Graves disease
| Classification according to ICD-10 | |
|---|---|
| E05.0 | Hyperthyroidism with diffuse goiter - Graves disease (Graves disease) |
| ICD-10 online (WHO version 2019) | |
Graves' disease (also Basedow's disease , of Latin morbus "disease"), Basedow's disease or Graves' disease (English Graves' disease ) is a well Immunhyperthyreose said autoimmune disease of the thyroid . The disease leads to an excessive production of thyroid hormones ( hyperthyroidism, hyperthyroidism ) and is often associated with an enlarged thyroid gland ( goiter ) or involvement of the eyes ( endocrine orbitopathy ).
While in some of the cases the disease comes to a standstill within one to one and a half years under bridging drug therapy ( remission ), in the majority of cases treatment by surgery ( goiter resection ) or radioactive therapy ( radioiodine therapy ) is necessary.
Synonyms
In the German-speaking area, the disease is named after Carl Adolph von Basedow (1840), the first German person to describe it . In English-speaking countries, the disease is referred to as Graves' disease after the Irish first descriptor Robert James Graves (1835) . Other names are autoimmune thyroid disease type 3, immune thyroid disease or immune hyperthyroidism (IHT). Graves disease is also known in the literature under the names Begbie's disease , Flajani's disease , Flajani-Graves syndrome , Marsh's disease or Parry’s disease .
history
The first descriptions of the disease come from Giuseppe Flajani (1802), Caleb Hillier Parry (1825) and RJ Graves (1835). In 1840 , the doctor Carl von Basedow , who worked in Merseburg , described the constellation of symptoms of exophthalmos , goiter and tachycardia, later known as the Merseburg triad . He interpreted it as "masked scrofulous dyscrasia of the blood" (dyscrasia: according to Hippocrates, incorrect composition of the body fluids ). He treated the syndrome with mineral water containing iodine . Robert James Graves had already described this symptom combination in 1835 and interpreted it as a disease of the heart. In 1886, Paul Julius Möbius demonstrated that the syndrome was related to an overactive thyroid .
Among the surgeons who dealt with Graves' disease were Theodor Billroth , who performed major goiter operations from 1862, Theodor Kocher , who published the connection between goiter resection and subsequent hypothyroidism in 1883 (and received the Nobel Prize for his thyroid research in 1909), as well as at the beginning of the 20th century Johann von Mikulicz and Ferdinand Sauerbruch in Breslau .
In 1942, S. Hertz and A. Roberts first used radioiodine therapy for Graves' disease. Edwin B. Astwood described in 1943 the therapy of the disease with the thyrostatic drug 2-thiouracil .
distribution
There is no precise information on the frequency ( prevalence ) of Graves' disease in Germany. For countries with an adequate iodine supply, the frequency in women is given as two to three percent, for men with about a tenth of it. The annual new disease rate ( incidence ) is one per 1000 inhabitants.
Graves' disease often affects women of childbearing age. The disease can occur at any age, a third of the cases occur before the age of 35, the maximum is between the ages of 20 and 40. In countries with a good iodine supply (such as the USA), Graves' disease is the most common cause of hyperthyroidism in over 95% of cases , whereas thyroid autonomy is more common in countries with a poor iodine supply . The simultaneous occurrence of Graves disease and thyroid autonomy is called Marine-Lenhart syndrome ; the frequency is given as one percent (for patients with Graves' disease).
In the case of Graves' disease, even newborns can have hyperthyroidism and goiter in their mother because the triggering immunoglobulins ( TSH receptor autoantibodies ) cross the placenta. In the case of manifest illness after the newborn phase, growth and bone aging are accelerated.
Pathophysiology
Basedow's disease is based on several factors. On the one hand, there is a genetically determined defect in the immune system ; on the other hand, it is intensified by certain external influences ( psychosocial, emotional or physical stress , environmental influences (smoking), (virus) infections); however, no specific triggers are known. Ultimately, the self-tolerance to antigens of the thyroid gland breaks down , resulting in an autoimmune disease .
The autoantibodies formed by the body against the thyroid tissue ( immunoglobulins of the IgG class ) bind to the receptor for thyrotropin (thyroid-stimulating hormone, TSH). TSH is the hormone that is produced by the pituitary gland as part of the thyrotropic control loop .
The TSH receptor antibodies ( TRAK ) have an intrinsic activity on the TSH receptor and therefore stimulate the follicular epithelial cells of the thyroid gland. The iodine uptake in the thyroid gland is increased, the thyroid hormones triiodothyronine (T 3 ) and thyroxine (T 4 ) are increasingly produced and released. The result is an overactive thyroid ( hyperthyroidism ). The growth of the thyroid gland is stimulated, which is why the thyroid gland often increases in size ( goiter ).
However, there are also TSH receptor antibodies without a stimulating effect and those with a blocking effect. A change in the quantitative composition of these antibodies leads to changes in the clinical course of the disease.
The histopathological signs of the disease are lymphocytic infiltrates in the thyroid, but also in the eye muscles and subcutaneous tissue .
Graves' disease is associated with the HLA- DR3 antigen . As an HLA-DR3-associated autoimmune disease, it occurs frequently together with other autoimmune diseases such as type 1 diabetes mellitus , type A gastritis , myasthenia gravis , lupus erythematosus , Werlhof's disease , vitiligo , Addison's disease and rheumatoid arthritis .
There is evidence that a certain genotype (MICA A5.1 / A5.1) favors the onset of the disease, while another genotype (MICA A6 / A9) has a more protective effect.
Clinical picture
Graves disease manifests itself on the thyroid gland and outside the thyroid gland. The time at which the symptoms start is often given quite precisely by the patient and typically coincides with external stress (e.g. exams, deaths in the area or special occupational stress).
In the thyroid gland, the autoantibodies cause an overactive thyroid gland ( hyperthyroidism ) and an enlargement of the thyroid gland ( goiter ).
Typical symptoms of hyperthyroidism are insomnia, irritability, nervousness and tremors (subtle tremor ), sinus tachycardia , extrasystoles , atrial fibrillation , weight loss despite cravings , heat intolerance, sweating, warm damp skin, increased stool frequency, weakness of the muscles, osteoporosis and temporary infertility up to and including menstrual disorders .
If there is a clear goiter, the patients often complain of a feeling of pressure, tightness or lump in the throat, abnormal sensations when wearing a tight collar, difficulty swallowing or shortness of breath when exercising.
The most common form of manifestation of Graves' disease outside the thyroid gland is endocrine orbitopathy (EO), which in its most noticeable form can present itself as protruding eyeballs ( exophthalmos ). When looking down, as the Berlin ophthalmologist Albrecht von Graefe observed, the upper eyelid remains behind ( Graefe sign ). The information on the frequency of EO varies. Subclinical EO can be determined in almost all patients with Graves' disease with subtle diagnostics ( ultrasound , magnetic resonance imaging , recording of eye movements ) . It occurs in about 60% of cases together with hyperthyroidism, less often during therapy and very rarely before the hyperthyroidism. Common antigens of the orbital tissue and the thyroid tissue are suspected to be the cause of the endocrine orbitopathy . Immigrating lymphocytes activate existing fibroblasts , which leads to an accumulation of mucopolysaccharides , which are responsible for the formation of edema and thickening of the fat and muscle tissue behind the eyes. The same causes are also assumed for pretibial myxedema as a further form of manifestation, the frequency of which is given as two to three percent. The Acropachyderma (formation of new bone at the finger joints) is a very rare phenomenon in Graves' disease.
Diagnosis and findings
The diagnosis "Graves' disease" can often be made from the typical symptoms (overactive thyroid with eye involvement).
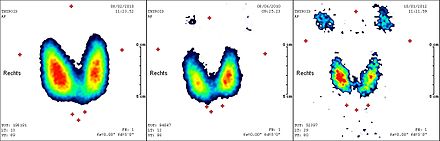
In the ultrasonic echo poverty of the thyroid tissue with a significant non-uniformity ( "inhomogeneity") and generally increased volume seen in Graves' disease. The Doppler sonography shows an increased blood supply to the entire thyroid gland as an expression of inflammation and increased metabolism. In the thyroid scintigraphy is - due to the stimulation of thyroid cells at the TSH receptor - an increased uptake ( uptake ) of the tracer ; usually is the technetium - uptake (normal: 0.5 to 2%) over 5%.
In most cases the laboratory results confirm the diagnosis: fT4 and fT3 in the serum are increased, the TSH is correspondingly decreased in the thyrotropic control loop . Positive TSH receptor autoantibodies (TRAK) are evidence for Graves' disease. In the case of negative TRAK, positive TPO-Ab or Tg- Ab can also support the diagnosis. Autoimmune hyperthyroidism with negative autoantibody status and no signs of endocrine orbitopathy is extremely rare .
Differential diagnosis
In the differential diagnostic differentiation from hyperthyroidism in the case of thyroid autonomy , the sudden onset, the presence of endocrine orbitopathy or myxedema, a rather diffuse goiter and young age indicate Graves' disease, while a gradual onset of hyperthyroidism symptoms, the absence of eye complaints and the presence of thyroid nodules older age are more likely to be found in autonomy.
A thyroiditis de Quervain may be associated with a hyperthyroid laboratory constellation because of destroyed cells, the hormone is released. In contrast to Graves' disease, there is mainly a hard, painful, palpable thyroid gland, fever and a feeling of illness. As a rule, these diseases must therefore be clinically differentiated from one another. De Quervain's thyroiditis is characterized by an increased rate of sedimentation of the blood cells , a typical ultrasound image and reduced perfusion of affected areas in the ultrasound. A reduced uptake would be found in the scintigram .
A hyperthyroid phase in Hashimoto's thyroiditis is often difficult to differentiate at the beginning, but in the long term it is easy to handle in the long-term from hypothyroidism .
Differential diagnostic problems can be caused by thyroid hormone resistance, in which both TSH and peripheral thyroid hormones can be elevated. In the case of this genetically determined variant of the norm, the family history often helps, and those affected usually have no complaints. A TSH-producing pituitary tumor very rarely leads to an overactive thyroid; here too, the increased TSH is noticeable.
Numerous other, rare forms of hyperthyroidism exist.
Treatment and prognosis
The need for immediate drug treatment usually arises from the pronounced overactive thyroid gland ( hyperthyroidism ). Symptoms caused by an enlarged thyroid gland ( goiter ) or other accompanying symptoms (e.g. endocrine orbitopathy ) can also make therapy necessary.
A causal treatment of the autoimmune disease is not yet known. A final (definitive) treatment of the hyperfunction is only possible with surgery or radioiodine therapy.
Medical therapy
The treatment always starts with drug therapy. Those affected are given thyreostatics , which inhibit the formation of thyroid hormones, in high doses until the laboratory values fT3 and fT4 ("peripheral euthyroidism") normalize. The aim is not to normalize the TSH value. Sulfur-containing anti-thyroid drugs ( propylthiouracil , carbimazole , thiamazole and others) are often used, but they have an effective latency of around one to two weeks. Most frequent side effects are a moderate reduction in the number of white blood cells ( leukocytes ), a moderate elevation of liver enzymes ( transaminases ), and various skin conditions ( exanthema , erythema , itching , hair loss ). Very rare but feared side effects are hepatitis , agranulocytosis and vasculitis .
Propranolol (a non-cardioselective β-receptor blocker ) is used as a supplement for palpitations ( tachycardia ), but also alleviates the non-cardiac symptoms of hyperthyroidism and inhibits the conversion (conversion) of T 4 to T 3 .
With thyroid therapy lasting 12 to 18 months, a remission occurs in about 40% of cases , so that after discontinuation of the thyroid drug there is no longer a hyperthyroid metabolic situation. Subsequently, however, it is not uncommon for an underactive thyroid to develop ( hypothyroidism ). Due to the severity of the potential side effects of thyrostatic therapy, it should not be used as long-term therapy (over 12 to 18 months). Exceptions only apply to patients who refuse definitive therapy or who are not eligible for definitive forms of therapy due to severe concomitant illnesses.
Drug treatment is mainly used in patients who have a low risk of recurrence: female patients who are over 40 years of age at the onset of the disease, have a thyroid volume below 40 ml and TSH receptor antibodies below 10 U / l. For the other patients (age at onset of the disease under 40 years or male gender or thyroid volume over 40 ml or TSH receptor antibodies over 10 U / l), an early definitive therapy is recommended because of the poor remission rate. Children have a higher rate of recurrence (around 70% within two years). It is still unclear whether this justifies a longer phase of thyrostatic treatment.
Definitive therapy
The radioiodine provides a definitive treatment is of Graves' disease. Is employed radioactive 131 iodine . Stove boxes of 200 to 300 gray are aimed for; the radiation exposure for the whole body is given as 30 to 40 mSv , which is around four powers of ten lower. Since the therapy only becomes effective after several weeks, thyreostatics must be used before and after treatment. As with the operation, the vast majority of patients subsequently develop hypothyroidism and therefore require lifelong substitution treatment using oral thyroid hormone administration. As contraindications pregnancy and lactation, the simultaneous suspicion of a valid thyroid carcinoma , and a florid endocrine ophthalmopathy. The success rate of radioiodine therapy is given as 80 to 90%, with repeat treatment with 100%.
The subtotal Strumaresektion represents a definitive therapy. In pregnant women, it is the only definitive treatment option because the radioactive iodine therapy is contraindicated because of placental transfer of iodine isotopes. The thyroid gland is removed except for a very small part. A lifelong hypothyroidism that requires treatment is deliberately brought about in order to safely eliminate the overfunction and to minimize the risk of a relapse (relapse). The (relative) contraindications are an increased risk of anesthesia and a previously operated thyroid, especially if there is already unilateral recurrent palsy . The success rate of the operation is over 95%, the recurrence rate below 10%. The complication rate is slightly higher than for operations for a goiter with or without a lump.
Therapy of endocrine orbitopathy
A causal therapy is also not known. In mild forms (dryness of the eyes with movement disorders of the eyelids), the use of tear substitutes or ointments is indicated locally .
In severe cases in which there is an existing or threatened impairment of vision, steroids are first used as long as no fibrosis has developed . In addition, radiotherapy (orbital tip irradiation: dose 2–16 Gy depending on the case ) may be necessary. Treatment of hyperthyroidism is also indicated.
If there is already fibrosis, surgical measures may be indicated. Depending on the indication, the following types of operations are carried out in rare cases:
- Reduction of pressure in the orbit - prevention of strangulation of the optic nerve and reduction of corneal exposure ,
- Eye muscle surgery - improvement of eye mobility, reduction of double vision and head posture and
- Plastic surgery on the eyelids - reducing dehydration of the eye caused by incomplete blinking and restoring a normal appearance.
Literature and Sources
Historical literature
- Robert James Graves: New observed affection of the thyroid gland in females. ( Clinical lectures. ) In: London Medical and Surgical Journal. 7, (Renshaw) 1835; 7, pp. 516-517. Reprinted in: Medical Classics. 5, 1940, pp. 33-36.
- KA von Basedow: Exophthalmus due to hypertrophy of the cell tissue in the eye socket. In: [Casper's] weekly for all medicine. Berlin 1840, 6, pp. 197-204, 220-228. English translation in: Ralph Hermon Major: Classic Descriptions of Disease. CC Thomas, Springfield 1932.
- KA von Basedow: The goggle eyes. In: [Casper's] weekly for all medicine. Berlin 1848, pp. 769-777.
- Ferdinand Sauerbruch : Lecture on Basedow's disease. In: Ferdinand Sauerbruch, Hans Rudolf Berndorff : That was my life. Kindler & Schiermeyer, Bad Wörishofen 1951; cited: Licensed edition for Bertelsmann Lesering, Gütersloh 1956, pp. 262–271.
Current literature
- Brakebusch, Heufelder, Zuckschwerdt: "Living with Basedow's Disease" A guide for those affected. Detailed explanations of symptoms, therapy, hormones and causes, 2002, ISBN 3-88603-799-1 .
- Lothar-Andreas Hotze, Petra-Maria Schumm-Draeger: Thyroid diseases. Diagnosis and therapy. Berlin 2003, ISBN 3-88040-002-4 .
- Malte H. Stoffregen: Basedow's disease. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 152.
Web links
- Competence network for immune thyroid disorders: Basedow's disease
- Basedow's disease at schilddruesenguide.de (PDF; 100 kB)
Individual evidence
- ↑ Basedow's syndrome or disease. whonamedit.com; Retrieved March 24, 2008
- ↑ www.whonamedit.com .
- ↑ a b J. Hädecke, U. Schneyer: Endocrinological findings in endocrine orbitopathy. In: Klin Monatsbl Augenheilkd. 2005; 222, pp. 15-18, doi: 10.1055 / s-2004-813646
- ^ Homepage of the city of Merseburg. ( Memento of the original from February 2, 2014 in the Internet Archive ) Info: The archive link was inserted automatically and has not yet been checked. Please check the original and archive link according to the instructions and then remove this notice. Retrieved March 24, 2008
- ↑ a b Barbara I. Tshisuaka: Basedow, Karl Adolf von. In: Werner E. Gerabek , Bernhard D. Haage, Gundolf Keil , Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 152 .
- ^ Robert James Graves . ( Memento of March 13, 2006 in the Internet Archive ) www.whonamedit.com; Retrieved March 23, 2008
- ↑ Fritz Spelsberg, Thomas Negele: Thyroid. 6th edition. S. Hirzel, Stuttgart 2005; 7th, unchanged edition, ibid 2008, ISBN 978-3-7776-1584-4 , p. 16.
- ↑ Wolfgang Wildmeister: Practical information on thyroid diagnostics. Hoechst Aktioengesellschaft 1984, p. 9 f. ( History of Thyroid Research ).
- ↑ Ferdinand Sauerbruch: That was my life. Kindler & Schiermeyer, Bad Wörishofen 1951; Licensed edition for Bertelsmann Lesering, Gütersloh 1956, p. 83 f. and 262-271.
- ^ S. Hertz, A. Roberts: Application of radioactive iodine in therapy of Grave's disease . In: J div , 21 (624) (1942) d-nb.info, accessed on March 10, 2008.
- ↑ R. Paschke u. a .: Therapy of uni- or multifocal thyroid autonomy. In: Dtsch Arztebl. , 2000; Retrieved March 10, 2008.
- ↑ Malte H. Stoffregen: Basedow's disease. In: Werner E. Gerabek, Bernhard D. Haage, Gundolf Keil, Wolfgang Wegner (eds.): Enzyklopädie Medizingeschichte. De Gruyter, Berlin / New York 2005, ISBN 3-11-015714-4 , p. 152.
- ^ J. Larry Jameson, Anthony P. Weetman (for the German edition: Jens Zimmermann and George Kahaly): diseases of the thyroid. In: Manfred Dietel, Joachim Dudenhausen, Norbert Suttorp (eds.): Harrison's internal medicine. Berlin 2003, ISBN 3-936072-10-8 .
- ^ JR Siewert, M. Rothmund, V. Schumpelick: Practice of Visceral Surgery: Endocrine Surgery. Springer, 2007, ISBN 978-3-540-22717-5 , p. 42 books.google.de
- ↑ a b c d e f g h i j k L.-A. Hotze, P.-M. Schumm-Draeger: Thyroid Diseases. Diagnosis and therapy. Berlin, 2003, ISBN 3-88040-002-4 .
- ↑ K. Mann, R. Hörmann: Antithyroid and TSH-suppressive treatment in Graves' disease? In: The internist. Springer Verlag, 1998, (39) 6, pp. 600–612, (online)
- ↑ a b c d e K.-H. Niessen: Pediatrics. Thieme Verlag, 2001, ISBN 3-13-113246-9 , pp. 242-243. books.google.de
- ↑ a b c d e f W. Siegenthaler u. a .: Siegenthaler's differential diagnosis. Thieme Verlag, 2005, ISBN 3-13-344819-6 , p. 490 ff., Books.google.de
- ↑ M. Ide u. a .: Polymorphisms of the MICA microsatellite in thyroid autoimmunity. In: Medical Clinic. Urban & Vogel, January 2007, pp. 11–15, ISSN 0723-5003 (online)
- ↑ Gerd Herold : Internal Medicine . Cologne 2005.
- ↑ Ferdinand Sauerbruch : Lecture on Basedow's disease. In: Ferdinand Sauerbruch, Hans Rudolf Berndorff : That was my life. Kindler & Schiermeyer, Bad Wörishofen 1951; cited: Licensed edition for Bertelsmann Lesering, Gütersloh 1956, pp. 262–271, here: p. 263.
- ↑ A. Heufelder: Basedow's disease and endocrine orbitopathy: consequences of new pathophysiological insights. In: K.-M. Derwahl, L.-A. Hotze (ed.): Autoimmune diseases of the thyroid. Current - Proven - Controversial. Berlin 2003
- ^ B. Müller, U. Bürgi: Akropachie bei Hyperthyreose. In: Switzerland Med Wochenschr. , 129/1999, p. 1560. smw.ch ( Memento of December 11, 2007 in the Internet Archive ) accessed on February 14, 2009
- ^ MJ Reinhardt. Radioiodine Therapy of Benign Thyroid Diseases: Graves' Disease - Current Aspects. In: Nuclear Medicine. 2005; 28, pp. 113-117 doi: 10.1055 / s-2005-836761
- ↑ F. Kaguelidou et al. a. Predictors of autoimmune hyperthyroidism relapse in children after discontinuation of antithyroid drug treatment. In: J Clin Endocrinol Metab . 2008 Oct; 93 (10), pp. 3817-3826. Epub 2008 Jul 15. PMID 18628515 doi: 10.1210 / jc.2008-0842 .
- ↑ MJ O'Doherty, PR McElhatton, SH Thomas: Treating thyrotoxicosis in pregnant or potentially pregnant women. In: BMJ. Volume 318, Number 7175, January 1999, pp. 5-6, PMID 9872862 , PMC 1114544 (free full text).
- ↑ a b c A. J. Augustin: Ophthalmology. Springer, 2007, ISBN 978-3-540-30454-8 , pp. 84-85. books.google.de
- ↑ JJ Kanski: Clinical Ophthalmology Textbook and Atlas. Urban & Fischer, 2008, ISBN 978-3-437-23471-2 , pp. 174-176. books.google.de

