appendicitis
| Classification according to ICD-10 | |
|---|---|
| K35 | Acute appendicitis |
| K36 | Other appendicitis - chronic appendicitis - recurrent appendicitis |
| K37 | Unspecified appendicitis |
| ICD-10 online (WHO version 2019) | |
The appendicitis (Latin appendicitis ) or appendicitis is an inflammation of the appendix (vermiform appendix) at the end of the caecum (cecum). If the appendix is inflamed, it is called typhlitis . In German appendicitis is also colloquially referred to as appendicitis . The acute appendicitis ( acute appendicitis ) is an emergency.
The course of the disease can range from slight irritation to severe inflammation and abscess formation to perforation of the wall ( intestinal perforation ) in the free abdominal cavity and thus to life-threatening peritonitis (peritonitis).
Anatomy, causes, frequency
The cecum ( cecum ), the "blind" the initial part of the ascending in the right lower abdomen colon ( ascending colon ). Appendectomy is an appendage, called the appendix ( vermiform appendix ). The appendix contains many lymphatic follicles and can become inflamed through infection with pathogens, but more often through laying, for example, with excrement stones or foreign bodies such as cherry pits or , more rarely, pits of grapes or melons . A worm infestation ( roundworms or oxyurs ) of the intestine is sometimes associated with it.
Appendicitis is the most common cause of the acute abdomen and occurs in western countries with a frequency of about 100 cases per 100,000 people per year. Between 2007 and 2009, an average of around 127,000 appendectomy operations (surgical removal of the appendix, appendectomies ) were performed each year. The risk of developing appendicitis in the course of life (life-time risk) is around 7–8%.
According to the 2009 hospital diagnosis statistics, appendicitis occurs most frequently in children and adolescents as well as in young adults. 38% of all appendectomies are performed in the 5 to 19 age group, 58% in the 5 to 29 age group. Small children are less likely to get sick, but tend to have only minor clinical symptoms and atypical courses, making the disease more dangerous. In children over 2 years of age, appendicitis is the most common cause of the acute abdomen.
In 2009, 46,500 children and adolescents between the ages of 5 and 19 years of age were operated on their appendix across Germany. However, there are clear differences in the frequency of operations in the individual districts. In the district with the highest OP index (2.3), this is six times higher than in the district with the lowest index (0.4), based on the number of people between the ages of 5 and 19 living there.
complaints
The main symptom is the clinical symptom change in the local abdominal finding: pain is usually felt in the area of the navel (periumbilical) and in the epigastric region, which shift to the right lower abdomen within a few hours. Patients often suffer from loss of appetite , nausea , vomiting and, in advanced stages, develop intestinal paralysis (paralytic ileus ). The body temperature can rise to 39 ° C ( fever ; there is a temperature difference between rectal and axillary measurements of about 1 ° C) with a correspondingly accelerated pulse ( tachycardia ). A displacement of the appendix can cause pain in the right upper or middle abdomen in pregnant women. In older patients, the symptoms are not so clearly pronounced, so that the symptoms cannot be assigned so easily (so-called age appendicitis). Symptoms of acute appendicitis are not always typical, so making a diagnosis can be difficult. In retrocecal (behind the cecum ) appendicitis, inflammation of the ureter is very common . The resulting erythrocyturia and leukocyturia must not lead to a hasty rejection of the diagnosis of appendicitis.
Diagnosis
The diagnosis of appendicitis is made during the medical examination. Most important are the anamnesis , the laboratory tests (in particular the determination of the increased white blood cell count and increased CRP value), the ultrasound and, in the case of technical difficulties, the CT. There is no test that can confirm or rule out appendicitis with certainty. The diagnosis of acute appendicitis is not easy, as it is usually based on rather unspecific signs such as right-sided lower abdominal pain, fever, increased inflammation values and the patient's history. The surgeon's discretion plays an important role in deciding whether or not to have surgery.
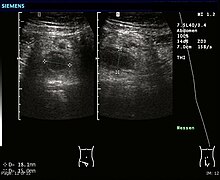
There is no external evidence that appendicitis is present. However, with a typical finding in the ultrasound, the diagnosis is now certain, since the ultrasound resolution has reached sufficient quality. However , it is often difficult to rule out appendicitis in the presence of an over-inflated bowel or in obese patients, as their abdomen is difficult to assess on ultrasound and by means of palpation. Computed tomography can be helpful here.
The measurement of the temperature difference between the armpit and the rectum (0.5–1 ° C), which was common in the past, is rarely used today.
Clinical examination and laboratory
The diagnosis of appendicitis is supported by clinical findings:

- Taking the patient's history and physical examination with palpation of the abdomen
- The palpation of the lower abdomen McBurney's point , lance-point , retrograde direction Darmausstreichen in Appendix (so-called. Rovsing's sign )
- Contralateral pain in letting go ( Blumberg's sign ): On the opposite side of the body (contralateral, i.e. on the left), manual pressure is exerted on the lower abdomen and suddenly released again. In the positive (= applicable) case, there is then pain on the right.
- Psoas stretch pain (the leg is bent in the hip joint against resistance; if pain occurs in the lower abdomen, the test is positive)
- Pain when shaken
- Douglas pain (pain on digital rectal examination)
- Ligat sample ( hyperesthesia of the 10th dermatome . In 86% of the cases in which the sample is positive, non-perforated appendicitis is present)
- Sitkowski's sign (increasing pain symptoms when taking the left lateral position due to internal stretching)
- Ten horn sign (active pulling down of the testicle causes pain at McBurney's point)
- Retraction sign (pressure at the McBurney point causes the right testicle to be pulled up briefly by the cremaster muscle )
- Temperature measurement
- Blood test, possibly also urine test
- Laboratory examination of the blood ( leukocytosis , increase in CRP, etc.)
- always gynecological examination in women
When taking the anamnesis, the pain may be shifted from the central upper abdomen to the right lower abdomen and the initially periumbilical (near the navel) or epigastric (near the stomach) pain may cease. The cause of this characteristic migration of pain lies in the local involvement of the parietal peritoneum adjacent to the inflammation focus in the disease process (visceral pain → peritoneal pain).
The sudden occurrence of a pain-free interval (the so-called "lazy peace") with subsequent massive pain throughout the abdomen suggests a breakthrough (a perforation of the intestine ) of appendicitis.
Imaging
- Ultrasound examination of the abdominal cavity (cockade deformation, tubular structure, abscess, exclusion of other diseases): A specific sign of appendicitis is a maximum external diameter of the appendix of more than 6 or 7 mm, with a larger diameter being more specific. The inflamed appendix is at least partially round in the transverse section and is non-compressible. A appendicolith is also specific to appendicitis, regardless of the maximum outer diameter of the appendix. Secondary signs of appendicitis are a wall thickness greater than 3 mm, a halo due to edema, and increased edematous mesenteric fat.
- Magnetic resonance imaging
- Computed tomography (CT)
- Possibly. X-ray of the abdomen while standing
Differential diagnoses
The following list of other possible diagnoses that may be hidden behind suspected appendicitis ( differential diagnoses ) is long. It includes all diseases that manifest themselves as severe abdominal and abdominal pain. The medical term for this complex is acute abdomen . With technical examination options and clinical follow-up examinations, these options can usually be reduced to a few diseases.
Gastrointestinal differential diagnoses
- Cholecystitis
- Crohn's disease
- Diverticulitis
- Meckel's diverticulum
- Duodenal ulcer
- gastroenteritis
- Enterocolitis
- Intestinal obstruction
- Tumor diseases
- Pancreatitis with exudate road towards the right lower abdomen
- Intestinal perforation
- Volvulus
- Non-specific abdominal pain ( irritable bowel syndrome )
- Epiploic appendicitis
- Mesenteric lymphadenitis ( Yersinia )
Gynecological and urological differential diagnoses
- Ovarian torsion
- Tubal pregnancy
- Endometriosis
- Twisted ovarian cyst
- Adnexitis
- Rupture of an ovarian cyst
- Ureteral stone
- Pyelonephritis
- Testicular torsion
- Cystitis
- Perinephritic (kidney-shaped) abscess
- Ovarian vein thrombosis
Pulmonary differential diagnoses
Systemic differential diagnoses
- Ketoacidosis in diabetes mellitus (pseudoappendicitis diabetic)
- Porphyry
- Henoch-Schönlein purpura
Differential Diagnoses in Children
- gastroenteritis
- Right basal pneumonia
- Urinary tract infections
- Constipation
- Twisted ovarian cyst in girls
- Celiac disease
- Meckel's diverticulum
treatment
The quality of treatment is measured by the rate of non-indicated appendectomies (negative appendectomy rate). The negative appendectomy, i.e. a free appendix operation, is confirmed by a histological examination. The negative appendectomy rate, i.e. H. the presence of a normal appendix with a positive examination result is between 10 and 40%. With additional diagnostics, after surgical evaluation, using computed tomography , the negative appendectomy rate can be reduced to 4%.
In principle, it is possible to wait with conservative treatment (bed rest, antibiotic treatment , food abstinence and laboratory tests). With this approach, studies have shown that the negative appendectomy rate can be reduced to 6%.
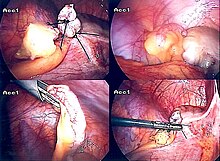
In principle, the operation remains indicated if acute appendicitis cannot be ruled out with sufficient certainty. The risk of negative appendectomies is lower than the risk of acute appendicitis. In up to 28% of patients a perforation of the appendix is found during the operation, which is associated with a mortality rate of approx. 10% (in the case of diffuse peritonitis up to 30%). The operation should be performed as early as possible (within about 48 hours). The appendectomy can be performed openly surgically through the so-called lower abdominal change incision (so-called laparatomy ) or laparoscopically with the help of a camera inserted into the abdominal cavity and other working accesses (so-called minimally invasive laparoscopy or "keyhole surgery").
The prognosis (prospect of a cure) for the disease is very good. The lethality during the procedure for non-perforated appendicitis is below 0.1% and is therefore very low. If the inflammation breaks out into the free abdominal cavity (perforation), however, it is around 10%.
Complications
- Conglomerate tumor
- perityphlitic abscess
- Perforation with peritonitis (about 5 to 10% of operated cases)
- Douglas abscess
- Paralytic ileus
history
Appendicitis was treated conservatively until the early 20th century, but often with poor results in the case of real appendicitis. Appendicitis was systematically researched from around 1886 by the Virchow student and Harvard professor Reginald Heber Fitz (1843–1913), who also gave this disease its name. A prominent case was the British King Edward VII , who ascended the throne in 1901 and only survived severe appendicitis with difficulty shortly before his coronation.
The French surgeon Claudius Amyand is said to have surgically removed the appendage ( appendectomy ) in 1735 . The first successful appendectomy is an operation performed on January 4, 1885 in Davenport (Iowa) on 22-year-old Mary Gartside by the surgeon William West Grant . Gartside made a full recovery and did not die until 1919. The Canadian surgeon Abraham Groves (1847–1935), who is said to have successfully performed an appendectomy in North America in 1883, and the British surgeon Robert Lawson Tait (1845–1899), were also pioneers of appendectomy . of which the first appendectomy is said to have been documented as early as 1880.
The vermiform appendix was removed from perforated appendix inflammation by George Thomas Morton in 1887 . One of the first German surgeons who advocated the surgical removal of the inflamed appendix was Bernhard Riedel , who was born in Mecklenburg (since 1888 professor and director of the surgical clinic in Jena). At the same time as the American Charles McBurney , Riedel developed the interchangeable incision as a surgical technique. McBurney, who also advocated early surgery for appendicitis, published his classic report on early surgical intervention in front of the New York Surgical Society in 1889 , which was made popular by John Murphy (1857-1916) and from around 1910 also became generally accepted in Europe. McBurney described the point of greatest pain in the right lower abdomen, which has since been known as the McBurney point . After the first surgical successes in appendicitis, the disease became a purely surgical matter for several decades. The surgeon diagnosed and operated on her. This led to a relatively high number of appendectomy operations. A milestone in surgical technology was the introduction and spread of laparoscopic appendectomy between 1980 and 1990.
With the refinement of the imaging diagnostics of ultrasound and CT, as well as the expansion of inflammation diagnostics in the blood using CRP and leukocytes , the indication for appendectomy moved back somewhat to internal medicine , and the number of unnecessary appendectomy operations decreased. Today, only about every tenth patient suspected of having appendicitis is operated on. What is astonishing in the medical history of appendicitis is the lack of experience with antibiotic therapy for this disease. Even when comparing surgical therapy with surgical therapy plus administration of antibiotics, there are hardly any usable comparative studies.
research
A 2014 study at Turku University Medical Center showed that antibiotic treatment can in some cases eliminate the need for surgical appendectomy. However, it is unclear whether this approach ultimately benefits patients.
According to a US study, outpatient appendectomies are safe.
literature
- Health fact check. Regional differences in health care . Bertelsmann Foundation, 2011.
- Charles McBurney : Experiences with Early Operative Interference in Cases of Disease of the Vermiform Appendix. In: New York Medical Journal , 1889, Volume 50, pp. 676-684.
- CG Thomas Jr .: Experiences with Early Operative Interference in Cases of Disease of the Vermiform Appendix by Charles McBurney, MD, Visiting Surgeon to the Roosevelt Hospital, New York City. In: Review of surgery. May-June 1969, Vol. 26, No. 3, pp. 153-166, PMID 4893208 .
- James N. Parker, Philip M. Parker: Appendicitis: A Medical Dictionary, Bibliography, and Annotated Research Guide to Internet References. Icon Health Publications, San Diego CA 2003, ISBN 0-585-49038-4 .
- Hans Adolf Kühn: Appendicitis (appendicitis), appendicitis. In: Ludwig Heilmeyer (ed.): Textbook of internal medicine. Springer-Verlag, Berlin / Göttingen / Heidelberg 1955; 2nd edition, ibid. 1961, pp. 813-816.
Web links
- E-learning course on appendicitis with images and videos (Charité Berlin)
- Fact check health appendix removal
Individual evidence
- ↑ a b c d Regional differences in health care . Health fact check. Bertelsmann Stiftung, 2011, p. 32 f.
- ↑ CM Rumack et al .: Diagnostic Ultrasonic Imaging. 4th edition, Elsevier / Mosby, Philadelphia PA 2011, ISBN 978-0-323-05397-6 , p. 286.
- ↑ CM Rumack et al .: Diagnostic Ultrasonic Imaging. Philadelphia PA 2011, p. 288.
- ^ AB Goldin, P. Khanna, M. Thapa, JA McBroom, MM Garrison, MT Parisi: Revised ultrasound criteria for appendicitis in children improve diagnostic accuracy. In: Pediatric radiology. Volume 41, No. 8, 2011, pp. 993-999, doi: 10.1007 / s00247-011-2018-2 .
- ↑ M. Thieme, M. Leeuwenburgh et al .: Diagnostic accuracy and patient acceptance of MRI in children with suspected appendicitis. In European Journal of Radiology. Volume 24, No. 3, 2014, doi: 10.1007 / s00330-013-3044-2 , p. 630.
- ↑ Groß et al .: A rare cause of pain in the right lower abdomen . In: Medical Clinic. March 2009, Volume 104, No. 3, pp. 249-250, doi: 10.1007 / s00063-009-1039-1 .
- ↑ Hole: Emergencies according to key symptoms . Deutscher Ärzte-Verlag, 2006, ISBN 978-3-7691-0424-0 , p. 7.
- ↑ JL Antevil, L. Rivera et al. a .: Computed tomography-based clinical diagnostic pathway for acute appendicitis: prospective validation . In Journal of the American College of Surgeons . Volume 203, Number 6, December 2006, ISSN 1072-7515 , pp. 849-856, doi: 10.1016 / j.jamcollsurg.2006.08.012 , PMID 17116553 .
- ↑ I. Montali, M. von Flue: The acute appendicitis today (PDF) In Switzerland Med Forum. (SMF) Volume 8, No. 24, 2008, pp. 451-455 (PDF 395kByte).
- ^ Wolfram Domschke, Mathias Berger, Werner Hohenberger: Therapy manual for internal medicine. Special edition 2011/2012, Urban & Fischer, Munich 2011, ISBN 3-437-22702-5 , pp. 392–395.
- ↑ Barbara I. Tshisuaka: Fitz, Reginald Heber. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 403.
- ↑ John Blair Deaver: Appendicitis. 3. Edition. P. Blakiston's, Philadelphia 1905, pp. 34-36. ( Text archive - Internet Archive ).
- ↑ a b First US appendectomy: Jan. 4, 1885. healthcentral.com
- ↑ Happy Anniversary: From top has frights to public flirts . independent.co.uk
- ↑ a b Christoph Weißer: Visceral surgery. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 1448 f .; here: p. 1448.
- ↑ Study: Antibiotics often make appendix surgery superfluous . On: spiegel.de from June 17, 2015.
- ↑ Paulina Salminen, Hannu Paajanen, Tero Rautio u. a .: Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis: The APPAC Randomized Clinical Trial. In: The Journal of the American Medical Association . (JAMA) 2015, Volume 313, No. 23, pp. 2340-2348, doi: 10.1001 / jama.2015.6154 .
- ↑ David R. Rosen, Kenji Inaba, Paul J. Oh, Adam C. Gutierrez, Aaron M. Strumwasser: Outpatient Laparoscopic Appendectomy: Feasible in a Public County Hospital? In: Journal of the American College of Surgeons . tape 224 , no. 5 , May 1, 2017, ISSN 1072-7515 , p. 862–867 , doi : 10.1016 / j.jamcollsurg.2017.02.004 ( journalacs.org [accessed May 5, 2017]).