Hyperglycemia
| Classification according to ICD-10 | |
|---|---|
| R73 | Elevated blood glucose |
| ICD-10 online (WHO version 2019) | |
Hyperglycemia ( Greek ὑπέρ hyper 'over' and Greek γλυκύς glykys 'sweet' and Greek αἷμα haima 'blood', coll. Also excessive sugar ) is a pathologically increased amount of glucose in the blood ( blood sugar ). Acute hyperglycaemia shows up in the glucose level, and long-term hyperglycaemia shows up in the HbA1c level of the blood.
Hyperglycemia is the main symptom of diabetes mellitus (diabetes), in which the necessary regulation of the nutrient glucose is disturbed, so that from a level of around 200 mg / dl, the so-called kidney threshold , it is also excreted in the urine. The symptoms that occur in hyperglycemia range from a feeling of thirst and dry mouth to increased urine output (polyuria) and visual disturbances to, if left untreated, fatal hyperglycemic coma . In the long term, hyperglycemia is a major contributor to the classic consequences of sugar disease such as stroke , loss of vision or kidney weakness . Their treatment consists in regulating the glucose level in the blood by means of suitable measures, such as the administration of insulin .
The term hyperglycemia was defined differently. Until the end of the 19th century, medicine assumed that any occurrence of sugar in the blood must be regarded as pathological. In 1885 it was recognized that sugar also occurs in the blood of healthy people and that increased urine excretion is a sign of illness only at a value of around 210 to 260 mg / dl . According to today's definition, the blood sugar level in healthy individuals does not exceed 100 mg / dl on an empty stomach and, according to a sugar stress test (oGTT), does not exceed 140 mg / dl. In people with diabetes it is over 125 mg / dl on an empty stomach and over 200 mg / dl in oGTT. The “gray area” in between is also known as intermediate hyperglycaemia and statistically carries an increased risk of developing diabetes mellitus.
Occurrence
The blood sugar level in healthy individuals should be below 100 mg / dl on an empty stomach (i.e. at least 8 hours after the last calorie intake) and below 140 mg / dl after a sugar stress test. When the body ingests food, glucose and other sugars , with a few exceptions, are absorbed through the intestine and conveyed to the liver via the portal vein circulation ( enterohepatic circulation ) before they enter the blood . Through various regulatory mechanisms, the blood sugar level in healthy people is kept constant at around 70 to 80 mg / dl for a long time. If the glucose level in the enterohepatic circulation rises as a result of a carbohydrate-rich diet, the beta cells of the pancreas are stimulated to secrete the blood sugar-lowering hormone insulin in order to keep the glucose level in the blood constant. If this regulation fails or if the insulin loses its effectiveness, short- or long-term hyperglycaemia occurs.
Hyperglycemia is the main symptom of diabetes mellitus, but it is not a reliable criterion for this. Even a Cushing's disease (elevated cortisol levels ), a acromegaly (increased growth hormone levels ), a pheochromocytoma (increased levels of epinephrine and norepinephrine ), a hyperthyroidism (for example, due to Graves' disease ), iron deposits in the pancreatic beta cells ( hemochromatosis can) and drugs trigger them. It can also occur with infections , after a heart attack , stroke or anesthesia . In females , it may due to high progesterone levels in the Zwischenbrunst cause a rise in blood sugar in the blood, in cats stress can trigger a prolonged hyperglycemia.
Emergence
There are various reasons why the body cannot stabilize the blood sugar level in the physiological range. The most common causes of an increase in blood sugar level are a reduced response of sugar-storing cells such as fat and muscle cells to insulin ( insulin resistance ) due to overconsumption of carbohydrates and sugar or a decreased insulin secretion by the pancreas. In the former case, the insulin release can even be increased. Therefore, advises the World Health Organization for sugar control in order to achieve a significant decline in sugar consumption so that fewer people overweight , obesity and diabetes are suffering.
The level of growth hormone ( somatropin ) in healthy people is only increased when the insulin level is too low. It increases the blood sugar level by inhibiting the absorption of sugar in fat and muscle cells, as well as reducing sugar consumption by increasing the supply of fats ( fatty acid oxidation ), especially in muscles. If both hormones are increased, hyperglycaemia can occur because the blood sugar-lowering effect of insulin on the sugar-storing cells is then restricted.
Cortisol increases blood sugar levels. In particular, it stimulates the formation of new sugar in the body and at the same time reduces sugar consumption . Therefore it counteracts the blood sugar lowering insulin. If there is an excess of cortisol ( Cushing's syndrome , stress), the blood sugar level rises.
At the same time, adrenaline and noradrenaline lead to increased formation and release of glucose as well as an inhibition of insulin release. Elevated levels, such as those found in pheochromocytoma , lead to hyperglycaemia.
In the case of an overactive thyroid , glycogenolysis and gluconeogenesis are stimulated; in hemochromatosis , the increased iron level in the pancreas leads to siderosis and fibrosis , which also affects the function of the insulin-forming beta cells . When glucagonoma increased causes glucagon an increase in gluconeogenesis with a simultaneous decrease of glycogenolysis and glucose consumption.
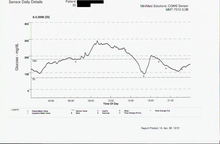
Serious illnesses such as myocardial infarction , severe infections or trauma , like anesthesia, can cause hyperglycaemia. The cause is the post-aggressive metabolism triggered by this , which leads to peripheral insulin resistance , whereby the administration of insulin does not lead to a sufficient lowering of the blood sugar level. A special case of morning hyperglycaemia while insulin therapy is ongoing are: The Somogyi effect , in which, for example, excessive evening insulin administration leads to nighttime hypoglycaemia and subsequent reactive hyperglycaemia. The dawn phenomenon is the hyperglycemia that occurs when the increased need for insulin in the second half of the night is not compensated for due to the increased GH excretion at this time , for example due to the nocturnal drop in the effectiveness of a delayed insulin after a single dose in the morning.
Clinical manifestations

The symptoms of hyperglycemia depend on the extent and duration of the high blood sugar level. A typical combination of symptoms that leads to the suspicion of hyperglycaemia (and thus diabetes mellitus) as the cause is frequent urination of large amounts of urine and, at the same time, increased feeling of thirst despite large amounts of water being consumed. In addition, there are not infrequently unspecific clinical signs such as dehydration , weakness, dizziness , visual disturbances, abdominal pain , nausea , vomiting , weakened muscle reflexes , dry mouth and dry skin. In severe cases that lead to hyperglycemic coma , the patients are then increasingly unconscious and, if left untreated, can also die from it.
Acute short-term hyperglycaemia can, for example, be recorded by means of a sugar load test, but do not cause any typical clinical symptoms as long as they do not exceed the kidney threshold (about 180 to 200 mg / dl ). Their clinical significance, especially with regard to the development of consequential damage , depends on their frequency and duration and can be estimated using the HbA1c . If the kidney threshold is exceeded, there is an increased urine excretion , in particular due to the water-binding property of sugar and the associated reduction in water reabsorption from the primary urine in the kidneys . The resulting increasing dehydration of the body is responsible for the feeling of thirst . Can prepare the amount does not adequately replace fluid loss, so it comes to dehydration . If this development of the disease is not recognized and treated, the result is a clouding of consciousness up to hyperosmolar coma , especially with very high blood sugar values (> 600 mg / dl) for days . Overall, there is a relative insulin deficiency in hyperosmolar coma, so that not infrequently too little insulin is available to adequately inhibit lipolysis. The formation of ketone bodies results in metabolic acidosis , which is usually relatively moderate , i.e. hyperacidity of the blood. A second form of clouding of consciousness associated with hyperglycaemia is the ketoacidotic coma , in which the blood sugar level can be significantly lower than in the hyperosmolar coma. However, it is less the dehydration than the complete lack of insulin as the cause of a generally much more pronounced acidosis than in hyperosmolar coma. The acidosis arises from lipolysis that is uninhibited due to a lack of insulin and the associated ketone body formation. The hyperosmolar coma is more likely to occur in type II diabetes (still existing insulin production) and the ketoacidotic coma is more likely to occur in type I diabetes (lack of insulin). In the latter, hyperglycemia can be seen as an accompanying symptom, but not as a causal condition as in the case of hyperosmolar.
In acute cases, visual disturbances caused by fluctuations in the blood sugar level are attributed less to diabetic retinopathy than to changes in the water content of the lens and vitreous humor . Abdominal pain can also accompany hyperglycaemia and then even resemble an acute abdomen . The cause in these cases is diabetic pseudoperitonitis , triggered by hyperperistalsis of the gastrointestinal tract as a result of acidosis. The weakening of the muscle reflexes (for example the patellar tendon reflex ) in connection with hyperglycemia are seen as the first sign of diabetic polyneuropathy , but acidosis as such leads to a decrease in the speed of contraction of the muscles regardless of the blood sugar level .
Long-term hyperglycemia leads to uncontrolled accumulation of sugar on proteins ( endogenous glycation ), which creates glycoproteins , so-called AGEs ( advanced glycation endproducts ). Clinically, these are of particular importance. In diagnostics, HbA1c is used as the glycoprotein of hemoglobin. In particular, damage to the basement membrane is significant. Due to the deposits of the AGEs there, it changes its properties. As a result, it becomes larger-pored and loses negative charge carriers. A microangiopathy develops. For example, their electrostatic and mechanical filter properties also change in the kidneys, making them permeable to proteins such as albumin and, as a result, proteins in the urine and, as the disease progresses, kidney failure . Diabetic retinopathy , neuropathy and peripheral macroangiopathy are considered to be further sequelae of microangiopathy . This uncontrolled accumulation of sugar also affects the cell membrane of the red blood cells, as well as other lipo- and seroproteins.
Investigation methods
The blood sugar is usually measured using capillary or venous blood. A measurement of the sugar content of the urine can also provide information ( kidney threshold ). The device usually indicates the level of blood sugar in the unit mg / dl (milligrams per deciliter), but in rare cases it can also be given in mmol / l ( millimoles per liter), with 1,000 mg / dl then about 0 .05549 mol / l.
In addition to a precise quantitative analysis laboratory tests (for example, by means of the reduction method according to Hagedorn-Jensen ) a rule, are in particular in emergency situations but also reliable for self-regulation possible detections of the magnitude of hyperglycemia important (semi-quantitative analysis). Rapid tests are suitable for this, in which the blood is applied to a test strip and causes discoloration there. This discoloration is then read out optically using a blood glucose meter . There are also test strips that allow a meaningful assessment without tools, i.e. with the naked eye. Microorganisms in urine and red blood cells in blood typically consume glucose. As a result, readings from samples that have been improperly stored for a long time can show falsely low values.
The determination of the glycohemoglobin HbA 1c from the venous blood is suitable for assessing the long-term course of the blood sugar level . It is based on the fact that, depending on the level of sugar in the blood, more or less sugar binds to the hemoglobin ( glycation ). The HbA 1c level shows the average sugar level for the past 6 to 8 weeks. Phases of hypoglycaemia and hyperglycaemia, which alternate with one another, can even result in normal HbA 1c levels in this way and thus falsely lead to normal blood sugar values.
pathology
- Depiction of the basement membrane
Image of the basement membrane and the basal lamina that can only be visualized with an electron microscope
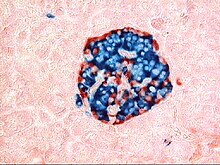
Hyperglycaemia can hardly be proven pathologically-anatomically (even in the case of death due to a form of diabetic coma) with sufficient certainty. The cause of this is the autolysis that occurs after death . For example, the disappearing granules in the B-cells very quickly, only the content of the liquor to lactose and glucose is increased by a diabetic coma. Long-term, structural changes such as amyloidosis of the islets of Langerhans or glomerulosclerosis remain recognizable after death .
In the long term, hyperglycemia leads to glycosylation (without the involvement of enzymes , therefore it is also known as glycation ) of different proteins . A major consequence is microangiopathy due to changes in the basement membrane of capillaries. This appears thickened. Since its permeability is disturbed before long-term effects occur, there is an increase in albumin in the tissue outside the capillaries (extra-capillary space). This applies not only to areas in which typical long-term effects such as diabetic retinopathy , neuropathy , peripheral macroangiopathy and renal insufficiency occur, but also to other areas such as the muscles .
treatment
In terms of treatment, a distinction must be made between acute intervention and long-term treatment (→ treatment of diabetes mellitus ). It also depends on the severity of the hyperglycaemia.
If, for example, slightly elevated blood sugar levels are found during a preventive medical check-up , no acute, blood-sugar-lowering measures are indicated, but rather further diagnostics. If a blood sugar load test reveals a disturbed glucose tolerance without the HbA1c level being increased, improvements in lifestyle such as dietary measures with special consideration of the glycemic index of foods are usually sufficient. If, at the same time, the HbA1c level is moderately increased in the sense of manifest diabetes mellitus , it should be checked to what extent dietary measures are sufficient or whether the administration of medication is necessary.
In the case of greatly increased values from around 250 mg / dl (13.9 mmol / l) to 300 mg / dl (16.7 mmol / l), even in the absence of accompanying symptoms, rapid action is required with the aim of normalizing blood sugar and so on prevent a diabetic coma is indicated. The administration of insulin is particularly suitable for acute therapy .
If a diabetic coma is already present, emergency medical intervention is necessary. (→ Diabetic Coma, Section Therapy )
Prevention and prospect of recovery
In the case of healthy people, apart from the generally applicable rule of a healthy lifestyle, no specific prevention is indicated, as the body is naturally able to keep the blood sugar level within normal limits. If, however, there is a glucose metabolism disorder, regular check- ups with good adherence to therapy are essential, not only with regard to coma prevention, but especially with regard to the best possible prevention of accompanying and secondary diseases , in particular the glycosylation of various proteins and the associated changes in the basement membrane Capillaries (see also section pathology).
history
The most famous effect of hyperglycemia, the occurrence of polyuria, was already known in ancient times. One of the oldest surviving descriptions comes from Aretaios in the 2nd century AD. The occurrence of honey-like tasting urine has also been known for a long time, but the first detection of sugar in urine was not carried out until 1776 by Matthew Dobson . The sugar in urine was made at that time by yeast - fermentation samples .
The presence of sugar in the blood, especially in diabetics, was the subject of scientific research in the first half of the 19th century. With the then usual method of blood testing according to William Hyde Wollaston , no corresponding evidence could be provided.
In 1839, Friedrich Ludwig Hünefeld describes the use of sulfuric acid to test urine for sugar (according to Runge ) as being more sensitive than fermentation and considers it possible to use this method for a corresponding test of the blood. The first actual chemical sugar test, also called Trommer's test, was introduced in 1841 by Karl August Trommer . The first chemical method that allowed a useful estimate of the blood sugar level was the Pettenkofer sugar test. After adding bile solution and sulfuric acid to the blood serum, a discoloration occurs due to heating, which depends on the blood sugar level. This method was described by Pettenkofer in 1844 and also mentioned in a case report in 1847 , i.e. used clinically.
In 1868 a connection between the level of blood sugar and polyuria was questioned. But there were already corresponding theses.
In the same year the view was also expressed that “... the organism does not tolerate the presence of sugar in the circulation, but always tries to get it to be excreted through the urine. ... “ (quoted from Schultz). In the 1970s, medicine still assumed that there was no sugar in the blood of healthy people and that its mere presence should therefore also be regarded as pathological in the sense of the term hyperglycemia . In this context, however, it should be noted that at the time, scientists were still trying to explain diabetes, i.e. the urinary dysentery, using the galenic theory of juices as the excretion of black bile, which tastes unfathomably sweet. In the 1880s, the idea of the Carlsbad doctor Carl Hertzka was taken up, who postulated the excretion of the sugary urine in excessive quantities as a sign of an underlying disease and not as a disease per se. He called the stage before the urinary dysentery the "passive stage of diabetes". In doing so, he finally opened the door to today's understanding of hyperglycemia as a key symptom of diabetes mellitus, although he was also unable to establish a connection between blood sugar levels and the occurrence of glucose / polyuria.
In 1885 normal blood was described as containing sugar and it was also noted that when its sugar content increased to 0.25 to 0.30% (according to today's nomenclature, about 210 to 260 mg / dl), sugar occasionally escapes into the urine, which yes, it had already been considered pathological in earlier years. It took until then until it was established that sugar also circulated in the blood of healthy people (normoglycemia) and that above a certain amount (today this limit is known as the "kidney threshold"), sugar can be found in the urine and thus hyperglycemia (a pathological excess of sugar in the blood) was defined. In 1952, Herder's Volkslexikon describes the normal value of 3.0 grams of sugar (0.07%) in the blood fluid (2800 ml) of 5 liters of blood. According to the units commonly used today, this corresponds to about 60 mg / dl. In 1959, the normal blood sugar level was defined as lying between 70 and 120 mg% (corresponds to mg / dl) ( Hagedorn - Jensen method - a reduction test against ferricyanide ) and thus almost corresponded to the current norm.
literature
- Helmut Schatz (Ed.): Diabetology compact. Basics and practice . 4th, enlarged and updated edition. Georg Thieme, Stuttgart a. a. 2006, ISBN 978-3-13-137724-1 .
- Hellmut Mehnert, Eberhard Standl, Klaus-Henning Usadel, Hans-Ulrich Häring (eds.): Diabetology in clinic and practice . Georg Thieme Verlag, Stuttgart 2003, ISBN 3-13-512805-9 ( limited preview in the Google book search).
Web links
Individual evidence
- ↑ Adolf Faller, Michael Schünke: The human body . Thieme Verlag, Stuttgart 2008, p. 371.
- ↑ a b c d National Health Care Guideline NVL Therapy of Type 2 Diabetes . (PDF)
- ↑ K. Dörner: Clinical chemistry and hematology: 69 tables . Thieme, 2009, ISBN 3-13-129717-4 , p. 148 ( limited preview in the Google book search).
- ↑ RW Nelson: Diabetes mellitus . In: Ettinger, Feldman (Ed.): Textbook of Veterinary Internal Medicine . 5th edition. Saunders, 2000, ISBN 0-7216-7256-6 , Vol. 2, pp. 1438-1460
- ↑ WHO demands: Limo and Cola have to become more expensive , Süddeutsche Zeitung, October 11, 2016
- ↑ WHO urges global action to curtail consumption and health impacts of sugary drinks , World Health Organization (WHO), October 11, 2016.
- ↑ Corresponding taxes have already been introduced by France, Hungary, Finland and Mexico. Questions, answers from Berit Uhlmann: What would a sugar tax do? In: sueddeutsche.de . 2016, ISSN 0174-4917 ( sueddeutsche.de [accessed on November 3, 2017]).
- ↑ JC Behrends: Physiology: 93 tables . Thieme, 2010, ISBN 3-13-138411-5 , p. 360 ( limited preview in Google book search).
- ↑ W. Ahne: Zoologie . Schattauer, 2000, ISBN 3-7945-1764-4 , p. 138 ( limited preview in Google book search).
- ↑ DU Silverthorn et al .: Physiology . Pearson, 2009, ISBN 3-8273-7333-6 , p. 22 ( limited preview in Google book search).
- ↑ S. Silbernagl, et al .: Pocket Atlas of Pathophysiology . Thieme, 2013, ISBN 3-13-150944-9 , p. 275 ( limited preview in Google book search).
- ↑ H. Genzwürker et al .: Anesthesia, intensive care medicine, emergency medicine and pain therapy . Thieme, 2007, ISBN 3-13-167892-5 , p. 312 ( limited preview in the Google book search).
- ↑ G. Herold: Internal Medicine. Self-published, 2007, p. 650.
- ↑ K. Bergis et al .: Diabetes Lexicon: with keyword reg . engl.-Ger.-span . Walter de Gruyter, 1988, ISBN 3-11-011620-0 , p. 114 ( limited preview in the Google book search).
- ↑ H. Bant et al .: Sports Physiotherapy . Georg Thieme, 2011, ISBN 3-13-165941-6 , p. 216 ( limited preview in Google book search).
- ↑ H. Geiger: Kidney diseases: pathophysiology, diagnostics and therapy . Schattauer, 2003, ISBN 3-7945-2177-3 , pp. 73 ff. ( Limited preview in the Google book search).
- ^ A b E. Buddecke: Pathobiochemistry: A textbook for students and doctors . Walter de Gruyter, 1978, ISBN 3-11-159944-2 , p. 86, ( limited preview in the Google book search).
- ↑ Hanes CS: An application of the method of Hagedorn and Jensen to the determination of larger quantities of reducing sugars In: Biochem J. 1929; 23 (1): 99-106, PMC 1253996 (free full text).
- ↑ C. Thomas: Macropathology . Schattauer, 1983, ISBN 3-7945-0910-2 , p. 179.
- ↑ H.-U. Häring et al .: Diabetology in Clinic and Practice . Georg Thieme, 2011, ISBN 3-13-157636-7 , p. 42 ff. ( Limited preview in the Google book search).
- ↑ HWBaenkler: Internal Medicine . Georg Thieme, 2001, ISBN 3-13-128751-9 , p. 940 ( limited preview in the Google book search).
- ↑ JFMeckel: German Archive for the physiology. Volume 1, 1815, p. 137 ( full text in the Google book search).
- ↑ GH Schwartze: Pharmacological tables or systematic drug theory in tabular form. Volume 2, Barth, 1839, p. 77 ( full text in the Google book search).
- ↑ J. Bostock et al .: The Cyclopædia of Practical Medicine: Comprising Treatises on the Nature and Treatment of Diseases, Materia Medica and Therapeutics, Medical Jurisprudence, Etc. Etc. Volume 1, Sherwood, Gilbert, and Piper, 1832, p. 540 ( full text in the Google book search).
- ↑ OL Erdmann: Journal for practical chemistry, Volume 16 , JA Barth, 1839, p. 31 ff. ( Full text in the Google book search).
- ^ HWO Seifert: Pocket book of medical-clinical diagnostics . Рипол Классик, ISBN 5-88025-877-7 , p. 144 ( limited preview in Google Book Search; first edition 1886).
- ↑ H. Schott: Chronicle of Medicine . Chronicle, 1993, ISBN 3-611-00273-9 , p. 404.
- ^ Max von Pettenkofer: Kleine Schriften, Volume 9 . Bayerische Staatsbibliothek, 1844, p. 90 ff. ( Full text in the Google book search).
- ^ W. Roser et al .: Archive for Physiological Medicine , 1848, p. 206 ( full text in the Google book search).
- ↑ A. v. Düring: cause and cure of diabetes mellitus . Schmorl & Seefeld, 1868, p. 11 ( full text in the Google book search).
- ↑ E. Schulz: About Diabetes Mellitus . 1868, p. 7 ( limited preview in Google Book search).
- ↑ E. Schultz: About Diabetes Mellitus . 1868, p. 11 ( limited preview in Google Book search).
- ↑ E. Harnack: On the pathogenesis and therapy of diabetes mellitus . Verlag H. Laakmann, 1873, p. 10 ( full text in the Google book search).
- ↑ DMW, German Medical Weekly . Volume 13, p. 131 ( limited preview in Google Book search).
- ^ Yearbook of practical medicine: Critical annual report for the training of practical doctors . F. Enke, 1885, p. 307 ( limited preview in Google book search).
- ↑ Herder's Encyclopaedia A-Z . Herder Verlag, Freiburg, 1952, p. 179.
- ↑ H. Huismans: Lexicon of clinical diabetology: practice-oriented interdisciplinary presentation . Deutscher Ärzteverlag, 2005, ISBN 3-7691-0478-1 , p. 14 ( limited preview in the Google book search).
- ^ W. Pschyrembel: Clinical dictionary . Walter de Gruyter, 1959, p. 109 ( limited preview in the Google book search).