Right bundle branch block
| Classification according to ICD-10 | |
|---|---|
| I45.0 | Right fascicular block |
| I45.1 | Other and unspecified right bundle branch block Right bundle branch block onA |
| ICD-10 online (WHO version 2019) | |
As a right bundle branch block (abbreviated RSB or rare RBBB from English. Right bundle branch block ) is in the medicine a disorder of impulse conduction in the heart and also the present case results in electrocardiogram called (ECG).
The conduction disorder "right bundle branch block" does not cause any symptoms, but, like the left bundle branch block , can be an indication of a significant heart disease or other stress on the right main chamber. The causes of a right bundle branch block are circulatory disorders, inflammation of the heart or volume loading of the right ventricle, and rarely poisoning. Often, however, no cause can be determined. Special therapy is not required.
The ECG finding “right bundle branch block ” is characterized by changes in the QRS complex , which shows the activation of the ventricles in the ECG . These changes can occur in various forms. As a “complete right bundle branch block” they indicate a conduction disorder in the right tawara limb , which supplies the right ventricle as part of the conduction system. As an “incomplete right bundle branch block”, however, they can also be present in people with healthy hearts without any pathological significance.

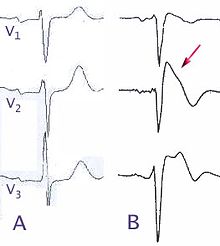
|
Right bundle branch block (ECG leads V 1–6 ) V 1 : QRS complex broadened (145 ms) V 6 : wide S-point (arrow) |
Emergence
The formation of a right bundle branch block can be explained using the anatomy of the conduction system and the physiology and pathophysiology of the conduction in the heart.
Excitation conduction system

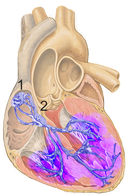
|
Excitation conduction system (schematic, in humans) 1 Sinus node |
The heart of mammals has specialized heart muscle cells that generate electrical impulses ( action potentials ) and pass them on within the heart via so-called gap junctions . These cells form the conduction system.
Below the secondary pacemaker, the so-called AV node , the part of the conduction system known as the bundle of His branches off into the right and left Tawara thighs. The left thigh is also divided into a rear and an anterior fiber bundle, the left posterior and left anterior fascicle.
From the so-called Purkinje fibers, the end branches of the Tawara thighs, the excitation then spreads into the muscles of the heart chambers (ventricles). The fibers of the right tawara thigh are mainly responsible for the muscles of the right ventricle and the fibers of the two fascicles of the left thigh are responsible for the left ventricle.
Normal excitation conduction
|
Normal excitation line (schematic) All heart muscle sections are excited almost simultaneously (purple color). |
Within the excitation conduction system, the conduction speed of about two meters per second (m / s) is so high that the average five to ten centimeters from the AV node to the tip of the human heart can be overcome within 25-50 milliseconds (ms). An exception is the AV node itself, which delays the conduction of excitation from the atria to the ventricles in order to guarantee a sufficient filling time of the chambers. The muscle cells on the inner wall of both heart chambers are almost simultaneously depolarized within a few milliseconds . From there, the excitation spreads to the remaining muscles of the ventricles at a speed of about one meter per second.
This type of excitation propagation with an intact excitation conduction system leads to a synchronous contraction of the muscles of the left and right heart chambers at the beginning of the expulsion phase ( systole ) of the heart.
Pathophysiology
With a complete right bundle branch block, the transmission of electrical impulses in the right tawara thigh is slowed down or completely blocked. As long as at least one fascicle of the left tawara thigh is still functioning, the excitation spreads from its terminal branches to the muscles of the right ventricle. Their muscle cells are then depolarized about 50 ms later than those in the left ventricle. This delay is due to the detour of the impulses via the left tawara thigh and the slower conduction of excitation in the working muscles (about 1 m / s) compared to the cells of the excitation conduction system (about 2 m / s).
causes
The possible causes of a right bundle branch block are many. They range from just lightly touching the ventricular septum during a cardiac catheter examination to serious heart diseases such as heart attacks or stress on the right heart in the case of lung diseases ( cor pulmonale ). It is observed in younger people in particular, even for no apparent cause. Complete right bundle branch block almost always has an organic cause. An incomplete RSB, on the other hand, can have other causes in addition to a slight conduction delay in the right tawara thigh and can also occur with normal excitation conduction.
Congenital causes
Congenital heart diseases such as atrial septal defect can cause RSB. In very rare cases the RSB can be traced back to a hereditary disease with an autosomal dominant inheritance, as it was found in a large Lebanese family. In her, a defect located on the long arm of chromosome 19 leads to various conduction disorders such as RSB, blockages in one of the left Tawara thighs or a complete AV block .
Also for arrhythmogenic right ventricular cardiomyopathy and Brugada syndrome , which are classified as “congenital primary cardiomyopathies ”, the accumulation of RSB in families is characteristic. Life-threatening cardiac arrhythmias often occur in these rare congenital heart muscle diseases .
Acquired causes
RSB are most common in elderly patients with coronary artery disease . Primary heart muscle diseases ( cardiomyopathy ) and acute or chronic stress on the right heart due to lung diseases (acute and chronic cor pulmonale ) are also frequent causes. In the case of a pulmonary embolism , a right bundle branch block indicates an acute cor pulmonale ; in the case of chronic obstructive pulmonary disease or pulmonary fibrosis , it is an indication of a chronic cor pulmonale .
Inflammation of the heart muscle ( myocarditis ) or inflammatory changes in the coronary arteries in periarteritis nodosa or endangiitis obliterans are rare causes. Also under other inflammation an RSB can occur familiar example are conduction disturbances at a heart muscle inflammation in the context of disease ( disease Lyme ).
Even with valvular right bundle branch block images can occur well after surgical interventions on the heart when the right ventricle was opened. This is particularly common after defects in the ventricular septum ( ventricular septal defect ) have closed and can also regress in the years after the operation.
Other possible causes are poisoning ( intoxication ) and electrolyte disturbances . RSB has been described in the case of lead and arsenic poisoning , and a number of drugs such as beta blockers , tricyclic antidepressants , diphenhydramine , chloroquine and digitalis preparations are also possible. Excessive levels of potassium in the blood ( hyperkalemia ) can also cause right bundle branch block .
Diagnostic criteria and nomenclature
The criteria for diagnosing right bundle branch block are nowhere stipulated. The definitions used today are based on the duration or width and certain features of the QRS complex in the ECG. The information for the upper limit of the normal QRS duration in humans fluctuates in the literature between 100 and 120 ms, the most frequently mentioned limit value is 120 ms. The so-called "upper transition point" (OUP) or "beginning of the greatest negativity movement" (GNB) is more than 30 ms after the start of the QRS complex.
The diagnosis of right bundle branch block in humans is made regardless of age or gender, although the duration of the QRS complex varies depending on these characteristics. The mean QRS duration in children in the second and third year of life is 56 ms, between 12-15 years 65 ms, in women over 49 years 87 ms and in men between 18 and 29 years 96 ms.
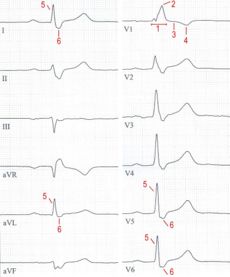
Complete right bundle branch block
A “complete right bundle branch block” or “complete right bundle branch block” is commonly spoken of when in humans
- the duration of the QRS complex is at least 120 ms and
- in leads V 1 and V 2 wide, notched R-serrations as well
- Broad, deep S-waves can be detected in leads V 5 and V 6 .
For animals, other limit values for the QRS duration must be taken into account (see veterinary aspects ).
Incomplete right bundle branch block
If the QRS complex lasts less than 120 ms in an otherwise typical form, the term “incomplete right bundle branch block” is often used, and more rarely “incomplete” or “partial right bundle branch block”. Some authors limit this diagnosis to patients with a QRS duration between 100 and 119 ms and prefer the designation "indicated right bundle branch block", "right delay" or "right delay curve" for a shorter QRS duration. These forms of right bundle branch block, however, are not uniformly defined and are also observed in people with normal conduction. The percentile P 98 , which only two percent of those examined exceeded, is 114 ms for men with healthy heart aged 18 to 29 years.
Wilson block
The term "Wilson block" has historical roots and is no longer common today. In the German-speaking countries in particular, it was used until the 1970s for the shape of the bundle branch block , which Wilson initially described in 1934 as the unusual type in right bundle-branch block , as opposed to the Bayley block . It corresponds to the current definition of “normal” right bundle branch block, a synonym is “right bundle branch block of the common type”.
Bayley's block or classic right bundle branch block
The terms “classic right bundle branch block” or “Bayley block”, which were particularly used in the German-language literature of the 1960s, are no longer in use. They were used to describe a mirror image of the left bundle branch block with deep, wide and often splintered S-waves in lead I and consequently a right-hand type or over-twisted right-hand type of the electrical heart axis . Since the 1970s it has been assumed that this block picture is caused by a combination of an RSB and a blockage in the posterior fascicle of the left tawara thigh ( left posterior hemiblock or LPH). Today this combination is called the bifascicular block .
Other forms
An only temporary right bundle branch block, in which the ECG is normalized again after elimination of a lead-delaying cause, is called “temporary” or “temporary right bundle branch block”. This phenomenon can be observed after heart muscle inflammation, prolonged tachycardia, or hyperkalemia. When there is a spontaneous change between RSB and normal conduction, the term “intermittent right bundle branch block” is common. The rare change between right and left bundle branch block is referred to as “bilateral” or “alternating bundle branch block”.
diagnosis
Experienced doctors may occasionally “hear” a right bundle branch block during auscultation as part of the physical exam. Due to the delayed contraction of the right ventricle, the splitting of the first heart sound is clearer and the splitting of the second heart sound, which is particularly pronounced during inhalation ( inspiration ), is emphasized by the later closure of the pulmonary valve . However, these findings are ambiguous; a reliable diagnosis is only possible with the help of the electrocardiogram (ECG).
|
Right bundle branch block (electrocardiogram) 1 QRS widened |
electrocardiogram
Due to the delayed excitation of the right ventricle, the QRS complex is abnormally shaped and broadened, especially in the EKG leads above the right heart (V 1–3 ). The upper transition point (OUP) is there more than 30 ms after the start of the QRS complex and is therefore delayed. The most common forms of the QRS complex are described as M-shaped, rsr 'configuration, rsR' configuration, rR 'configuration or RsR' configuration, more rarely also as qR configuration. In the leads with the most pronounced delay of the upper transition point, the ST segment is often sloping (descending) and the T wave is negative.
The complete RSB is characterized by slim and high R-waves and broad, clumsy S-waves in leads I, aVL and V 5-6 with a normal position of the electrical heart axis.
| Examples of the shape of the QRS complex in lead V 1 at RSB (schematic) | ||||
Differential diagnosis
As a rule, the EKG findings of a right bundle branch block are clear. It has a QRS duration of more than 120 ms in common with the left bundle branch block (LSB), but it differs significantly from it in the derivation with the greatest delay of the upper transition point. With the RSB it is the lead V 1 or rarely V 2 , with the LSB one of the left-facing leads (I, aVL, V5 or V6).
A strongly widened QRS complex that fulfills both the RSB and the LSB criteria is rarely observed, and only when the heart muscle is severely damaged. This prognostically unfavorable finding is called branching or arborization block or "diffuse intraventricular conduction disorder".
Particularly in younger patients who have had syncope or who have blood relatives who have syncope under the age of 45, it is important to look out for evidence of Brugada syndrome or arrhythmogenic right ventricular cardiomyopathy (ARCM) in right bundle branch block images. A tent-shaped or arched ST segment elevation in more than one of leads V 1-3 makes Brugada syndrome probable and requires further differentiated therapy. Negative T waves in the chest wall leads (often V 2–4 ) and extrasystoles with a right bundle branch block-like appearance indicate ARCM.
The distinction between an isolated right bundle branch block and a bifascicular block, i.e. a combination of RSB and left posterior (LPH) or left anterior hemiblock (LAH), is mainly done by analyzing the electrical axis of the heart . It is normal with the RSB and shifted to the left with the combination RSB + LAH. The LAH can be considered secured with a QRS axis <−45 °. With the combination of RSB + LPH, which was previously called “classic right bundle branch block”, the QRS axis is shifted to the right (secured at> + 120 °).
therapy
A right bundle branch block without recognizable heart disease does not require any therapy .
With a right bundle branch block it is basically possible to normalize the temporal sequence of ventricular excitation with the help of a biventricular pacemaker ("three-chamber pacemaker ") , but only a few patients with RSB were included in the studies on this treatment, known as cardiac resynchronization therapy (CRT). so the benefit is not well documented. In severe heart failure and a QRS duration of more than 120 ms, the CRT can be used if the two chambers of the heart show a pronounced asynchronous movement pattern during the ultrasound examination of the heart ( echocardiography ).
In the case of a pure right bundle branch block , the risk of a complete AV block due to progression of the conduction disturbance to the left tawara thigh is low. In combination with a blockage in one of the left fascicles (left anterior or left posterior hemiblock), on the other hand, the probability of a complete AV block and the risk of mortality are increased, especially in older people. For this reason, prophylactic pacemaker implantation is considered if there are blockages in the left tawara thigh . It comes into question when switching between left and right bundle branch block, with additional frequent AV blockages and with syncope that has already been suffered .
statistics
Epidemiology
In people without an identifiable heart disease, the proportion of ECG with right bundle branch block is around 0.12 to 0.18%. The ECG of patients admitted to hospital showed right bundle branch block in 3.6%, and in patients aged 90 and over even in 13% of women and 7% of men.
Overall, right bundle branch block is about as common as left bundle branch block. In contrast to the right bundle branch block, the left bundle branch block is often the result of an organic heart disease.
forecast
Dependencies of the forecast
The prognosis of people with right bundle branch block depends on whether they also have an identifiable heart disease. The prospects are good for people with healthy hearts. Since in a study by the Royal Canadian Air Force on almost 140,000 young men no adverse effects of right bundle branch block were found in the 168 people affected, they have also been accepted as pilots there since 1953. These results were confirmed again in 1996 on the basis of examinations in a total of 110,000 people without recognizable or suspected heart disease. While people with a left bundle branch block suffered significantly more often from coronary artery disease and died from heart disease than those without a bundle branch block, this was not the case for people with a right bundle branch block. Another study from the USA showed a trend towards a slightly increased mortality after an average of 7.7 years in people with an incidentally discovered right bundle branch block without any other signs of heart disease compared to people without a bundle branch block, but this was not statistically significant ( relative risk 1.18; confidence interval 0.85–1.65, p = 0.32).
In patients with diseases of the heart or other organs, however, an EKG with a right bundle branch block indicates a worse prognosis than a normal EKG. The annual mortality rate of patients with right bundle branch block at the Palo Alto Veterans Affairs Medical Center was 3.6%, significantly higher than that of patients with a normal ECG (0.5%).
For coronary heart disease
An isolated right bundle branch block has no prognostic significance in patients who are only suspected of having coronary artery disease . The combination of RSB and left anterior hemiblock (LAH), on the other hand, was associated with a more than three-fold higher mortality after about 3.5 years in this patient group.
In patients with acute chest pain, right bundle branch block has been shown to be an independent risk factor for mortality in the following seven days, and it is particularly important in the case of a heart attack . It is found in a good 10% of all heart attack patients and is associated with a significantly more frequent occurrence of heart attack complications. Heart failure is almost twice as common, and AV blocks requiring a pacemaker are even three times more common. In one study, mortality within one year in patients with an RSB was significantly increased at 40.7% compared to 17.6%. Especially in newly emerged RSB that do not resolve, the 30-day mortality rate is 76%.
Veterinary medicine
relevance
In veterinary medicine , right bundle branch block is only of clinical significance in dogs , cats and horses , although the corresponding ECG findings in horses are not diagnostically reliable, as hypertrophy of the heart chambers can be similar. The change is sometimes seen as an incidental finding in healthy dogs and cats. In cats , the picture may appear as a result of hyperkalemia when the urethra is occluded. Other possible causes include ventricular septal defect , tumor diseases of the heart (especially metastatic hemangiosarcoma (dog), lymphosarcoma (cat) and mammary gland tumors (both)), cardiomyopathies, injuries, heartworm infestation , of previous cardiac arrest and chronic Trypanosoma cruzi infections ( Chagas disease ). In the Beagle , a - usually incomplete - right bundle branch block can be the result of a genetic change in the wall thickness of the right ventricle. An enlargement of the right ventricle must be excluded from the differential diagnosis. Although a right bundle branch block usually does not need to be treated with medication, it can be a sign of an underlying heart disease that needs treatment.
EKG changes
In dogs, the duration of the QRS complex in RSB is more than 80 ms (or 70 ms in dwarf breeds), in cats it is more than 60 ms. The electrical axis of the heart is usually shifted to the right. The QRS complex is positive in the leads aVR, aVL and CV 5 RL (rV 2 ) and has a broad, often M-shaped RSR or rSR shape in this lead. In V 10 it is often W-shaped. In II it is negative. The S-wave is enlarged and broadened in leads I, II, III, aVF, CV 6 LL (V 2–3 ) and CV 6 LU (V 4–6 ). If the described changes occur with a normal or slightly increased duration of the QRS complex, an incomplete right bundle branch block is suspected. In the differential diagnosis, the presence of ventricular extrasystoles must be ruled out, especially in the case of deviations from the normal sinus rhythm - for example due to atrial fibrillation - since the therapeutic consequences (e.g. administration of cardiac glycosides ) contradict each other .
history
The history of the term right bundle branch block as an EKG diagnosis began in the early 20th century. As part of his pioneering work on the introduction of electrocardiography, the Dutch physiologist and later Nobel Prize winner Willem Einthoven described in 1906 and 1910 not only the normal EKG but also widened QRS complexes and attributed them to disturbances in the conduction of excitation. In 1917 the Viennese Carl Rothberger and Heinrich Winterberg presented test results in the "Journal for the Entire Experimental Medicine" which allowed a distinction between left and right bundle branch block on the basis of the EKG. Under the title "Experimental Contributions to the Knowledge of Conduction Disorders in the Chambers of the Mammalian Heart" they published their knowledge, obtained with the string galvanometer developed by Einthoven , that the QRS complex resembles an extrasystole from the left ventricle after severing the right Tawara branch temporarily assumes such a shape when pressure is applied to the right thigh.
The descriptions of right bundle branch block that are common today were essentially developed in the 1930s and significantly influenced by the American cardiologist Frank Norman Wilson . In practice, even in the early 30's only two kinds of bundle branch block different from the shape of the QRS complexes: frequent ( common type ) and a rare type ( rare type ). In 1932 Wilson succeeded in identifying the common type as left bundle branch block and the rare type as right bundle branch block . From 1934 onwards, the common and rare types used until then were increasingly abandoned after Wilson had found that their frequency was by no means as different as previously assumed.
Also in 1934 he described the typical form of the QRS complexes in bifascicular block and attributed it to a blockage of the right Tawara thigh and an unknown additional factor, since it was included in the chest wall leads named after him ("Wilson leads") in dogs had observed ECG findings comparable to an experimentally generated block.
In the 1950s, Braunwald and his colleagues were able to use the simultaneous recording of ECG and pressure curves from the right ventricle to prove that a right bundle branch block actually leads to a contraction of the right ventricle that is about 0.05 seconds late.
At the beginning of the 1970s it was shown that an incomplete right bundle branch block in dogs is more often due to a presumably genetic thickening of the right ventricular heart muscle than to a conduction delay in the right tawara thigh, which led to a partial reassessment of the incomplete block diagram.
In the 1990s, a special form of right bundle branch block was delineated as an independent disease that poses a significant risk of sudden cardiac death for affected patients . It is now usually referred to as Brugada syndrome after its first description and has been classified as a cardiomyopathy since 2006.
literature
- D. Kalusche, G. Csapo: Conventional and intracardiac electrocardiography . 3. Edition. Novartis Pharma GmbH, 1997, ISBN 3-933185-05-X .
- DM Mirvis, AL Goldberger In: DP Zipes et al. (Ed.): Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine . 7th edition. WB Saunders Company, Philadelphia 2004, ISBN 1-4160-0014-3 , pp. 114-128.
Web links
- Color-coded computer simulation of the propagation of excitation in RSB (format MOV, "movie 3") at The Visible Human Project of the National Library of Medicine
Individual evidence
- ^ H. Antoni: Functions of the heart . In: RF Schmidt, G. Thews: Physiology of humans . 23rd edition. Springer-Verlag, 1987, ISBN 3-540-16685-8 , p. 264.
- ^ A b c A. L. Goldberger: Electrocardiography . In: DL Kasper et al .: Harrison's Principles of Internal Medicine . 16th edition. Mcgraw-Hill Professional, 2004, ISBN 0-07-139140-1 .
- ↑ E. Stéphan, A. de Meeus, P. Bouvagnet: Hereditary bundle branch defect: right bundle branch blocks of different causes have different morphologic characteristics. In: American Heart Journal . Volume 133, Number 2, February 1997, pp. 249-256, ISSN 0002-8703 . PMID 9023172 . Pp. 249-256.
- ^ A b c E. Nusser, G. Trieb, A. Weidner: Differentialdiagnostik des EKG . 2nd Edition. FK Schattauer Verlag, 1982, ISBN 3-7945-0822-X , p. 146.
- ↑ M. Stille-Siegener, H. Eiffert, S. Vonhof: Cardiac and neurological manifestations of Lyme borreliosis in congenital AV block of the 1st degree . In: German Medical Weekly . Volume 121, Number 42, October 1996, pp. 1292-1296, ISSN 0012-0472 . doi : 10.1055 / s-2008-1043142 . PMID 8964203 . Pp. 1292-1296.
- ↑ U. Schilling, R. Mück, E. Heidemann: Lead poisoning after ingestion of ayurvedic drugs. In: Medical Clinic . Volume 99, Number 8, August 2004, pp. 476-480, ISSN 0723-5003 . doi : 10.1007 / s00063-004-1072-2 . PMID 15309279 .
- ^ SA Ahmad et al .: Electrocardiographic abnormalities among arsenic-exposed persons through groundwater in Bangladesh. In: Journal of health, population, and nutrition. Volume 24, Number 2, June 2006, pp. 221-227, ISSN 1606-0997 . PMID 17195563 .
- ↑ JA Wagner et al .: Resuscitation and protracted cardiac depression after suicidal metoprolol / ramipril intoxication. In: Intensive Care Medicine and Emergency Medicine. 43, 2006, pp. 50-54, doi : 10.1007 / s00390-006-0651-z .
- ↑ HK Thanacoody, SH Thomas: Tricyclic antidepressant poisoning: cardiovascular toxicity. In: Toxicological Reviews . Volume 24, Number 3, 2005, pp. 205-214, ISSN 1176-2551 . PMID 16390222 .
- ^ AC Thakur: QT interval prolongation in diphenhydramine toxicity. In: International Journal of Cardiology . Volume 98, Number 2, February 2005, pp. 341-343, ISSN 0167-5273 . doi : 10.1016 / j.ijcard.2003.10.051 . PMID 15686790 .
- ↑ JP Baguet, F. Tremel, M. Fabre: Chloroquine cardiomyopathy with conduction disorders. In: Heart . Volume 81, Number 2, February 1999, pp. 221-223, ISSN 1355-6037 . PMID 9922366 . PMC 1728937 (free full text). (Review).
- ↑ PK Moulik, C. Nethaji, AA Khaleeli: Misleading electrocardiographic results in patient with hyperkalaemia and diabetic ketoacidosis. In: BMJ (Clinical research ed.). Volume 325, Number 7376, December 2002, pp. 1346-1347, ISSN 1756-1833 . PMID 12468487 . PMC 1124804 (free full text).
- ↑ a b C. Lentner (Ed.): Geigy Scientific Tables. Vol. 5: Heart and Circulation . CIBA-GEIGY Corporation, 1990, ISBN 0-914168-54-1 .
- ^ AT Mauric, NJ Samani, DP de Bono: When should we diagnose incomplete right bundle branch block? In: European Heart Journal . Volume 14, Number 5, May 1993, pp. 602-606, ISSN 0195-668X . PMID 8508853 .
- ↑ a b c F. A. Schaub: Outline of clinical electrocardiography . Ed .: Ciba-Geigy AG. Documenta Geigy. Supplementum I. Basel 1965, pp. 46-47.
- ↑ Csapo G: Conventional and intracardiac electrocardiography . 1982, p. 288. Werk-Verlag Dr. Edmund Banaschewski .
- ^ FR Eberli: Differential diagnostic significance of the heart sounds . In W. Siegenthaler (Ed.): Siegenthaler's differential diagnosis 19th edition. Georg Thieme Verlag, 2005, ISBN 3-13-344819-6 , pp. 623-624.
- ^ D. Corrado, et al .: Right bundle branch block, right precordial st-segment elevation, and sudden death in young people. In: Circulation . Volume 103, Number 5, February 2001, pp. 710-717, ISSN 1524-4539 . PMID 11156883 .
- ^ FR Eberli: Arrhythmogenic right ventricular cardiomyopathy . In: W. Siegenthaler (Ed.): Siegenthalers Differentialdiagnose. 19th edition. Georg Thieme Verlag, 2005, ISBN 3-13-344819-6 , p. 682.
- ↑ a b B. Lemke, B. Nowak, D. Pfeiffer: Guidelines for pacemaker therapy . In: Journal of Cardiology . Volume 94, Number 10, October 2005, pp. 704-720, ISSN 0300-5860 . doi : 10.1007 / s00392-005-0269-3 . PMID 16200488 .
- ↑ M. Lerecouvreux et al .: Right bundle branch block: electrocardiographic and prognostic features . Archives des maladies du coeur et des vaisseaux. Volume 98, Number 12, December 2005, pp. 1232-1238, ISSN 0003-9683 . PMID 16435603 .
- ↑ AE Tammaro, G. Forin: Incidence and outcome of fascicular blocks in the aged. Retrospective studies . In: Giornale italiano di cardiologia. Volume 6, Number 6, 1976, pp. 1140-1141, ISSN 0046-5968 . PMID 1022615 .
- ^ A b G. W. Manning: An historical review of the electrocardiogram of right bundle branch block in the Royal Canadian Air Force. In: The Canadian journal of cardiology. Volume 3, Number 8, 1987 Nov-Dec, pp. 375-377, ISSN 0828-282X . PMID 3427534 .
- ↑ a b G. J. Fahy et al .: Natural history of isolated bundle branch block. In: The American journal of cardiology. Volume 77, Number 14, June 1996, pp. 1185-1190, ISSN 0002-9149 . PMID 8651093 .
- ↑ a b A. D. Desai et al .: Prognostic Significance of Quantitative QRS Duration. In: The American journal of medicine. Volume 119, Number 7, July 2006, pp. 600-606, ISSN 1555-7162 . doi : 10.1016 / j.amjmed.2005.08.028 . PMID 16828632 . ( online (PDF; 260 kB) , accessed on February 11, 2007.)
- ↑ GP Kelley et al .: Electrocardiographic findings in 888 patients> or = 90 years of age. In: The American journal of cardiology. Volume 98, Number 11, December 2006, pp. 1512-1514, ISSN 0002-9149 . doi : 10.1016 / j.amjcard.2006.06.055 . PMID 17126661 .
- ↑ a b W. L. Miller et al .: Risk factor implications of incidentally discovered uncomplicated bundle branch block. In: Mayo Clinic proceedings. Mayo Clinic. Volume 80, Number 12, December 2005, pp. 1585-1590, ISSN 0025-6196 . doi : 10.4065 / 80.12.1585 . PMID 16342651 . ( online )
- ↑ L. Cortigiani et al .: Prognostic implications of intraventricular conduction defects in patients undergoing stress echocardiography for suspected coronary artery disease. In: The American journal of medicine. Volume 115, Number 1, July 2003, pp. 12-18, ISSN 0002-9343 . PMID 12867229 .
- ↑ KM Nielsen et al .: How can we identify low- and high-risk patients among unselected patients with possible acute coronary syndrome? In: The American journal of emergency medicine. Volume 25, Number 1, January 2007, pp. 23-31, ISSN 0735-6757 . doi : 10.1016 / j.ajem.2006.06.003 . PMID 17157678 .
- ^ A. Melgarejo-Moreno et al .: Incidence, clinical characteristics, and prognostic significance of right bundle-branch block in acute myocardial infarction: a study in the thrombolytic era. In: Circulation. Volume 96, Number 4, August 1997, pp. 1139-1144, ISSN 0009-7322 . PMID 9286941 .
- ↑ O. Dietz, B. Huskamp: Handbuch Pferdepraxis . 2nd Edition. Enke, Stuttgart 1999, ISBN 3-432-29262-7 , p. 295.
- ↑ MS Miller et al .: Electrocardiography . In: PR Fox, D. Sisson, NS Moise: Textbook of Canine and Feline Cardiology: Principles and clinical Practice. Second edition. Saunders, Philadelphia 1999, ISBN 0-7216-4044-3 , pp. 84-85.
- ^ LP Tilley: ECG in dogs and cats. Basics, evaluation and therapy. 1st edition. Schlütersche Verlagsanstalt, Hanover 1989, ISBN 3-87706-096-X , pp. 76–77, 112–113.
- ^ SJ Ettinger et al .: Electrocardiography. In: SJ Ettinger, EC Feldman: Textbook of Veterinary Internal Medicine. Fifth edition. Saunders, Philadelphia 2000, ISBN 0-7216-7257-4 , pp. 817-818.
- ^ Carl J. Wiggers : Willem Einthoven (1860-1927) Some Facets of His Life and Work . In: Circ Res . (1961) 9, ISSN 0009-7330 , pp. 225-234.
- ^ RD Pruitt: Experimental Bundle-Branch Block Fifty Years Ago . In: Circulation. (1967) 36, ISSN 0009-7322 , pp. 625-627.
- ^ FN Wilson, AG Macleod, PS Barker: The order of ventricular excitation in human bundle-branch block. In: American Heart Journal. 7, 1932, pp. 305-330, doi : 10.1016 / S0002-8703 (32) 90346-9 .
- ^ FN Wilson, et al .: The significance of electrocardiograms characterized by an abnormally long QRS interval and by broad S-deflections in lead I. In: American Heart Journal. 9, 1934, pp. 459-471, doi : 10.1016 / S0002-8703 (34) 90094-6 .
- ^ FN Wilson, FD Johnston, PS Barker PS: Electrocardiograms of an unusual type in right bundle-branch block. In: American Heart Journal. 9, 1934, pp. 472-479, doi : 10.1016 / S0002-8703 (34) 90095-8 .
- ^ E. Braunwald et al .: Right bundle-branch block, hemodynamic, vectorcardiographic and electrocardiographic observations. In: Circulation. Volume 13, Number 6, June 1956, pp. 866-872, ISSN 0009-7322 . PMID 13356442 .
- ↑ EN Moore, JP Boineau, DF Patterson: Incomplete right bundle-branch block. An electrocardiographic enigma and possible misnomer. In: Circulation. Volume 44, Number 4, October 1971, pp. 678-687, ISSN 0009-7322 . PMID 4255293 .
- ^ GK Massing, TN James: Conduction and block in the right bundle branch, real and imagined. In: Circulation. Volume 45, Number 1, January 1972, pp. 1-3, ISSN 0009-7322 . PMID 4257021 .
- ^ P. Brugada, J. Brugada: Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. In: Journal of the American College of Cardiology . Volume 20, Number 6, November 1992, pp. 1391-1396, ISSN 0735-1097 . PMID 1309182 .