralis , medialis and posterior. As their names suggest, the vessels run circularly around the femoral neck. If there is a fracture, there is a risk of injury to the vessels. Depending on the extent of the vascular injury, parts of the femoral neck and the femoral head can no longer be supplied with blood, so that femoral head necrosis can occur. The influence on the choice of therapy is great, because if femoral head necrosis is expected, joint-preserving therapy can usually no longer be selected.
The circumflexa arteries are connected to each other at different points ( natural anastomoses ). Such anastomoses occur in various places in the body and ensure further blood supply to the affected area if a vessel is injured or blocked. If the vascular ring on the femoral neck is interrupted in more than one place, this protective device can no longer function.
Etiology and causes
The femoral fractures near the hip joint are mostly caused by falls from a low height in older people. Accidents such as slipping, falling out of bed, falling due to weakness or dizziness are typical causes for the development of the fracture. Usually the fall occurs on the hip or the buttock region. The affected leg is not spread apart, but placed against the other leg ( adducted ). The so-called adduction fracture occurs . A fall on the splayed ( abducted ) leg, however, can lead to an abduction fracture .
Falling or falling, however, does not have to be a trigger for a broken bone, as a younger person with a healthy skeleton will rarely get a fracture if they fall on their side. Osteoporosis , the loss of hard bone substance ( calcium salt content ), means that bones can break more easily. Therefore, the femoral neck fracture is a typical fracture in the elderly.
Other factors that favor a fracture in a fall on the hip are: A deficient soft tissue covering (muscles, fat layer) of the hip, the point of impact (the closer to the hip itself, the more likely it is to fracture) and the lack of fall defense reflexes (spread of the Arms when falling to catch him).
The femoral neck fracture can also occur as a pathological fracture , with various previous illnesses or with bone tumors and metastases .
Classification
Femoral neck fractures are differentiated according to their location and the resulting consequences for treatment.
Classification according to fracture location
Medial femoral neck fracture
The medial femoral neck fracture is the most common fracture of the femur. It is a fracture of the femoral neck near or directly on the femoral head. In contrast to the lateral femoral neck fracture (see below), it lies within the joint capsule ( intracapsular ). Older textbooks only named the fracture directly on the femoral head as a medial femoral neck fracture and those that only lie in the region of the femoral neck near the femoral head as "intermediate". This term is no longer used today.
Lateral femoral neck fracture
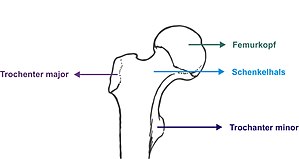
The lateral femoral neck fracture occurs with a frequency of about 5 percent, so it is rather rare. Young people are often affected after high-speed traumas such as B. Car accidents. It usually arises as an adduction fracture. Its fracture line lies directly on the greater trochanter , which is why it is often called a post-trochanteric fracture . It is an (extracapsular) fracture located outside of the joint capsule with greater possible blood loss.

Classification according to the direction of dislocation
A distinction is made between abduction fractures, adduction fractures and shear fractures. Abduction fractures occur when you fall onto the splayed (abducted) leg and are therefore rather rare. The fracture has a valgus position and is mostly indented and therefore resilient. Adduction fractures are common as they follow the typical fall to the side . The result is a varus position of the femoral neck with an upward dislocation of the femur, which leads to a shortening of the leg. When the fracture dislocates , the slipped femoral head often moves backwards ( retrotorsion fracture ), which also leads to a dorsal bone defect. The risk of damaging the vessels of the femoral head and thus the risk of femoral head necrosis is very high with this fracture. Shear fractures in the femoral neck area are rare and more likely to occur in younger patients as a result of tangential violence, for example in car accidents ( dashboard injury ) or falls from a great height. The prognosis is very poor due to the mostly severe dislocation and instability.
Classifications
There are three relevant classifications: One according to Pauwels (I-III), which is based on the angle between the horizontal and the fracture line , one according to Garden (I-IV), which is based on the degree of dislocation of the fracture , and one from the classification of the fractures of the working group for osteosynthesis issues .
| Classification of the medial femoral neck fracture according to Pauwels | ||
|---|---|---|
| Pauwels | angle | typical characteristics |
| I. | below 30 ° | Abduction fracture with resulting valgus position / compression |
| II | 30-50 ° | Adduction fracture , varus position |
| III | over 50 ° | Shear fracture with varus position |
| Prognostic fracture stages according to Garden | ||
|---|---|---|
| Garden | Fracture type | forecast |
| I. | Classic Pauwels I fracture in abduction without dislocation (slipping) of the head | good prognosis |
| II | slight axial indentations, no real dislocation. Fracture corresponds to an abduction fracture, angle> 60 ° | good prognosis with early reduction |
| III | Adduction fracture, corresponding to Pauwels III with severe dislocation, no interruption of the vascular supply to the dorsal cortex | unfavorable prognosis, repositioning necessary as soon as possible |
| IV | Adduction fracture with complete dislocation of the head and division of the vessels | poor prognosis, high rate of femoral head necrosis |
| AO classification of femoral neck fractures (31 = proximal femur) | ||
|---|---|---|
| Coding | Fracture type | |
| 31-B1 | Fracture subcapital (under / behind the head), impacted (indented), not or only slightly dislocated | |
| 31-B2 | transcervical fracture (corresponds to Pauwels II-III) | |
| 31-B3 | Subcapital fracture, not compressed, dislocated, possibly with fragmentation of the femoral neck | |
In medicine, classifications serve on the one hand as a prognostic aid, but above all as a therapeutic guideline. This is also the case with the three classifications listed here, all of which allow conclusions to be drawn about the probability of shearing or dislocation, and are therefore decisive for the choice of therapy.
Symptoms and clinical picture
Typical - especially for the medial femoral neck fracture - are the externally rotated and shortened leg on the affected side. In addition, there is usually severe pain in the groin and pounding pain over the large rolling mound ( greater trochanter see above ). Compressed and nondisplaced fractures can be asymptomatic. In these cases, the dull pain after an accident / fall is often mistaken for a bruise . It is not uncommon for patients with such fractures to walk to the doctor or to the clinic and report pain when walking. Fractures with severe dislocation, for example when the femoral head has completely slipped off, cause extreme pain and come to the clinic as an emergency. Femoral neck fractures with dislocation usually do not require a long diagnosis, the finding is literally eye-catching. The typical signs of compression or, depending on the type of fracture, possible dislocations of the femoral head can be seen in the X-ray image.
therapy
Femoral neck fractures are usually treated surgically as an "emergency with postponed urgency". As a rule, a basic internal diagnosis is carried out, possibly followed by appropriate acute therapy. In Germany, surgical therapy must be carried out within 24 hours if there are no serious medical reasons preventing it or the general condition of the patient allows it. For this purpose, there has been a mandatory guideline of the Federal Joint Committee since July 1, 2020 in Germany , which obliges all hospitals to maintain appropriate standards and resources. Although the scientific evidence in the analysis of the IQTiG shows a clear superiority of rapid surgical care within 24 hours, in Germany there have been considerable quality deficiencies in many hospitals for many years , which systematically prevented this.
In the case of compressed abduction fractures with a very low risk of shearing off, the treatment is more conservative (i.e. non-surgical), but a so-called prophylactic screw connection ( osteosynthesis ) can be carried out.
The goal of every form of therapy for femoral neck fractures is the earliest possible mobilization . The immobilization of the patient should be kept as short as possible.
Operative therapy
Medial femoral neck fracture
The medial femoral neck fracture in the elderly is often treated by implanting a total hip endoprosthesis or hemiprosthesis ( dual head prosthesis ). This procedure is justified with the high risk of later femoral head necrosis . For this reason, the older patient should be spared a second operation if possible. Furthermore, after a total endoprosthesis or dual head prosthesis, patients can put weight on the affected side again much more quickly, which considerably reduces the risk of impending immobility for the predominantly older patients.
Younger patients with a low general risk of surgery are more likely to use femoral head-conserving procedures. The aim here is to have an operation within a few hours in order to minimize the risk of femoral head necrosis. Preserving the natural joint means a better quality of life. This justifies the fact that in the case of femoral head necrosis, a second operation is more reasonable.
So-called undisplaced (i.e. undisplaced) or indented medial femoral neck fractures with a flat fracture inclination angle are often treated with so-called lag screws (see figure). These are hollow screws that are screwed over previously inserted guide wires ( cannulated screws ). In younger patients, attempts are usually made to preserve the head of the femur. Screws are also used for this.
- Lag screw fixation for a medial fracture. Treatment of a nondisplaced medial femoral neck fracture in a 92-year-old patient.
After surgery with lag screws, ap exposure. You can see the Redon drainage still in place .
Lateral femoral neck fracture
Fractures in the base of the femoral neck are treated with an osteosynthesis , depending on the degree of dislocation, often in order to preserve the joints . The treatment concept largely corresponds to that of pertrochanteric femoral fractures . Various procedures can be used, including gamma nail osteosynthesis, dynamic hip screw fitting (DHS) and the like.
|
|
Complications
Blood loss in fractures near the hip joint can reach proportions that lead to the occurrence of blood loss anemia . The picture of acute volume deficiency shock is rather rare in the femoral neck fracture due to the anatomical conditions (tight muscular guidance of the joint and the resulting "self-tamponade" of the bleeding), in particular much less frequently than in the pertrochanteric fracture or the femoral shaft fracture .
Injuries to the sciatic nerve only occur in the case of extreme misalignment (dislocation), as do injuries to the femoral nerve .
Pronounced muscle injuries with additional bleeding are rather rare in the typical femoral neck fractures in old people and are only found in very pronounced deformities.
The greater the degree of dislocation, the higher the likelihood of later femoral head necrosis , due to the destruction of blood flow to the femoral head via the joint capsule in the event of severe dislocation. Aseptic femoral head necrosis is a complication of the screw connection , which necessitates secondary implantation of a hip prosthesis. Surgical measures to preserve the femoral head are therefore only advisable in younger patients with little fracture dislocation.
Wound healing disorders and deep infections can also occur here, as after any operation. Other general complications, especially after surgery and when you are in bed, are thrombosis , embolism , pressure ulcers and pneumonia . Prolonged bed rest is particularly dangerous for older patients, since they are vitally more susceptible to such complications, especially to pressure ulcers.
Follow-up treatment and rehabilitation
Early mobilization is the most important element of follow-up treatment. If possible, the patients are placed on the edge of the bed on the first day after the operation , and if the patient tolerates this, the first steps are taken under physiotherapeutic guidance. There are also active and passive movement exercises in bed. Physiotherapy is continued throughout the entire inpatient stay, which usually lasts 2 to 3 weeks. In particular, patients who have not been treated with a load-stable procedure have to learn to use forearm crutches and climb stairs safely during this time.
Effective pain relief not only serves the “comfort” of the patient, but is an indispensable prerequisite for early mobilization. For this purpose, strong centrally acting analgesics (e.g. opioids ) should be avoided as early as possible in favor of non-opioid analgesics ( NSAIDs , metamizole , paracetamol ) in order to avoid mobilization caused by the side effects such as fatigue and dizziness that regularly occur with opioids and impaired drive weakness. Analgesics are not administered "as needed" but according to a schedule that is standardized in most clinics. If this is not enough, additional analgesics are given generously and at an early stage. In the first few days after the operation, an epidural catheter placed before the operation can also help combat pain.
It is also important to treat the comorbidities ( diabetes mellitus , arterial hypertension , cardiac insufficiency , renal insufficiency ) that are common in this age group , as these worsen in the course of accidents and surgery and can also represent an obstacle to mobilization. Often the internist is asked for advice on this .
After discharge from inpatient treatment, in Germany there is usually at least three weeks of inpatient follow-up treatment in a suitable rehabilitation clinic . The prerequisite for this is a Barthel index of at least 70. Patients who do not reach this mobility level due to age or illness are either transferred to geriatric early rehabilitation or to a short-term and transitional care facility. The aim of a rehabilitation stay is to restore the patient's former mobility and independence. The focus is on exercises to promote mobility and muscle building. By practicing a safe gait pattern, the risk of falling should be reduced.
Prevention
The femoral neck fracture is not only the most common injury to the thigh near the joint, it is also the most common fracture in the elderly. There are many reasons why an accident or fall can occur. Often older people do not drink enough fluids due to the feeling of thirst that decreases with age . This leads to low blood pressure and not infrequently to dizziness. Another reason can be the unsteady gait caused by other diseases, such as the spine or leg joints. Cardiovascular medication that is dosed or taken incorrectly is often the cause of dizziness and unsteady gait. Regardless of the cause of a fall, it is important to avoid it as much as possible by taking appropriate measures.
Another effective method to prevent femoral neck fractures are hip protectors , which, however, require a well-developed willingness to cooperate on the part of the patient.
Since femoral neck fractures in older patients are in most cases fractures favored by osteoporosis , prophylaxis with treatment of osteoporosis according to appropriate guidelines is possible. For this purpose z. B. Bisphosphonates (blockers of bone-degrading osteoclasts ) supplemented with vitamin D3 and calcium. A fracture of the head of the humerus, spine, femoral neck or wrist in the elderly is often a sign of osteoporosis, whose treatment according to guidelines can prevent further fractures. The treatment (see above) is very effective.
Sleep pills are also dangerous for old people because they reduce the ability to react and then e.g. B. can cause falls when going to the toilet at night.
history
In 1898, based on his own animal studies, Nicolas Senn suggested immobilization in a pelvic cast after exact repositioning. Böhler initially treated in an extension bandage and then continued the treatment in a pelvic and leg cast. These conservative treatment concepts have not been carried out for a long time because of the long immobilization required with its complications ( thrombosis , pulmonary embolism , hypostatic pneumonia , decubitus and others).
The first attempts at surgical treatment using extra-articular screws go back to Langenbeck (1858) and König (1875). However, the results were initially unsatisfactory due to the inadequate reduction and the poorly precise positioning of the screws.
The development of modern forms of care goes back to Smith-Petersen , who stabilized the femoral neck fracture from 1925 with a Mercedes star-shaped lamellar nail. The suggestion of a guide wire to improve retention and more precise nail placement by Sven Johansson in 1932 is still standard today in most femoral head-preserving surgical procedures. From 1942 - parallel to the development of the Küntschernagels for intramedullary nailing in the case of shaft fractures - a threaded screw was used with which the fracture ends could be brought closer together according to the principle of the lag screw . This principle can still be found today in many modern therapy methods.
In the 1950s, Puhg and Pohl recognized that complications such as implant breakout and head perforation were the result of the rigidity of the implants. The “Pohl's tab screw” resulting from this knowledge is guided distally in a directional sliding sleeve that allowed the fracture to be “sintered” by shortening the femoral neck without the risk of dislocation. This implant was the model for the development of the dynamic hip screw (DHS) by the AO in the early 1980s. This is still one of the most common implants today.
Elastic round and bundle nails have been suggested by various authors. The best known were the "endernails", elastic bundle nails, which were developed in 1970 and are introduced intramedullary from the knee and driven forward into the femoral head due to their predetermined curvature. With a well-chosen indication, these nails were able to achieve high stability while maintaining dynamics in the fracture gap. However, the procedure is burdened with a high rate of complications (head perforations, wandering of the nails with knee problems, long fluoroscopy times and high dependence on the skill of the surgeon) and is now rarely used.
The 90 ° and 135 ° angle plate developed by the AO in the early 1960s also frequently led to the above-mentioned complications of rigid systems and was largely replaced by the DHS and various intramedullary nails with femoral neck components in the treatment of femoral neck fractures. With other indications (subtrochanteric fractures, osteotomies, etc.) it is still widely used.
Hip joint endoprostheses (both hemi and total endoprostheses) have been used since the beginning of their development not only for the treatment of coxarthrosis, but also for the definitive, primarily load-stable treatment of medial femoral neck fractures, especially in older people.
See also
literature
- V. Bühren, O. Trentz, U. Heim: Checklist traumatology . Thieme, 2005, ISBN 3-13-598106-1 .
- Pelvic ring and hip In: J. Duparc: Surgical techniques in orthopedics and traumatology. Elsevier, 2005, ISBN 3-437-22556-1 .
- AB Imhoff, R. Baumgartner: Checklist Orthopedics. Thieme, 2006, ISBN 3-13-142281-5 .
- R.-P. Meyer, A. Gächter: Hip surgery in practice. Springer, 2005, ISBN 3-540-22718-0 .
- S2e guidelines for femoral neck fractures in adults from the German Society for Trauma Surgery (DGU). In: AWMF online (as of 2008)
- S2e guideline for proximal femoral fractures in children of the German Society for Trauma Surgery (DGU). In: AWMF online (as of 2008)
Web links
Individual evidence
- ^ Herbert Lippert: Textbook Anatomie Elsevier, 2007, ISBN 978-3-437-42362-8 .
- ^ Volker Ewerbeck: Standard procedure in operative orthopedics and trauma surgery . Thieme, 2006, ISBN 3-13-100533-5 .
- ^ RG Cumming, RJ Klineberg: Fall frequency and characteristics and the risk of hip fractures. In: J. Am. Ger Soc. 42, (1994), pp. 774-778.
- ↑ a b C. J. Wirth: Orthopedics and orthopedic surgery. Band: pelvis / hip. Thieme, 2004, ISBN 3-13-126221-4 .
- ↑ misinterpretation of Pauwel's Classification. (No longer available online.) Bone and Joint, 2014, archived from the original on November 23, 2015 ; accessed in October 2015 . Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ↑ Arne Hillienhof, SB: Femoral neck fracture: New guideline prescribes fast surgery Deutsches Ärzteblatt 2019, Volume 116, Issue 49 of December 6, 2019, page A-2280, link accessed on December 15, 2019, 9:03 p.m. CEST
- ↑ J. Duparc: Surgical Techniques in Orthopedics and Traumatology. Pelvic ring and hip. Elsevier, 2005.
- ↑ AB Imhoff, R. Baumgartner: Checklist Orthopedics. Thieme, 2006.
- ↑ V. Bühren, O. Trentz, U. Home: Checklist traumatology. Thieme, 2005.
- ↑ Stefan Ocken: The bipolar dual head endoprosthesis for the therapy of femoral neck fractures. Result control and metric recording of the head position . Dissertation. Giessen University Hospital, 1999.
- ↑ F. Bonnaire, T. Lein, T. Hohaus: Prosthetic treatment of proximal femur fractures . In: trauma surgeon. 2005. Edition 108, pp. 387-400.
- ↑ R. Blomfeldt, H. Tornkvist, S. Ponzer: Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. In: Journal Bone and Joint Surgery. 2005. Edition 87, pp. 523-529.
- ↑ R.-P. Meyer, A. Gächter: Hip surgery in practice. Springer, 2005.
- ↑ HJ. Maurer, HJ. Teuber, M. Bier, I. Hermanns: Fracture line course - femoral head necrosis in the medial femoral neck fracture. In: Archives of Orthopedic and Trauma Surgery . 2004.
- ↑ Treatment of acute perioperative and post-traumatic pain . ( Memento of November 27, 2009 in the Internet Archive ) (PDF) AWMF guideline 041/001, 2007, pp. 219–228.
- ↑ Guideline Osteology: Osteoporosis of the Elderly . ( Memento from September 11, 2010 in the Internet Archive ) AWMF online
- ^ U. Kaack: The proximal femoral fracture of the elderly: Therapy concepts and results of a retrospective study. Dissertation. Bochum 2000, pp. 10-12, DNB 962764698/34 (PDF).