Cataract (medicine)
| Classification according to ICD-10 | |
|---|---|
| H25 | Senile cataract |
| H26 | Other forms of cataract |
| H28 | Cataract and other affections of the lens in diseases otherwise classified |
| Q12.0 | Cataracta congenita |
| ICD-10 online (WHO version 2019) | |
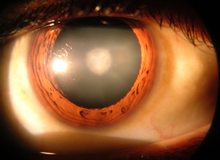
The cataract [ ˌkataˈʁakt ], also known as cataract , describes a clouding of the eye lens . Looking at people who are suffering from an advanced cataract, you can see the gray color behind the pupil see where the term "gray Star " is derived. In most cases, the clouded lens can be surgically replaced with an artificial lens implant .
Word origin
The grammatically masculine word cataract means “ waterfall ” or a “ rapids ” divided by blocks or rock bars and has been in German since the 16th century. Specifically for medical contexts, the borrowed word as part of the language of scholars retained the grammatical gender of female Latin form cataracta , in turn, from the (male) Greek Substantivierung καταῤῥάκτης (ancient Greek pronunciation Katarraktes ), down Dashing ', this to Attic καταῤῥάττειν , katarrháttein , fall down' was borrowed.
In a booklet of eyes created around 1160 in Toledo or Seville, Alkoatim (or Alcoatim) mentions (Suleimān ibn Ḥāriṯ al-Kuwaitī; Arabic سليمان بن حارث القوتي) the substance cataracta , regarded as responsible for the suffering and thought to have dripped down from the brain .
Demarcation
Cataract is not with the glaucoma (glaucoma) to be confused, a number of different eye diseases cause (see Star (Ophthalmology) ).
history
In ancient times, people assumed that when cataracts developed (in the sense of Hippocratic - galenic humoral pathology ) substances would flow down behind the pupil and interfere with the visual process. Here, a cooling and solidification of the brain was held in the nose and eye area as a drop ( gutta cataracta ) dripped excess phlegm (mucus or snot) as the cause. The term star already existed in German in the 8th century and refers to the "solidification" of the mass that has flowed in, which should then be treated with drugs or surgery. Another explanation derives the term “staring”, which is intended to describe the affected person, who is characterized by a stare, as “blind with open eyes”.
Even in pre-Christian times, attempts were made to cure cataracts surgically. The oldest surgical method is the pressing down ( depression ) of the eye lens into the eye using a needle. The star engraving is said to have been known since Babylonian times , but this is controversial. Derived from this is the phrase "stab someone's star" with the meaning "reveal the truth to someone, educate someone about something".
In addition to the surgical-operative approach, conservative treatment approaches based on humoral pathology were also used, for example in a small cataract treatise by a Magister Narcissus , whose diagnostic and therapeutic instructions were put on paper by a Swabian clerk between 1450 and 1475. In an Olomouc drug handbook , like the Narcissus text to be found in a Silesian collective manuscript , written by a surgeon with expertise in ophthalmology, also the conservative star therapy as an externally applied ointment treatment with warming and softening (and thus humoral-pathologically causal against the cold and hard cataract mass effective) intended Marciaton ointment is used.
The French military doctor Michel Brisseau had proven in 1705 that the clouding of the lens is the cause of cataracts and Antoine Maître Jan 1725 also published it. The academic elaboration of this theory, which clarified the true nature of cataracts, was succeeded by Lorenz Heister in 1712 , which led to a long scholarly dispute. The traditional doctrine was based on a cloudy membrane in front of the lens.
In the second half of the 18th century, beginning with Jacques Daviel around 1746, the surgical extraction of the clouded lens replaced the star stitch that had been common up until then. At the end of the 1980s, extracapsular cataract extraction predominated; today, phacoemulsification is mostly used.
Symptoms
The main subjective symptom is a slow, painless loss of visual acuity , especially when the incipient opacity is in the central areas of the lens. The result is blurred vision and increased sensitivity to glare , as the diffuse scattering reduces the image contrast and the patients perceive their surroundings “as if through a fog”.
Occasionally, there will be double monocular vision that will persist when the other eye is closed. Halos or halos are observed around light sources . The light-dark adaptation of the eye is slowed down and spatial vision can be impaired.
In rare cases, there may be a temporary improvement in close-up vision from time to time. The thickening of the lens and the compression of the lens nucleus cause an increasing "myopization" (change in the refractive power towards nearsightedness ). However, this improvement is offset by a corresponding deterioration in distance vision. In addition, this condition is often short-lived because the increasing opacity of the lens decreases visual acuity at all distances.
distribution
As a rule, cataracts only appear with age, but they can develop earlier. The typical "old age star" develops over years, sometimes even in a few months.
The frequency is given as 17% in adults older than 40 years. Age-related cataracts are considered to be the most common cause of visual impairment and blindness .
Congenital forms
There are innate (congenital) forms with a frequency of about 1–6 per 10,000 people that can be found shortly after birth. Metabolic or systemic diseases are the basis in more than 60% .
root cause
The cause of cataracts is often unknown. Ionizing radiation , especially UV radiation , can damage the lens of the eye and thus promote the development of cataracts. Diabetes mellitus , reactions to medication (especially cortisone ), drugs or trauma are also possible causes. Also smoking can promote a cataract development. In the long term, quitting smoking can reduce the need for an operation, especially for male smokers, but it does not reduce the general risk of illness in humans. Vitiligo (white spot disease) can also trigger cataracts. Increased cataract formation is also observed in Siemens bullous ichthyosis .
Exposure to high voltage currents and lightning strikes can cause cataracts. A cataract caused by infrared radiation (fire star, heat star or glassmaker star) in occupations in which very hot materials are processed (blast furnace workers, glass blowers) is recognized as an occupational disease.
Rubella during pregnancy can cause cataracts in the newborn ( rubella embryopathy ). A congenital cataract can also occur with a lack of galactokinase . In cases of congenital cataracts, depending on its severity, the cloudy lens must be surgically removed as early as infancy due to the risk of impending amblyopia . If a cataract occurs in childhood or adolescence, the neurodegenerative disease cerebrotendinous xanthomatosis may also be the cause .
At the molecular level, cataract is a disruption of the arrangement of the crystalline proteins , which are the main substance of the lens of the eye. Current research results show that lanosterol plays a crucial role in maintaining the light-transparent structure. This can be an approach for prophylaxis and conservative therapy .
During the development of a cataract, the lenses have to be adjusted more frequently due to the changing refractive power of the eye . If the patient perceives the reduction in his visual acuity as disturbing and intolerable, even with optimal correction, an indication for surgical removal of the lens and its replacement with an artificial implant is given. There is no known conservative treatment of cataracts. The operation is usually carried out on an outpatient basis , but also as an inpatient if there are additional risks. If an indicated operation is delayed for a long time, the lens will usually become increasingly hardened, making it more difficult and therefore more risky to remove. In addition, the condition can steadily worsen without surgical measures, in some cases even up to blindness.
Classification
In general, the cataract is classified according to the location of the cloudiness.
- In the case of the cortical cataract , the lens cortex becomes cloudy due to so-called water gaps (i.e., fluid-filled vacuoles ). Approximately 50% of old age starlings begin with this lesion pattern.
- The posterior subcapsular cataract (posterior subcapsular cataract) accounts for about 20% of old age starlings . It progresses quickly and vision problems occur early on, especially with nearby vision.
- The nuclear cataract is slowly advancing. There is a brownish cloudiness and an increase in the refractive power. If a patient is already presbyopic , there may be a temporary improvement in visual acuity in the vicinity, which can make reading glasses superfluous for a certain period of time. As the disease progresses, double monocular vision can occur.
Operative therapy (cataract surgery)
Over 650,000 operations are performed in Germany every year in which the clouded lens is replaced by an artificial lens implant . They are among the most frequently performed surgical interventions. Until a few years ago, the main indication for cataract surgery was significantly reduced visual acuity to around 0.3 and worse. Today, subjective impairments of the patient, such as greatly increased sensitivity to glare or reduced vision in twilight, are recognized as sufficient reasons to undertake an appropriate intervention.
Not having a cataract operation if the eyesight is impaired could not only reduce the quality of life but also increase mortality . At least that was shown by an Australian study that looked at two groups who either had an operation or refused to do it. At first glance, the differences were small, but when age, other health status, lifestyle and much more were taken into account, a significantly increased mortality rate was observed in those who did not undergo cataract surgery despite impaired vision. Reasons for the increased mortality could be increased risk behavior with a lower quality of life, mistakes in taking medication and falls.
Around 90% of cataract operations in Germany are performed on an outpatient basis. Reasons for an inpatient stay are lack of home care for drip therapy, poor general condition, difficult initial situations with concomitant ophthalmic diseases (e.g. glaucoma ) or operations on the only eye (oculus ultimus).
anesthesia
General anesthesia and sedation
A cataract operation under general anesthesia (general anesthesia ) or (anal) sedation is rarely indicated by the ophthalmologist, in Germany currently in around 16% of cases. In children and patients with involuntary movements (e.g. in Parkinson's disease or restless legs syndrome ) or mental disorders, however, anesthesia can sometimes make the procedure possible in the first place. Other reasons can be foreseeable intraoperative difficulties that could force an extension of the procedure. Often, however, it is the patient's wish that leads to an operation under anesthesia. The anesthesia and the surgical procedure must be discussed in detail with the patient preoperatively depending on previous and concomitant diseases of the eye, previous operations, as well as any existing risks and expected complications.
Local anesthesia
In the vast majority of cases, cataract surgery is performed under local anesthesia. The analgesia can be improved by using additional intravenous narcotics.
Topical anesthesia (drops only)
Most (43% of all cases) operations in Germany are carried out under anesthetic drip, in which the anesthetic is dripped onto the surface of the eye before and during the procedure. The anesthesia is intensified by administering gels containing anesthetics to the eye during the operation (visco anesthesia). Almost complete freedom from pain can be achieved. The patient should be able to focus straight ahead as possible. An important advantage of drip anesthesia is that an injection next to or behind the eye with the risk of bruising is not carried out. For this reason, it is particularly preferred for the many patients who are on therapy with anticoagulant drugs ( ASA , Marcumar , DOAK ).
Infiltration anesthesia with injection (syringe)
The classic method is retrobulbar anesthesia, in which the anesthetic is injected behind the eye. Ideally, the eye is not only completely painless, but can no longer be actively moved. Some surgeons combine retrobulbar anesthesia with a facial block. A short-term paralysis of the orbicularis oculi muscle is generated by means of another syringe at the outer corner of the eyelid or near the ear. The aim here is to prevent the eyelids from closing unintentionally with increasing vitreous pressure during the operation.
Due to the possible complications of retrobulbar anesthesia, which include perforation of the eye, damage to the optic nerve and eye muscles, there are many surgeons who inject next to the eye (deep layers next to the eye muscles: parabular anesthesia or only in the anterior areas of the eye; subtenonal anesthesia or subconjunctival anesthesia) . This reduces the risks of the injection, but also reduces the effects on the mobility of the eye during the procedure. In contrast to pure retrobulbar anesthesia, lidakinesia with an additional syringe is not necessary.
Accompanying measures
Ocular compression
A so-called oculopression can be carried out with all stunning methods. Before the operation, continuous pressure is applied to the eyeball over a period of a few minutes using a balloon . The aim is to counter possible risks during the procedure, such as increased vitreous pressure and flattening of the anterior chamber. The ocular compression can reduce intraocular pressure by up to 10 mmHg by reducing the vitreous volume. On the other hand, short-term pressure increases of up to 50 mmHg can arise in the process, which in a previously damaged eye, e.g. B. glaucoma , can lead to irreversible damage. For this reason, the ocular compression is only performed in appropriately indicated cases.
Endophthalmitis prophylaxis
To avoid severe postoperative infections of the inside of the eye ( endophthalmitis ), an antibiotic is administered into the anterior chamber by the surgeon after around 50% of the operations .
Techniques and Procedures
There are three different approaches:
Intracapsular cataract extraction
The only used in exceptional cases intracapsular cataract extraction is on the outer edge of the cornea ( cornea ) or the adjacent dermis ( sclera to make a long incision) and the whole lens with the lens capsule, d. H. their outer shell.
Phacoemulsification
Nowadays, the standard procedure after circular opening (diameter approx. 5 mm) of the anterior capsule leaf is to smash the lens using ultrasound while protecting the rest of the capsule ( phacoemulsification ) and suck it off. An artificial lens is then inserted into the then empty capsular bag. These artificial lenses are - in contrast to the acrylic glass lenses, which were exclusively used up to 10 to 15 years ago - usually made of elastic materials (e.g. silicone or acrylic plastics) so that they can be folded or rolled through a 2.5 to 3 mm cut at the edge of the Insert the cornea, after which it unfolds in the capsular bag and self-centering and fixing using two elastic brackets (haptics).
Femtosecond laser cataract surgery
Since 2008 there has been a new procedure in cataract surgery, the femtosecond laser cataract surgery , which was first described by Zoltán Zsolt Nagy (Budapest). The femtosecond laser , which has been used in ophthalmology for several years for refractive corneal operations, is now being used in more and more surgical centers and takes on two steps of the operation that are otherwise performed manually by the surgeon: opening the anterior capsule (capsulotomy) and the Disassembly (fragmentation or pre-fragmentation) of the lens. Possible advantages of femtosecond laser cataract surgery over conventional phacoemulsification are the significantly more precise incision and, above all, the fact that after the lens has been dismantled with the laser, far less - or no - ultrasound energy is required (this can include the sensitive inner Layer of the cornea, the endothelium). At specialized centers, more than 90% of cataract operations with the femtosecond laser can now be operated without ultrasound (zero phaco) . In 2013, children with congenital cataracts were successfully operated on with the femtosecond laser for the first time. Disadvantages named include a longer operation time, the exclusion of certain patient groups and the high costs of the own.
Use of artificial lenses
Without an adequate replacement in the form of a lens implant, so-called intraocular lenses , one would generally see the world blurred after the lens removal, since the eye would then be around 16 to 18 diopters farsighted. Such a aphakia ( aphakia ) can use a contact lens or - also be corrected by a subsequent (secondary) artificial lens implantation - in appropriate cases. So-called star glasses are seldom considered and only when other procedures cannot be carried out.
After removing the natural lens, the eye can no longer adjust ( accommodate ) to different viewing distances . Therefore, for reading, as in the case of presbyopia ( presbyopia a) reading glasses required. In particular for young patients who still had a full capacity for accommodation up to the operation, the loss of this definitely represents a reduction in the quality of life. The subject of current research is therefore on the one hand artificial lenses which are intended to replace a certain capacity for accommodation of the eye. However, the results so far should be viewed with caution. Multifocal intraocular lenses (implanted varifocal lenses) offer the possibility of living a "life without glasses" if the disadvantages in the form of weak double images and reduced contrast vision are accepted. On the other hand, by selecting the appropriate lens implants, a state of anisometropy can be brought about, which enables one eye to see clearly in the distance and the other closer to it ( monovision or Goethe gaze ). However, two-eyed and thus spatial vision is only possible to a limited extent.
The insertion of intraocular lenses opens up the possibility of correcting defective vision ( ametropia ). This is an additional advantage for high refraction values. In pronounced cases, however, from a medical point of view, it is usually unavoidable to operate both eyes in quick succession, as symptoms can be expected from an anisometropia (difference in refractive power between the two eyes) of around three diopters. Before the operation, the patient has to decide whether he wants to live without distance glasses but with reading glasses after the operation, or vice versa, so that the appropriate strength of the artificial lenses can be selected. Toric intraocular lenses are also available to correct astigmatism. If both eyes have to be operated on, the interventions should be carried out a few weeks apart, in individual cases a few days.
Post-operative follow-up care
After the operation, the operated eye is covered with a bandage, usually a watch glass bandage , which is removed for the first time the next day if the course is uneventful. 90% of patients can see better after the operation than before: Most patients' first impression is that they see colors much more vividly than before and that the overall picture is brighter or even slightly dazzling. Depending on the choice of correction, it is then determined that one can see sharply either close up or in the distance without glasses. However, eyesight may still be reduced if another eye disease such as AMD is present.
Antibiotic and anti-inflammatory eye drops are given for about three to four weeks . In some cases, nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid drops are also used. Depending on the healing process, two, three or more ophthalmological checks are carried out; Postoperative visual impairment, flashes of light, severe redness or persistent pain are considered an emergency. Any pressure on the eye should be avoided, including the entry of soap, shampoo, make-up or similar in the first few weeks, as well as visits to swimming pools, saunas and heavy lifting. After the operation, it usually takes up to eight weeks for the healing process to complete and for a stable situation to be established that allows new lenses to be fitted. Active participation in road traffic is only permitted after a visual test and medical consultation.
A new method of cataract surgery is the insertion of the so-called light-adjustable lens (LAL). With this lens, the refractive power can be readjusted after the operation by irradiation with UV light.
Complications
Despite very rare cases of blindness, the complication rate in cataract operations is now relatively low at less than 1%. Possible complications include infection inside the eye, endophthalmitis , injury to the posterior lens capsule with subsequent vitreous herniation, swelling of the middle of the retina (cystoid macular edema ) and clouding of the posterior lens capsule (cataract).
It is controversial whether the risk of a later retinal detachment after (complication-free) cataract surgery is significantly increased. Some studies indicate an increased risk for young, male, or nearsighted patients and in the event of vitreous loss during surgery.
It is undisputed that the surgical procedure regularly disrupts the so-called blood-aqueous humor barrier .
In cataract operations that are judged to be successful, patients often report (dys) photopsias . A very small proportion of the patients feel that this affects themselves in the long term. Positive photopsia are reflections or ghost images, negative photopsia are dark shadows in the field of vision. Their causes have not been conclusively clarified. It is assumed that positive dysphotopsias can arise, for example, "through multiple reflections on the front and rear surfaces of the lens, the edge of the lens or through a direct light path through the iris and past the edge of the lens". Negative dysphotopsias, especially in the temporal field of vision, are common after cataract surgery. The declaration includes: a. slight change in the image scale due to the new lens, which could lead to “a slight shift in the object space corresponding to the blind spot and the central vessels”.
Post-cataract
As a result of a cataract operation, after a few months, but not infrequently even after years, the posterior lens capsule can become cloudy with a corresponding deterioration in vision. This so-called secondary cataract (cataracta secundaria) used to develop in up to 50% of the operated eyes. However, modern lens designs and surgical procedures have reduced the post-cataract rate to less than 4% on average. This is a clouding of the posterior lens capsule either as a result of connective tissue transformation of the capsule (fibrotic form) or due to the proliferation and spread of lens cells remaining from the operation on the capsule (regenerative form).
The cataract is treated painlessly with a small outpatient procedure. After the pupil has been dilated with medication ( mydriasis ), the posterior lens capsule is opened by a capsulotomy with several pulses from an Nd: YAG laser so that the incident light can again reach the retina unhindered. Alternatively, the cataract can be treated surgically (so-called cataract suction).
History of cataract surgery in modern times
With a sometimes decorated cataract needle was in Europe from Star engravers of the limbus of the 17th century temporal inserted and pressed the cloudy lens down and back into the vitreous. Common complications were infections and glaucoma . Jacques Daviel (1696–1762) removed the lens from 1745 after an arcuate corneal incision from the eye. Albrecht von Graefe introduced the narrow star knife in the second half of the 19th century and improved the cut with the intention of reducing the complication rate. The introduction of antisepsis from 1870 onwards brought decisive progress. The introduction of cocaine for local anesthesia on the eye in 1884 by Koller brought great relief for the patient and the surgeon. While the contents of the lens were previously removed from the capsule (extracapsular lens extraction), Anton Elschnig developed intracapsular (ic) extraction at the beginning of the 20th century. H. Removal of the lens in the capsule from the eye. Cataract surgery - with modifications such as suction or freezing of the lens ( cryo-extraction ) or enzymatic breakdown of the zonula fibers ( zonulolysis ) - was carried out in this way until the end of the 1960s.
The observation during World War II that acrylic glass splinters from shot-up aircraft cockpits were tolerated without reaction in the eyes of pilots led to the development of acrylic lenses after the war. However, due to incompatibility, these had to be removed again - in some cases by eye. As it turned out later, the incompatibility was a result of the further development of acrylic glass through chemical additives. With this knowledge, compatible artificial lenses could then be constructed.
(Source below)
Veterinary medicine
Surgical replacement of cloudy lenses with an implant is also possible in animals and has been the therapy of choice in many cases for years. For example, at the University of Wisconsin-Madison School of Veterinary Medicine, cataract surgery was performed on a blind eagle owl .
In domestic dogs , cataracts are the most common cause of blindness. Hereditary forms of cataract affect over 100 breeds . An autosomal recessive inheritance is present in Bichon Frize , Boston Terriers , Staffordshire Bull Terriers and Miniature Schnauzers ; in Australian Shepherds , the cataract is inherited as an autosomal dominant trait. A mutation of the HSF4 gene was found to be the cause in the Australian Shepherd, and this gene is also the cause in Staffordshire Bull Terriers, Boston Terriers and French Bulldogs , albeit in a different locus .
literature
- Theodor Axenfeld (founder), Hans Pau (ed.): Textbook and atlas of ophthalmology. With the collaboration of R. Sachsenweger u. a. Gustav Fischer Verlag, Stuttgart 1980, ISBN 3-437-00255-4 .
- Albert J. Augustin: Ophthalmology . Springer Verlag, Berlin 2007, ISBN 978-3-540-30454-8 .
- David Allen, Abhay Vasavada: Cataract and surgery for cataract . In: BMJ. 2006 Jul 15; 333 (7559), pp. 128-132. Review, PMID 16840470
- J. Albrecht: Cataract formation in ichthyosis Bullosa Siemens. In: Alexander Meves: Dermatology intensive course. Urban & Fischer, Munich 2006, ISBN 3-437-41162-4 , p. 171.
- Burkhard Dick , Ronald D. Gerste, Tim Schultz: Femtosecond Laser in Ophthalmology. Thieme, New York 2018, ISBN 978-1-62623-236-5 .
- Otto Hockwin: On the pathogenesis and therapy of old age cataract: historical aspects and new ideas. In: Historia ophthalmologica internationalis 2, 1981, pp. 115-131.
- Gundolf Keil : "blutken - bloedekijn". Notes on the etiology of the hyposphagma genesis in the 'Pommersfeld Silesian Eye Booklet' (1st third of the 15th century). With an overview of the ophthalmological texts of the German Middle Ages. In: Specialized prose research - Crossing borders. Volume 8/9, 2012/2013, pp. 7-175.
- Jens Martin Rohrbach: What is a cataract and when should its operation be indicated? An opinion. Clinical monthly sheets for ophthalmology 2019, 236, pp. 1346-1349
Web links
- Cataract - Friedrich Schiller University Jena
- Cataracts (cataracts) in adulthood (PDF; 103 kB) Guideline No. 19 of the Professional Association of Ophthalmologists in Germany (BVA)
- Cataract (cataract) surgery in adulthood . Guideline No. 19a of the Professional Association of Ophthalmologists in Germany (BVA)
- Cataracts , informedhealth.org, Institute for Quality and Efficiency in Healthcare (IQWiG), 25th September 2019
Individual evidence
- ↑ a b Kluge: Etymological dictionary of the German language . 24th edition.
- ↑ cataract. on: dictionary.reference.com (English) (compare also the catarrh ).
- ^ Karl Felsch: Die Augenheilkunde des Alcoatim (1159) translated into German for the first time and accompanied by comments. Medical dissertation, Friedrich-Wilhelms-Universität zu Berlin 1898.
- ↑ Friedrich Schlepckow: Ophthalmology of Alcoatim from the year 1159, part III. Translated into German for the first time and annotated. Medical dissertation Berlin 1899.
- ↑ Gundolf Keil (2012/2013), p. 14, note 70.
- ↑ Gundolf Keil (2012/2013), p. 14, note 70, and p. 67–76.
- ↑ Frank Krogmann: Star, grayer (cataract). In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil, Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1355.
- ↑ a b Klaus Müller (ed.): Lexicon of speeches. Orbis, Niedernhausen / Ts. 2001 (Original: Bertelsmann, Munich), ISBN 3-572-01296-1 , p. 573.
- ^ Franz Krogmann: Star operation. In: Werner E. Gerabek u. a. (Ed.): Encyclopedia of medical history. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 1356 f.
- ↑ Omid Kermani: Defining dysfunctional lens syndrome. Clinical entity of DLS has been overlooked, inadequately characterized. In: Ophthalmology Times Europe , Vol. 13, No. 3 (April 2017), p. 6.
- ↑ A. Peters: The pathology of the lens. In: O. Lubarsch u. a. (Ed.): Results of the general pathology and pathological anatomy of humans and animals. Springer, Berlin 1933, pp. 1–120, here: p. 31 ( Google Books ).
- ^ Bernhard Dietrich Haage, Wolfgang Wegner, Gundolf Keil, Helga Haage-Naber: German specialist literature of Artes in the Middle Ages and early modern times. Berlin 2007 (= Basics of German Studies. Volume 43), p. 206 f.
- ↑ The Marciaton ointment is already used by Aëtios , Alexander von Tralleis and Paulus von Aegina and is also recorded in the Antidotarium Nicolai as unguentum marciaton . Cf. Gundolf Keil: The "Cirurgia" Peters von Ulm. Investigations into a memorial of old German specialist prose with a critical edition of the text. (= Research on the history of the city of Ulm. Volume 2). Stadtarchiv, Ulm 1961 (also philosophical dissertation Heidelberg 1960), p. 421.
- ↑ Gundolf Keil (2012/2013), pp. 11–16, 46.
- ↑ Aloys Henning: On the paradigm shift in cataract surgery, especially in Berlin from 1755. In: Würzburger medical history reports. Volume 18, 1999, pp. 271-296, here: pp. 276-280.
- ↑ Axel W. Bauer : Therapeutics, Therapy Methods. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil, Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , pp. 1388-1393, here: p. 1390.
- ^ Alfred Bader: Development of ophthalmology in the 18th and 19th centuries. With special consideration of Switzerland. Benno Schwabe & Co., Basel 1933.
- ^ Julius Hirschberg: History of ophthalmology . In: Handb.d, general ophthalmology . tape 14 . Engelmann, Leipzig 1912.
- ↑ Anselm Kampik: Osteopathic Therapy , Georg Thieme Verlag, 2002, ISBN 978-3-13-128411-2 . P. 164 .
- ↑ emedicine Senile Cataract
- ↑ Emedicine Congenital Cataract
- ↑ Birgitta Ejdervik Lindblad, Niclas Håkansson, Alicja Wolk: Smoking Cessation and the Risk of Cataract. In: JAMA Ophthalmology. 2014; 132 (3), pp. 253-257. doi: 10.1001 / jamaophthalmol.2013.6669 .
- ^ Roche Lexicon Medicine. Urban & Fischer at Elsevier, 2003, ISBN 3-437-15150-9 .
- ↑ Verrips et al .: Clinical and molecular genetic characteristics of patients with cerebrotendinous xanthomatosis. In: Brain . 2000, doi : 10.1093 / brain / 123.5.908 ( oup.com ).
- ↑ Ling Zhao, Xiang-Jun Chen, Jie Zhu, Yi-Bo Xi, Xu Yang, Li-Dan Hu, Hong Ouyang, Sherrina H. Patel, Xin Jin, Danni Lin, Frances Wu, Ken Flagg, Huimin Cai, Gen Li , Guiqun Cao, Ying Lin, Daniel Chen, Cindy Wen, Christopher Chung, Yandong Wang, Austin Qiu, Emily Yeh, Wenqiu Wang, Xun Hu, Seanna Grob, et al .: Lanosterol reverses protein aggregation in cataracts . In: Nature . July 2015, doi : 10.1038 / nature14650 ( online ).
- ^ Johannes Patzelt: Ophthalmology Munich 2005, ISBN 3-437-42126-3 , p. 53.
- ↑ Cataract surgery: Risk of bleeding reduced with oral anticoagulation . In: Dtsch Arztebl. 2005; 102 (1-2), pp. A-58 / B-49 / C-46
- ↑ Information document. ( Memento from June 25, 2012 in the Internet Archive ) (PDF; 401 kB) Federal Association of Ophthalmologists in Germany BVA
- ↑ Calvin Sze-un Fong, Paul Mitchell, Elena Rochtchina, Erdahl T. Teber, Thomas Hong, Jie Jin Wang: Correction of Visual Impairment by Cataract 'Surgery and Improved Survival in Older Persons. In: Ophthalmology. 120, 2013, pp. 1720-1727. doi: 10.1016 / j.ophtha.2013.02.009 .
- ↑ a b c d Martin Wenzel, H. Burkhard Dick, Armin Scharrer, Kaweh Schayan, Thomas Reinhard: Outpatient and inpatient intraocular surgery 2016 results of the current survey by DGII, DOG, BVA and BDOC . In: OPHTHALMO SURGERY . tape 29 , 2017, p. 185-194 .
- ↑ Local anesthesia in ophthalmic surgery. Retrieved December 27, 2017 .
- ↑ Volker Hessemer: Peribulbar anesthesia versus retrobulbar anesthesia with facial block - techniques, local anesthetics and additives, akinesia and sensitive blocks, complications. In: Thieme eJournal from "Clinical Monthly Ophthalmology 1994". 204 (2), pp. 75-89, doi: 10.1055 / s-2008-1035503 .
- ↑ ZZ Nagy: New technology update: femtosecond laser in cataract surgery. In: Clinical Ophthalmology. June 2014; 8, pp. 1157-1168.
- ↑ Burkhard Dick, Ronald D. Gerste, Tim Schultz: Femtosecond Laser in Ophthalmology. Thieme, New York 2018, ISBN 978-1-62623-236-5 .
- ↑ KE Donaldson et al. a .: Femtosecond laser-assisted cataract surgery. In: Journal of Cataract and Refractive Surgery. 2013; 39, pp. 1753-1763.
- ^ HB Dick , T. Schultz: On the way to zero phaco. In: Journal of Cataract and Refractive Surgery . 2013; 39, pp. 1442-1444.
- ^ HB Dick , T. Schultz: Femtosecond laser-assisted cataract surgerz in infants. In: Journal of Cataract and Refractive Surgery. 2013; 39, pp. 665-668.
- ↑ HB Dick, T. Schultz: Femtosecond laser-assisted cataract surgery . In: The ophthalmologist . tape 111 , no. 7 , July 2014, p. 614-623 , doi : 10.1007 / s00347-014-3033-0 .
- ↑ Werner Bachmann, Ophthalmic Cooperative Westphalia eG: Billing recommendation for cataract surgery using femtosecond laser. (PDF) (No longer available online.) Archived from the original ; accessed on April 26, 2018 .
- ↑ a b Freiburg University Hospital: Cataract surgery and intraocular lens (PDF)
- ↑ Christoph Martin Lwowski, Adonis Chedid de Robaulx, Thomas Kohnen: Peri- / Postoperative anti-inflammatory therapy after cataract surgery and refractive surgery . In: Clinical monthly sheets of ophthalmology . tape 236 , no. 5 , 2019, p. 636-646 , doi : 10.1055 / a-0877-7221 ( thieme-connect.de ).
- ^ T. Kohnen, M. Baumeister, D. Kook, OK Klaproth, C. Ohrloff: Cataract surgery with implantation of an artificial lens . In: Dtsch Arztebl Int. tape 106 , no. 43 , 2009, p. 695-702 ( aerzteblatt.de ).
- ^ T. Kohnen, M. Baumeister, D. Kook, OK Klaproth, C. Ohrloff: Cataract surgery with implantation of an artificial lens . In: Dtsch Arztebl Int. tape 106 , no. 43 , 2009, p. 695-702 ( aerzteblatt.de ). Quoted by: Aqua-Institut, Cross-Sectoral Quality Assurance in Health Care (PDF; 962 kB) Cataract Surgery, Final Report October 18, 2010, accessed on October 3, 2012, p. 19.
- ^ MH Qureshi, DHW Steel: Retinal detachment following cataract phacoemulsification-a review of the literature . In: Eye (London, England) . October 2019, doi : 10.1038 / s41433-019-0575-z , PMID 31576027 .
- ^ W. Herrmann, H. Helbig, H. Heimann: [Pseudophakic retinal detachment] . In: Clinical monthly sheets for ophthalmology . tape 228 , no. 3 , March 2011, p. 195-200 , doi : 10.1055 / s-0029-1246116 , PMID 21374539 .
- ^ Ives CA Robert, Balder Gloor, Christian Hartmann, Rainer Rochels: 7th Congress of the German-speaking Society for Intraocular Lens Implantation . Springer-Verlag, 2013. p. 57. ISBN 978-3-642-50183-8 .
- ↑ Michelle Stephenson: Dysphotopsia: Not Just Black and White. In: Review of Ophthalmology. November 7, 2017, accessed November 9, 2019 .
- ↑ Stefan Palkovits, Oliver Findl: Pseudophakic Dysphotopsien . In: Spectrum of Ophthalmology . No. 6/2016 ( springermedizin.at ). Summary.
- ↑ Jonathan M. Davidorf, Kevin M. Miller and Steven I. Rosenfeld in an interview with Linda Roach: Shedding Light on Pseudophakic Dysphotopsia . In: American Academy of Ophthalmology (Ed.): EyeNet Magazine . December 2014 ( aao.org ).
- ↑ Achim Langenbucher: Ghost images and shadows - optical phenomena after cataract surgery. (PDF) In: 27th Fielmann Academy Colloquium. 2014, accessed November 9, 2019 . . Pp. 2-4.
- ↑ Martin Wenzel, Achim Langenbucher, Timo Eppig: Causes, diagnosis and therapy of negative dysphotopsia . In: Clinical monthly sheets of ophthalmology . tape 236 , no. 6 , 2019, pp. 767-776 , doi : 10.1055 / s-0043-112855 ( thieme-connect.com [PDF]).
- ↑ Post-cataract. Charité, Universitätsmedizin Berlin, 2020, accessed on February 18, 2020 .
- ↑ R. Stanka: The bacteriological prophylaxis before ocular opening operations . Clinical monthly sheets for ophthalmology Volume 72, 1924, p. 432.
- ↑ A. Elschnig: The intracapsular starling extraction , manual of the entire ophthalmology, ed. Th. Axenfeld, A. Elschnig, 2. u. 3. Edition. Springer, Berlin 1932.
- ^ RF Moore: A modified suction cataract extraction . British Journal of Ophthalmology, Vol. 7, 1923 p. 233.
- ↑ Hugh P. Williams: Sir Harold Ridley ’s vision . In: British Journal of Ophthalmology , Vol. 85, pp. 1022-1023.
- ^ Alfred Bader: Development of ophthalmology in the 18th and 19th centuries. With special consideration of Switzerland. Benno Schwabe & Co., Basel 1933.
- ↑ Cataract: Star meets owl. euro-focus.de, February 13, 2004; Retrieved October 3, 2013.
- ↑ Cathryn S. Mellersh, Bryan McLaughlin, Saija Ahonen, Louise Pettitt, Hannes Lohi, Keith C. Barnett: Mutation in HSF4 is associated with hereditary cataract in the Australian Shepherd. In: Veterinary Ophthalmology. 12, 2009, pp. 372-378, doi: 10.1111 / j.1463-5224.2009.00735.x .
- ↑ Christina Julia Rabe: Cataloging of phenotypes, genotypes and genetic tests of genetic defects characterized by molecular genetics in domestic dogs (Canis familiaris). Dissertation . Munich 2009, pp. 125–129. uni-muenchen.de (PDF)
- ↑ Elaine A. Ostrander : Genetics of the Dog. CABI, 2012, p. 219.