Merkel cell polyomavirus
| Merkel cell polyomavirus | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Systematics | ||||||||||||||||||||
|
||||||||||||||||||||
| Taxonomic characteristics | ||||||||||||||||||||
|
||||||||||||||||||||
| Scientific name | ||||||||||||||||||||
| Merkel cell polyomavirus | ||||||||||||||||||||
| Short name | ||||||||||||||||||||
| MCPyV | ||||||||||||||||||||
| Left | ||||||||||||||||||||
|
The Merkel cell polyomavirus ( MCPyV or MCV ) was discovered in January of 2008. MCPyV is one of seven oncoviruses known in humans . It is believed to cause the majority of all Merkel cell carcinoma cases , a rare but aggressive form of skin cancer . Infections with MCPyV were found in about 80% of Merkel cell carcinomas (MCC). Antibodies against MCPyV (which indicate contact with the virus) can be detected in healthy people, depending on the age group, in up to 80% of the test persons, whereby this seroprevalence in children under 15 years is already 50%. Since it was also found in bronchial secretions , it can be assumed to be transmitted via the airways. These isolates in healthy virus carriers correspond to the unmutated wild type. Most virus genomes isolated from MCC tumors are subject to at least two mutations that make them non-communicable: firstly, the virus is clonally integrated into the host genome , and secondly, the viral T antigen is shortened by a mutation so that it is necessary for the replication of the viral genome can no longer initiate necessary cellular DNA replication .
The fact that MCPyV is the cause of the MCC tumors infected with it has been proven in studies by inhibiting the virus oncoproteins . If these virus proteins are suppressed, the cells of MCPyV-positive Merkel cell carcinomas die, in contrast to the cells from tumors that do not carry the virus. The virus-positive tumor cells are therefore dependent on MCPyV.
MCPyV is subordinated to the species Human polyomavirus 5 by the International Committee on Taxonomy of Viruses (ICTV) .
classification
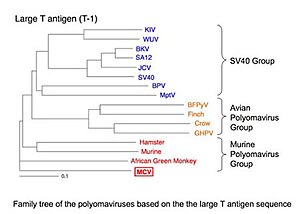
MCPyV is the fifth polyomavirus to be discovered in humans. The MCPyV has been tentatively assigned as an unclassified species of the genus Polyomavirus . Among the three genogroups of this genus it belongs to the group of the murine polyomavirus . This group is named after the murine polyomavirus that was first discovered and does not imply that MCPyV is transmitted from rodents to humans. To date, MCPyV is the only human polyomavirus that does not fall into the SV40 -like group .
MCPyV is the B-lymphotropic polyomavirus genetically very similar (formerly African green monkey lymphotropic papovavirus called), so it could be a co-evolution with the apes have passed.
Virus genome
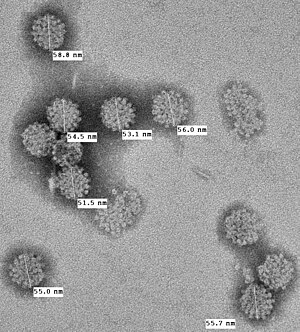
Polyomaviruses are about 50 nm small, envelope-free viruses with a double-stranded circular DNA as genome. The genome of the MCPyV prototype consists of 5387 base pairs and encodes characteristic proteins of the polyomaviruses including a large T antigen and a small t antigen as non-structural proteins as well as the structural proteins VP1 and VP2 / 3 for the construction of the capsid . The large MCPyV T antigen is similar to the T antigens of other polyomaviruses, so-called oncogenes , and is expressed as in human tumors. The T antigen is a spliced gene and makes different proteins depending on the splice pattern. Large and small T antigen proteins can transform healthy cells into tumor cells by inhibiting tumor suppressors such as the retinoblastoma protein . The large T antigen also has a DNA helicase and a binding site for the origin of replication of the viral DNA, which the cellular DNA polymerase needs to replicate the viral genome. The virus itself does not code for its own viral DNA polymerase , which is why, as with all polyoma and papilloma viruses , it is dependent on the cellular DNA polymerase , which is only active during cell division (S phase). As with all DNA viruses, the replication of the virus genome therefore takes place in the nucleus of the host cell.
Viral etiology of Merkel cell carcinoma
The Merkel cell carcinoma is a highly aggressive skin cancer , the first in 1972 by Cyril Toker was described as "trabecular skin tumor." The cancer seems to originate from the microscopic Merkel bodies in the skin and intestines, which are responsible for sensations of touch and pressure. Accordingly, it is one of the neuroectodermal tumors . MCC is rare compared to other skin cancers, but its incidence in the US tripled between 1986 and 2001 to approximately 1,400 cases per year.
Merkel cell carcinomas are mostly found in older people. It is also known that patients with immunodeficiencies get sick more often, e.g. B. after organ transplants or with an AIDS infection, and this fact supports the assumption that a virus or other infectious agent is involved in the development of cancer. Kaposi's sarcomas and Burkitt's lymphomas are examples of tumors of known viral etiology that are more common in immunocompromised individuals. Another risk factor for developing MCC is ultraviolet light .
In a first study, eight out of ten Merkel cell carcinomas were infected with MCPyV. The virus is integrated in these tumors in the cancer cell genome and can no longer reproduce freely. Current studies from other laboratories have confirmed this: In one study, 30 of 39 (77%) Merkel cell tumors were MCPyV-positive; in another study 45 out of 53 (85%).
The viruses from Merkel cell tumors were sequenced; they regularly showed tumor-specific mutations that shorten the MCPyV-T antigen. These mutations (which do not occur in the native virus isolated from non-tumor tissue) eliminate the T-antigen helicase and thus prevent the integrated virus from multiplying independently of the host cancer cell. The tumor is a "dead end" for the virus. Usually the virus exists as a circular episome (or plasmid) within the cell, and its DNA is packaged in viral capsids and transferred to other cells. In tumor cells, the virus DNA has broken down and integrated into human DNA, so that the virus can no longer be transmitted. It cannot leave the host cell and can only multiply together with the host cell. Research on infected tumors has shown that the majority of them have a clear monoclonal pattern, suggesting that the virus originally entered a single cell before it began its cancerous reproduction. This is very strong evidence that MCPyV causes some - but not all - of Merkel cell carcinomas. MCPyV can also be found in normal tissue from people without Merkel cell carcinoma. A complete MCPyV genome (MCV-HF) was assembled from several MCPyV genomes of the tumor type and had the ability to replicate successfully in vitro. Identical sequences have been found in normal human skin. The exact prevalence of the infection in humans is unknown, but it is likely that most infections will not cause cancer.
Prevention, diagnosis, treatment
Patients with virus-positive Merkel cell carcinoma are not infectious to others, and protective measures are not required. This is due to the fact that, on the one hand, the tumor virus has already mutated and can no longer be transmitted, and on the other hand, most people were exposed to the virus through asymptomatic carriers in their childhood or as young adults.
According to the current data, MCC, like other skin cancers, can be prevented by preventing sunburn and unnecessary exposure to the sun, and by using sunscreens. In this way, risk-increasing virus mutations can be prevented in people who are already infected with MCPyV. People with immunosuppression (e.g. AIDS patients or organ recipients) have a higher risk of developing this type of cancer and could benefit from regular skin exams. Any painless, rapidly growing tumor, especially in those over 50 or those who are immunocompromised, must be shown to a doctor. The diagnosis of Merkel cell tumor can be made quickly by a biopsy , and in the early stages the prognosis after standard therapy is good. So far, there are no preventive vaccinations or drugs that could prevent the infection or the development of cancer.
Detection of the virus is the subject of research and is usually not available as a clinical test. The viral DNA is detected by means of PCR or Southern Blot . Caution should be exercised when interpreting PCR results because false positive contamination will occur and a significant proportion of samples from healthy skin may be weakly infected. The presence or absence of tumor-specific mutations can be determined by sequencing the virus genome.
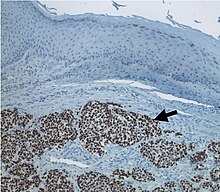
Antibodies have been developed that stain the T antigen in tumor tissue and appear to be specific for MCPyV-infected cancer cells. Blood tests have also been developed to show that the majority of adults have been exposed to MCPyV and may be carrying it as an asymptomatic infection.
The treatment guidelines do not differentiate between Merkel cell carcinomas with and without MCPyV infection. A recent nationwide study in Finland suggests that MCPyV-positive tumors have a better prognosis than non-infected tumors (although other studies did not). If this is confirmed, routine virus detection could be useful in future medical treatment. As far as we know so far, the virus itself is insensitive to common antiviral drugs.
Discovery and description of the MCPyV
Yuan Chang and Patrick S. Moore , who discovered Kaposi's sarcoma herpes virus in 1994 , together with their colleagues Huichen Feng and Masa Shuda at the University of Pittsburgh (USA) used the new high-speed sequencing technique called digital transcriptome subtraction (DTS) to look for a virus in Merkel cell tumors. In this method, all of the mRNA from the tumor is converted into cDNA and sequenced deep enough to find a viral cDNA, if one is present. The sequences are then compared to the human genome, and all of the human sequences are "subtracted" leaving a number of most likely non-human sequences. When this was done on four cases of Merkel cell carcinoma, a cDNA was found that resembled the sequences of known polyomaviruses, but with enough differences to identify them as a new virus. For the study, genetic sequences from almost 400,000 strands of mRNA were analyzed. Once the virus was found, Feng and coworkers quickly determined that the infected Merkel cell carcinomas carried it in an integrated monoclonal pattern and that only 8-16% of tissue samples from patients without MCC were positive for the virus. This was quickly confirmed by studies in MCC patients around the world; including evidence of monoclonal integration of the virus in these tumors.
MCPyV as a cause of Merkel cell carcinoma
While the original authors cautiously noted that it was "too early" to determine whether MCPyV was a cause of Merkel cell carcinoma, the scientific public now suspects that the virus causes most, if not all, Merkel cell tumors. The virus, if present, is monoclonally integrated into the tumor, ie the later tumor stem cell was attacked before its cancerous multiplication. Mutations of the T antigen make the virus infectious, so it cannot have infected the tumor that has already developed as a secondary infection ( passenger virus ). Eventually, the T antigen oncogene is expressed in all tumor cells, and when inhibited by RNAi , the MCPyV positive cells die. MCPyV-positive tumors therefore need the virus to grow. Other host cell mutations likely contribute to ultimately triggering the tumor. Merkel cell carcinoma is associated with exposure to UV and ionizing radiation, and these mutagens likely increase the mutation rate either in the virus or in the Merkel cell genome and thus contribute to the risk of cancer after infection.
It remains completely open why 20% of Merkel cell carcinomas are virus-negative. Among other things, it is speculated that Merkel cell carcinoma could actually be two or more closely related cancers, only one of them with MCPyV infection. Misdiagnosis of the difficult cancer entity could be responsible for some of the negative results. Only a small proportion of those infected with MCV will develop the cancer. There is currently no generally available test for the virus and no change in recommended treatment based on known MCPyV infection status. MCC patients can participate in studies, but they are unlikely to benefit personally. Sun protection measures reduce UV exposure and are believed to reduce the risk of developing MCC as well as other types of skin cancers.
Moore has suggested that one could develop with the information about the virus, if they are correct a blood test or a vaccination, to improve the treatment of the disease or prevent it, such as the HPV vaccine to the cervical forward bending. Chang said studying MCPyV might help to better understand other cancers as well: “Once the virus is integrated, it could produce an oncoprotein or it could turn off a gene that inhibits tumor growth. Anyway, the results will be interesting. "
Sources and individual references
- ↑ a b c d e ICTV: ICTV Taxonomy history: Human polyomavirus 1 , EC 51, Berlin, Germany, July 2019; Email ratification March 2020 (MSL # 35)
- ↑ a b c d e f g h i H. Feng, M. Shuda, Y. Chang, PS Moore: Clonal Integration of a Polyomavirus in Human Merkel Cell Carcinoma . In: Science . 319, No. 5866, 2008, pp. 1096-1100. doi : 10.1126 / science.1152586 . PMID 18202256 . PMC 2740911 (free full text).
- ^ A b Jaime M. Kean, Suchitra Rao, Michael Wang, Robert L. Garcea, Walter J. Atwood: Seroepidemiology of Human Polyomaviruses . In: PLoS Pathogens . 5, No. 3, 2009, p. E1000363. doi : 10.1371 / journal.ppat.1000363 . PMID 19325891 . PMC 2655709 (free full text).
- ↑ a b c Yanis L. Tolstov, Diana V. Pastrana, Huichen Feng, Jürgen C. Becker, Frank J. Jenkins, Stergios Moschos, Yuan Chang, Christopher B. Buck: Human Merkel cell polyomavirus infection II. MCV is a common human infection that can be detected by conformational capsid epitope immunoassays . In: International Journal of Cancer . 125, No. 6, 2009, pp. 1250-1256. doi : 10.1002 / ijc.24509 . PMID 19499548 . PMC 2747737 (free full text).
- ↑ cdc.gov
- ↑ cdc.gov
- ↑ a b c M. Shuda, H. Feng, HJ Kwun, ST Rosen, O. Gjoerup, PS Moore, Y. Chang: T antigen mutations are a human tumor-specific signature for Merkel cell polyomavirus . In: Proceedings of the National Academy of Sciences . 105, No. 42, 2008, pp. 16272-7. doi : 10.1073 / pnas.0806526105 . PMID 18812503 . PMC 2551627 (free full text).
- ↑ jvi.asm.org
- ↑ ICTV: Polyomaviridae , ICTV Report, June 2017, revision from July 2018.
- ↑ M. Pawlita, A. Clad, H. zur Hausen: Complete DNA sequence of lymphotropic papovavirus: prototype of a new species of the polyomavirus genus . In: Virology . 143, No. 1, May 1985, pp. 196-211. doi : 10.1016 / 0042-6822 (85) 90108-4 . PMID 2998001 .
- ↑ Archived copy ( Memento of the original from January 21, 2010 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice.
- ^ Toker C: Trabecular carcinoma of the skin . In: Archives of Dermatology . 105, No. 1, January 1972, pp. 107-10. doi : 10.1001 / archderm.105.1.107 . PMID 5009611 .
- ↑ SM Maricich, SA Wellnitz, AM Nelson, DR Lesniak, GJ Gerling, EA Lumpkin, HY Zoghbi: Merkel Cells are Essential for Light Touch Responses . In: Science . 324, No. 5934, 2009, pp. 1580-1582. doi : 10.1126 / science.1172890 . PMID 19541997 . PMC 2743005 (free full text).
- ↑ a b c Christopher K. Bichakjian, Lori Lowe, Christopher D. Lao, Howard M. Sandler, Carol R. Bradford, Timothy M. Johnson, Sandra L. Wong: Merkel cell carcinoma: Critical review with guidelines for multidisciplinary management . In: Cancer . 110, No. 1, 2007, pp. 1-12. doi : 10.1002 / cncr.22765 . PMID 17520670 .
- ↑ RH Williams, MB Morgan, IM Mathieson, H. Rabb: Merkel cell carcinoma in a renal transplant patient: increased incidence? . In: transplant . 65, No. 10, May 1998, pp. 1396-1397. doi : 10.1097 / 00007890-199805270-00019 . PMID 9625025 .
- ↑ E. Engels, M. Frisch, J. Goedert, R. Biggar, R. Miller: Merkel cell carcinoma and HIV infection . In: The Lancet . 359, No. 9305, 2002, pp. 497-498. doi : 10.1016 / S0140-6736 (02) 07668-7 . PMID 11853800 .
- ↑ a b Ahmad Kassem, Anja Schöpflin, Carlos Diaz, Wolfgang Weyers, Elmar Stickeler, Martin Werner, Axel Zur Hausen: Frequent Detection of Merkel Cell Polyomavirus in Human Merkel Cell Carcinomas and Identification of a Unique Deletion in the VP1 Gene . In: Cancer Research . 68, No. 13, 2008, pp. 5009-5013. doi : 10.1158 / 0008-5472.CAN-08-0949 . PMID 18593898 .
- ↑ a b c Jürgen C Becker, Roland Houben, Selma Ugurel, Uwe Trefzer, Claudia Pföhler, David Schrama: MC Polyomavirus Is Frequently Present in Merkel Cell Carcinoma of European Patients . In: Journal of Investigative Dermatology . 129, No. 1, 2008, pp. 248-250. doi : 10.1038 / jid.2008.198 . PMID 18633441 .
- ↑ Huichen Feng, Hyun Jin Kwun, Xi Liu, Ole Gjoerup, Donna B. Stolz, Yuan Chang, Patrick S. Moore: Cellular and Viral Factors Regulating Merkel Cell Polyomavirus Replication . In: PLOS ONE . 6, No. 7, 2011, p. E22468. doi : 10.1371 / journal.pone.0022468 . PMID 21799863 .
- ↑ Rachel M. Schowalter, Diana V. Pastrana, Katherine A. Pumphrey, Adam L. Moyer, Christopher B. Buck: Merkel Cell Polyomavirus and Two Previously Unknown Polyomaviruses Are Chronically Shed from Human Skin . In: Cell Host & Microbe . 6, No. 6, 2010, pp. 509-515. doi : 10.1016 / j.chom.2010.05.006 . PMID 20542254 .
- ↑ RP Viscidi, KV Shah: CANCER: A Skin Cancer Virus? . In: Science . 319, No. 5866, 2008, pp. 1049-1050. doi : 10.1126 / science.1155048 . PMID 18292327 .
- ↑ Masahiro Shuda, Reety Arora, Hyun Jin Kwun, Huichen Feng, Ronit Sarid, María-Teresa Fernández-Figueras, Yanis Tolstov, Ole Gjoerup: Human Merkel cell polyomavirus infection I. MCV T antigen expression in Merkel cell carcinoma, lymphoidues and lymphoid tumors . In: International Journal of Cancer . 125, No. 6, 2009, pp. 1243-1249. doi : 10.1002 / ijc.24510 . PMID 19499546 .
- ↑ Roland Houben, David Schrama, Miriam Alb, Claudia Pföhler, Uwe Trefzer, Selma Ugurel, Jürgen C. Becker: Comparable expression and phosphorylation of the retinoblastoma protein in Merkel cell polyoma virus positive and negative Merkel cell carcinoma . In: International Journal of Cancer . 126, No. 3, 2009, pp. 796-798. doi : 10.1002 / ijc.24790 . PMID 19637243 .
- ↑ Klaus J. Busam, Achim A. Jungbluth, Natasha Rekthman, Daniel Coit, Melissa Pulitzer, Jason Bini, Reety Arora, Nicole C. Hanson: Merkel Cell Polyomavirus Expression in Merkel Cell Carcinomas and Its Absence in Combined Tumors and Pulmonary Neuroendocrine Carcinomas . In: The American Journal of Surgical Pathology . 33, No. 9, 2009, pp. 1378-1385. doi : 10.1097 / PAS.0b013e3181aa30a5 . PMID 19609205 .
- ↑ H. Sihto, H. Kukko, V. Koljonen, R. Sankila, T. Bohling, H. Joensuu: Clinical Factors Associated With Merkel Cell polyomavirus infection in Merkel Cell Carcinoma . In: Journal of the National Cancer Institute . 101, No. 13, 2009, pp. 938-945. doi : 10.1093 / jnci / djp139 . PMID 19535775 .
- ↑ Y Chang, E Cesarman, M. Pessin, F Lee, J Culpepper, D. Knowles, P. Moore: Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma . In: Science . 266, No. 5192, 1994, pp. 1865-1869. doi : 10.1126 / science.7997879 . PMID 7997879 .
- ↑ H. Feng, JL Taylor, PV Benos, R. Newton, K. Waddell, SB Lucas, Y. Chang, PS Moore: Human Transcriptome Subtraction by Using Short Sequence Tags To Search for Tumor Viruses in Conjunctival Carcinoma . In: Journal of Virology . 81, No. 20, 2007, pp. 11332-11340. doi : 10.1128 / JVI.00875-07 . PMID 17686852 . PMC 2045575 (free full text).
- ↑ Xavier Sastre-Garau, Martine Peter, Marie-FrançOise Avril, Hélène Laude, Jérôme Couturier, Flore Rozenberg, Anna Almeida, FrançOise Boitier: Merkel cell carcinoma of the skin: pathological and molecular evidence for a causative role of MCV in oncogenesis . In: The Journal of Pathology . 218, No. 1, 2009, pp. 48-56. doi : 10.1002 / path.2532 . PMID 19291712 .
- ↑ Christopher B. Buck, Douglas R. Lowy: Getting Stronger: The Relationship Between a Newly Identified Virus and Merkel Cell Carcinoma . In: Journal of Investigative Dermatology . 129, No. 1, 2009, pp. 9-11. doi : 10.1038 / jid.2008.302 . PMID 19078983 .
- ^ New Pathogen Discovery: Frequently Asked Questions . KSHV laboratory, molecular virology program, University of Pittsburgh Cancer Institute. Archived from the original on April 22, 2008. Retrieved April 13, 2008.
- ↑ Newly Discovered Virus Linked To Deadly Skin Cancer , University of Pittsburgh Medical Center News Bureau, Jan. 17, 2007 at sciencedaily.com
- ↑ Allison Gandey: newly discovered virus linked to neuroendocrine cancer of the skin . MedScape Medical News. January 18, 2008. Retrieved May 28, 2012.