Endocrine orbitopathy
| Classification according to ICD-10 | |
|---|---|
| H06.2 * | Exophthalmos in thyroid dysfunction |
| ICD-10 online (WHO version 2019) | |
The endocrine ophthalmopathy (from the Latin orbis , circle 'and ancient Greek πάθος páthos , German , passion, addiction' ; endocrine , inward releasing '; synonyms thyroid eye disease , EO ) is a disease of the eye socket ( orbit ). It is one of the organ-specific autoimmune diseases and usually occurs together with a thyroid dysfunction ( endocrine ), with women being affected significantly more often than men.
Clinically, it manifests itself with a clear protrusion of the eyes ( exophthalmos ), raised upper eyelids (eyelid retraction) and an associated widening of the eyelid fissures . Trigger for this striking symptoms are structural and image size changes behind the eyeball (retrobulbar) located muscle, fat and connective tissue .
Together with a racing heart ( tachycardia ) and an enlargement of the thyroid gland ( goiter ), the exophthalmos forms the so-called Merseburg triad , a three-part (triad) symptom complex. This is one of the classic but not mandatory clinical signs of Basedow's disease and was described as early as 1840 by Carl Adolph von Basedow , who was working in Merseburg at the time.
The course of the disease shows different degrees of severity and activity . Because of the conspicuous cosmetic appearance, the organic and functional problems can also be accompanied by strong psychosocial stress from which those affected have to suffer. Although there are a number of symptomatic treatment measures, a (causal) therapy that eliminates the causes is not yet known.
Cause and frequency
The cause of endocrine orbitopathy is still unknown. A hereditary autoimmune disease , which is responsible for the formation of autoantibodies against thyrotropin receptors (the hormone thyrotropin , TSH for short, significantly influences thyroid growth), is considered likely . These receptors are also found in the tissue of the eye socket.
Endocrine orbitopathy occurs in 10% of all thyroid patients and occurs simultaneously in up to 90% of cases in the context of Graves' disease , 60% in connection with an overactive thyroid ( hyperthyroidism ). However, there is no precise information on the frequency ( prevalence ) of Graves' disease in Germany. In areas with an adequate supply of iodine, this is reported to be 2 to 3% for women and around a tenth of it for men. The annual incidence rate of Graves' disease is 1 per 1,000 inhabitants.
However, endocrine orbitopathy can also develop before or years after the onset of thyroid disorders. Endocrine orbitopathy is therefore interpreted as a manifestation of the autoimmune processes on which Graves' disease is based outside the thyroid gland (extrathyroidal) . Thus the same causes are assumed. Play genetic predisposition , environmental influences, their meanings are not yet clear, and a complex immunological processes involved. Even with radioiodine therapy , a previously mild or clinically inapparent (inconspicuous) endocrine orbitopathy can develop or worsen significantly.
However, it is only rarely found in Hashimoto's disease or completely without evidence of thyroid involvement. Excessive nicotine consumption ( nicotine abuse ) can negatively affect the course and severity of the disease. Endocrine orbitopathy occurs six times more often in women than in men, with severe cases clearly predominating in men. Thyrotropin receptor autoantibodies (TSH receptor antibodies) correlate with the activity of the disease and help to assess the prognosis of endocrine orbitopathy.
Although endocrine orbitopathy is associated with thyroid disease in the vast majority of cases, a causal relationship has not yet been proven, which is why it is also viewed as an autoimmune disease in its own right .
The common in the English-speaking world and interchangeably used term Graves ophthalmopathy already provides a direct link between the increased incidence of this eye disease and Graves 'disease ( Engl. : Graves' disease ) ago. The Irish doctor Robert James Graves described a case of pathological enlargement of the thyroid gland ( goiter ) in combination with an exophthalmos as early as 1835 .
Disease emergence
The occurrence of endocrine orbitopathy is the result of complex defense mechanisms of the body against its own tissue ( autoimmune processes ), which are triggered by certain blood cells, so-called B and autoreactive T lymphocytes , and with an increased formation of antibodies ( thyrotropin receptor autoantibodies , TRAK) go hand in hand. There are indications that TRAKs with stimulating properties ( thyroid stimulating antibodies , TSAb) particularly favor the development of endocrine orbitopathy, but the exact mechanism is not yet known. Other receptor antibodies (e.g. the insulin-like growth factors ) could also play a role.
Compared to other areas of the body, certain connective tissue cells, so-called fibroblasts , react particularly strongly in the retrobulbar tissue to inflammatory stimuli, in particular to stimulation of special antigens, so-called CD40 proteins, which leads to the formation of new fat cells. A genetic predisposition and tobacco consumption also have a beneficial effect .
The immunological inflammation triggered in this way leads to swelling of the muscle, fat and connective tissue in the eye socket, widens the distance between the orbital wall and the eyeball and thus leads both to protrusion of the eye (exophthalmos) and to a loss of elasticity of the eye muscles with movement restrictions and Double vision. The main reasons for this process are penetration of the tissue with lymphocytes (lymphocytic infiltrations ) and an increase in fibroblasts. In addition, there is an increase in a connective tissue building material, collagen , with a simultaneous increase in other stored glycosaminoglycans and an excessive accumulation of water in the tissue. A typical appearance of the eye muscles and, more rarely, the optic nerve is also a diffuse fat tissue growth, a so-called lipomatosis .
Clinical manifestations
The endocrine orbitopathy occurs on one or both sides, but then often to different degrees. Other sources point to a more bilaterally symmetrical clinical picture. It has a number of dynamically changing clinical features, which are usually caused by inflammation , structural changes and an increase in volume of orbital fat , connective and muscle tissue located behind the eye ( see also: Periorbita ). If the endocrine orbitopathy is so pronounced that it is no longer possible to close the eyelid completely ( lagophthalmos ) and corneal ulcers therefore occur, it is called malignant exophthalmos .
Like other diseases, endocrine orbitopathy can put a lot of psychological strain on those affected. In addition to the general complaints, the functional restrictions caused by double vision and forced head postures, which can usually represent clear obstacles in many areas of life, the cosmetic-aesthetic aspect can lead to social withdrawal .
Eye socket (orbit)
The exophthalmos , the emergence of one or both eyes from the eye socket is, the classic symptom of endocrine ophthalmopathy and the result of a painful proliferation of retrobulbar tissue that extends into the eyelids can protrude. In 3% of the cases there is also swelling of the soft tissue in the tip of the orbit (e.g. edema ) and as a result compression and thus damage to the optic nerve with deterioration in visual acuity and corresponding visual field defects .
The extent of the exophthalmos can be quantified with an ophthalmological examination device, the so-called exophthalmometer , and thus also allows the course and status to be documented. Space-consuming processes and space conditions in the orbit can be visualized with imaging methods ( ultrasound , CT , NMR ). An examination of the field of vision and visual acuity is carried out using perimetry and eye tests .
Eye muscles
Movement disorders arise from swelling , infiltration or pathological tissue proliferation ( fibrosis ) of the eye muscles , whereby an enlargement of up to ten times its usual volume is possible. As a result, there is a loss of elasticity with, in some cases, significantly reduced elasticity, often accompanied by pain when looking around. The movement restrictions do not appear in the direction of muscle pull as an expression of reduced muscle strength, but in the opposite direction, which is more or less an apparent paralysis ( pseudoparesis ) of the muscular opponent ( antagonist ) on the same side . Clinical signs, for example, are the restriction of the monocular fields of vision , strabismus and double vision with compensatory head postures . Another typical symptom is the so-called Möbius sign , a sometimes pronounced inability to move both eyes towards the nose at the same time ( weak convergence ).
Different motility examinations and the determination of the areas in which one can simply see with both eyes without double images ( fusion fields of view ) are usually carried out using a so-called synoptometer or in free space on the tangent table (according to Harms). To determine the maximum mobility of the right and left eye (monocular excursion routes) , an examination of the subsequent movements on the Goldmann perimeter can also be carried out. A forceps pull test provides information about the passive mobility of the eye. Since when looking in the opposite direction to the pulling direction of a fibrosed muscle there is a short-term increase in intraocular pressure , it can be useful to carry out intraocular pressure measurements in different directions of view ( gaze tonometry ). Muscle structures and dimensions can be represented by imaging methods.
Eyelids
Usually the upper eyelid is withdrawn ( retraction ), which gives the impression of a stare ( Kocher's sign ). The white skin of the eye ( sclera ) is often visible above the transition ( limbus ) to the cornea ( Dalrymple sign ), and the upper eyelid remains behind when looking down ( Graefe sign ). A seldom blinking of the eye ( Stellwag sign ) often leads to wetting disorders of the cornea as well as dehydration and chemosis of the conjunctiva .
To document progress and status, the width of the eyelid gap (space between the upper and lower eyelid) and mobility can be assessed with a simple ruler and is given in millimeters. The frequency of the blinking of an eye is expressed in numbers per minute.
Other clinical signs
Additional symptoms of endocrine orbitopathy include upper eyelid edema (Enroth's sign), difficult ectropioning (Gifford's sign), abnormal upper eyelid pigmentation (Jellinek's sign), horizontal eyelid furrow (Pocher sign), lack of frowning when looking up (Joffroy sign) and Lid tremors with closed lids (Rodenbach sign).
Diagnosis
The diagnosis is primarily made clinically. In the classic case, exophthalmos occurs as part of the so-called Merseburg triad together with an enlarged thyroid and an accelerated heartbeat in the context of Graves' disease .
Further diagnostic measures primarily serve to record the severity and activity level of the disease, as well as impending complications. The investigation by means of nuclear magnetic resonance spectroscopy ( NMR ) is particularly suitable for estimating the inflammatory activity .
In terms of differential diagnosis , various imaging methods ( computed tomography , NMR ) can be used to exclude not only a tumor located behind the eye, but also the clinical picture of ocular myositis . It is difficult to differentiate from endocrine orbitopathy (Graves ophthalmopathy) the, so far largely not understood, idiopathic orbital inflammation and the isolated immunogenic orbitopathy . Both are ultimately diagnoses of exclusion in the absence of evidence of endocrine involvement.
There are various schemes for classifying the course and stage of the disease, none of which, however, has finally established itself as a standard. The so-called NOSPECS scheme , a classification of the American Thyroid Association, has been in use since 1969 . The letter sequence is a special abbreviation ( acronym ) for the English names of the queried symptoms. It is also known as the Werner classification by the name of its developer, the US doctor Sidney C. Werner . Within this classification there is a further classification according to the severity levels 0, A, B and C, with which a certain point value can be determined. Together with another parameter for disease activity , the so-called CAS score (according to Mourits ), the entire course of the disease is assessed.
As an extension of the NOSPECS scheme, the so-called LEMO classification has established itself, which should contain a more meaningful and more practicable classification and was first proposed by Boergen and Pickardt in 1991 . This is a so-called facet classification . The division is made with the preceding letter and a following number. L 1 E 2 M 0 O 2 stands for “only eyelid edema, conjunctival irritation in the morning, missing muscle changes and peripheral visual field defects”.
These schemes are an important aid before and during the treatment in order to be able to assess the progression or a therapy-related improvement of the clinical picture in a meaningful way. They also provide a clear overview of the importance of important symptoms.
| class | clinical features | English name |
|---|---|---|
| 0 | no signs or symptoms | N o signs or symptoms |
| 1 | Signs (e.g. eyelid retraction), not symptoms | O nly signs, no symptoms |
| 2 | Soft tissue involvement | S often tissue involvement |
| 3 | Exophthalmos | P roptosis |
| 4th | Muscle changes | E xtraocular muscle involvement |
| 5 | Corneal complications | C orneal involvement |
| 6th | Visual and visual field restrictions | S ight loss |
| Symptoms | class | Finding |
|---|---|---|
|
Changes in the eyelids ( L ) |
0 | missing |
| 1 | only eyelid edema | |
| 2 | real retraction (impaired lid closure) | |
| 3 | Retraction plus upper eyelid edema | |
| 4th | Retraction plus upper and lower eyelid edema | |
| Exophthalmos ( E ) | 0 | missing |
| 1 | without lid closure insufficiency | |
| 2 | Conjunctival irritation in the morning | |
| 3 | Conjunctival irritation constantly | |
| 4th | Corneal complications | |
|
Changes in the muscles ( M ) |
0 | missing |
| 1 | only detectable with imaging methods | |
| 2 | Pseudoparesis | |
| 3 | Pseudoparalysis | |
|
Involvement of the optic nerve ( O ) |
0 | missing |
| 1 | only in color vision and in VEP | |
| 2 | peripheral visual field defects | |
| 3 | central visual field defects |
Therapy and prognosis
A ( causal ) therapy that eliminates the causes is not yet known. However, in many cases it is possible to treat the symptoms . Cortisone preparations are the first choice. In cases in which their effect is unsatisfactory, additional measures can be taken, but their use is not based on empirically proven effectiveness ( evidence-based ) due to pending scientific studies . The effectiveness of the therapy can be improved through the cooperation of several medical specialties ( interdisciplinary - internal medicine , radiation therapy , ophthalmology and specialized surgeon ). In cases of particular psychological stress due to the illness, support from psychologists can be helpful. Despite professional therapy, there is an improvement in only 30% of the patients, in 60% nothing changes, and in 10% a deterioration occurs.
Conservative treatment
Conservative treatment measures generally depend on the severity and degree of activity of the disease and are primarily aimed at inhibiting or reducing inflammatory processes. Little information has been given in the literature about the direct improvement in eye motility through conservative forms of treatment. If the squint angle is not too large, special prismatic glasses can be used to bridge the gap between the double images .
Psychosomatic care is indicated in around half of all patients with pronounced endocrine orbitopathy . In addition to improving the organic and functional situation, the basic aim of treatment is to achieve the best possible restoration of the patient's external appearance and reintegration into their professional and private environment.
Medication
Local treatment with tear substitutes or ointments may be sufficient for mild forms that are only associated with dryness of the eyes or slight conjunctival irritation .
In moderate to severe cases in which there is an existing or threatened impairment of vision, cortisone preparations , usually administered intravenously, are the first choice. Concomitant treatment of the thyroid dysfunction is of course necessary. Cortisone preparations have proven themselves in active inflammatory processes because of their rapid effectiveness on swelling. In the case of severe disease progression, intravenous, high-dose treatment can be recommended. However, there are a number of side effects (weight gain, mood swings , stomach problems ) and contraindications ( diabetes mellitus , infectious diseases , psychoses , stomach ulcers , osteoporosis ).
Possible combinations
In cases in which the initially initiated cortisone therapy fails, there is currently no consensus on the optimal follow-up treatment. The use of a second cortisone treatment with radiation or cyclosporine appears to be promising. The selection of additional procedures depends on the experience of the treating physicians, as there are currently no evidence-based recommendations in this area.
Experimental treatment approaches
Other methods in the experimental stage are biotechnologically produced drugs ( biologics ), in particular the active ingredient rituximab .
Prevention with radio-iodine therapy
As a preventive measure, the administration of prednisolone is recommended when performing radioiodine therapy . However, what constitutes an optimal dosage is debatable.
Irradiation
Irradiation is recommended in addition, together with another cortisone attack, if the first one has not been sufficiently successful. However, evidence-based recommendations are still lacking. It is carried out in the form of orbital tip irradiation with a diagnosis-dependent dose of 2–16 Gy . This has the advantage that, in contrast to cortisone administration, there are significantly fewer side effects. However, the overall effect is less and it takes longer to occur. Recent studies have shown that lower doses (1 Gy / week), staggered over a longer treatment interval (10-20 weeks), can be just as effective as the use of higher doses over shorter periods of time (4 times / week 2 Gy to a maximum of 12 Gy total dose).
Botulinum toxin
As a treatment with a limited duration of action, the nerve toxin botulinum toxin can be injected into the affected external eye muscle or the tarsalis muscle (Müllerian muscle - eyelid lifter) to reduce double vision or upper eyelid retraction, thus causing these muscles to relax temporarily. However, no permanent damage to the structures due to fibrosis should have occurred.
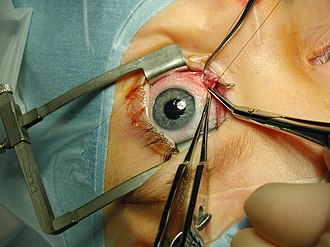
Operations
Surgical interventions are only carried out in the inactive, chronic fibrotic phase of the disease and after a constant finding has existed for a period of at least six months. The sequence of measures, according to which first the orbit, then the external eye muscles and finally the eyelids are treated, must be observed. There should be a few months between each operation.
Orbit
Operations on the eye socket are carried out as a relief measure, on the one hand to treat an impending or already occurred entrapment of the optic nerve. They come into consideration when all conservative therapy options have been exhausted, or as emergency care in the event of an acute crushing of the optic nerve. On the other hand, they are also performed for cosmetic and aesthetic reasons, to treat a conspicuous exophthalmos and to reposition the eyeball in the orbit. Here, however, the disease must have taken a stable course for about six months without further progression and without acute inflammatory processes.
There are different methods of pressure relief (decompression). Either fatty tissue is removed directly, or space is created in which the tissue can expand by removing the lateral or lower bony orbital boundaries. Removal of the orbital ceiling is rare because of the close proximity to the interior of the skull. Depending on the access route to the operating area and the technique of the procedure used, surgical interventions are eye and / or ENT surgery and can therefore represent an interdisciplinary treatment strategy.
Like other surgeries, orbital decompression procedures are not without risk. In some cases there may be complications with impaired sensation in the face or an increased squint of the eyes. In very rare cases, injuries to the eye can also occur.
Eye muscles
The aim of eye muscle operations in endocrine orbitopathy is to achieve a normalization of the eye mobility with the largest possible field of simple vision with both eyes, and this without adopting a compensatory head posture. The success rate is between about 60-80% freedom from double images in the normal field of vision . Since squint positions and restricted mobility are due to a lack of flexibility and structural changes in the muscles, the procedural principles and dosage guidelines of normal squint operations can only be used to a very limited extent in such operations. Which muscles are ultimately treated surgically with which technique depends on the individual clinical picture and the respective findings. Careful dosing is particularly necessary to avoid overcorrections. For this reason, several operations, even on both eyes, may well be indicated.
Usually one will return transfer of fibrotic muscle performed. This can be done with or without a firm reattachment ( refixation ) of the muscle to the globe . In the second case there is the possibility of influencing the effect of the operation by readjusting the threads up to the first postoperative day. As a dosage guideline, it was suggested to use a squint angle reduction of 2 ° per millimeter of muscle repositioning as a basis for surgery on the vertical straight eye muscles, and 1.7 ° per millimeter of repositioning distance for surgery on horizontal straight eye muscles. The recommendation of pure repositioning does not apply to very large squint angles.
Eyelids
In terms of time , eyelid operations are last in the series of surgical therapeutic measures for endocrine orbitopathy. They can be considered if this makes sense for cosmetic and aesthetic reasons due to permanent retraction of the upper eyelid, especially when looking down, or if there is a risk of corneal drying out due to incomplete eyelid closure .
As a rule, a weakening procedure is performed on the lifter of the eyelid, the levator palpebrae superioris muscle . Further procedures are the upper and lower eyelid lengthening and lateral eyelid gap reduction .
Health economic aspects
Although there are no specific health economic data relating to endocrine orbitopathy, it is assumed that it causes very high direct and indirect costs. On the one hand, these are due to the complex and interdisciplinary therapeutic measures, the possibly very long or therapy-resistant course of the disease, and correspondingly intensive follow-up care. On the other hand, sick leave can lead to long absence from work or even permanent inability to work . The establishment of specialized centers and increased research, especially in the genetic field, are seen as an approach to developing more targeted and efficient treatment measures and thus reducing costs without counteracting the primary goal of optimal patient care.
literature
- Herbert Kaufmann (Ed.): Strabismus. With the collaboration of Wilfried de Decker u. a. 3rd, fundamentally revised and expanded edition. Georg Thieme, Stuttgart a. a. 2004, ISBN 3-13-129723-9 .
- Theodor Axenfeld (founder), Hans Pau (ed.): Textbook and atlas of ophthalmology. 12th, completely revised edition. With the collaboration of Rudolf Sachsenweger a . a. Gustav Fischer, Stuttgart a. a. 1980, ISBN 3-437-00255-4 .
Web links
- Guideline No. 28 of the Professional Association of Ophthalmologists in Germany (BVA) and the German Ophthalmological Society (DOG): Orbital diseases / exophthalmos
- Katharina A. Ponto, Susanne Pitz, Norbert Pfeiffer, Gerhard Hommel, Matthias M. Weber, George J. Kahaly: Endocrine Orbitopathy - Quality of Life and Occupational Stress . (PDF) In: Deutsches Ärzteblatt. Volume 106, issue 17, April 24, 2009 (PDF)
- Announcement by the German Society for Endocrinology, Volume 27 - Issue 2/2003 (PDF; 1.3 MB)
Individual evidence
- ↑ a b c d Gerd Herold : Internal Medicine 2007. A lecture-oriented presentation. Self-published, Cologne 2007, pp. 674–675.
- ↑ a b c d e f g Information on endocrine orbitopathy, Center for Ophthalmology at the Essen University Hospital
- ↑ a b c d e f g Albert J. Augustin: Ophthalmology. 3rd, completely revised and expanded edition. Springer, Berlin a. a. 2007, ISBN 978-3-540-30454-8 , pp. 84-85.
- ^ AJ Dickinson: Clinical manifestations. In: Wilmar M. Wiersinga, George J. Kahaly (Eds.): Graves' orbitopathy. A multidisciplinary approach. Karger, Basel a. a. 2007, ISBN 978-3-8055-8342-8 , pp. 1-26.
- ^ J. Larry Jameson, Anthony P. Weetman (for the German edition: Jens Zimmermann and George Kahaly): diseases of the thyroid. In: Manfred Dietel, Joachim Dudenhausen, Norbert Suttorp (eds.): Harrison's internal medicine. 15th edition, German edition, special edition. Lehmanns Media LOB.de u. a., Berlin a. a. 2003, ISBN 3-936072-10-8 .
- ↑ Jörg Rüdiger Siewert , Matthias Rothmund , Volker Schumpelick (eds.): Practice of visceral surgery. Endocrine surgery. Springer Medicine, Berlin a. a. 2007, ISBN 978-3-540-22717-5 , p. 42 .
- ↑ GB Bartley, V. Fatourechi, EF Kadrmas, SJ Jacobsen, DM Ilstrup, JA Garrity, CA Gorman: Chronology of Graves' ophthalmopathy in an incidence cohort. In: American Journal of Ophthalmology. Vol. 121, No. 4, 1996, ISSN 0002-9394 , pp. 426-434, PMID 8604736 .
- ↑ a b c d J. Hädecke, U. Schneyer: Endocrinological findings in endocrine orbitopathy. In: Clinical monthly sheets for ophthalmology. Vol. 222, No. 1, 2005, ISSN 0023-2165 , pp. 15-18, doi: 10.1055 / s-2004-813646 .
- ^ A b Sally R. James, Aaron M. Ranasinghe, Rajamiyer Venkateswaran, Christopher J. McCabe, Jayne A. Franklyn, Robert S. Bonser: Lower Dose Prednisone Prevents Radioiodine-Associated Exacerbation of Initially Mild or Absent Graves' Orbitopathy: A Retrospective Cohort Study. In: The Journal of Clinical Endocrinology and Metabolism . Vol. 95, No. 3, 2010, ISSN 0021-972X , pp. 1333-1337, doi: 10.1210 / jc.2009-2130 , PMID 20061414 .
- ↑ Katharina A. Ponto, George J. Kahaly: Endocrine Orbitopathy - Current Diagnostics and Therapy. In: Medical Clinic. Vol. 103, No. 10, 2008, ISSN 0723-5003 , pp. 717-730, doi: 10.1007 / s00063-008-1112-1 , quoted from Katharina A. Ponto, Susanne Pitz, Norbert Pfeiffer, Gerhard Hommel, Matthias M. Weber, George J. Kahaly: Endocrine orbitopathy: quality of life and occupational stress. In: Deutsches Ärzteblatt International. Vol. 106, No. 17, 2009, ISSN 1866-0452 , pp. 283-289, doi: 10.3238 / arztebl.2009.0283 .
- ^ A b U. Hennighausen: For the annual conference of the Saxon Ophthalmological Society. About conservative therapy for endocrine orbitopathy. In: The ophthalmoscope. Forum of ophthalmologists. Vol. 55, No. 4, ISSN 0004-7937 , p. 8 ff.
- ↑ a b A. Eckstein, M. Plicht, N. Morgenthaler, KP Steuhl, K. Renzing-Koehler, B. Quadbeck, K. Mann, J. Esser: The TSH receptor antibodies help to assess the prognosis of an endocrine orbitopathy. 101st annual meeting of the DOG (German Ophthalmological Society) 2003.
- ↑ Search for "Graves". In: Fritz-Jürgen Nöhring : specialist dictionary medicine. German English. 3rd, heavily revised and enlarged edition. Langenscheidt u. a., Berlin a. a. 2003, ISBN 3-86117-185-6 .
- ^ RJ Graves: New observed affection of the thyroid gland in females. (Clinical lectures). In: The London Medical and Surgical Journal. NS Vol. 7, 1835, ZDB -ID 422792-x , pp. 516-517; Reprinted in Medical Classics. Vol. 5, 1940/1941, ZDB -ID 604496-7 , pp. 33-36.
- ↑ Anja K. Eckstein, Marco Plicht, Hildegard Lax, Herbert Hirche, Beate Quadbeck, Klaus Mann, Klaus P. Steuhl, Joachim Esser, Nils G. Morgenthaler: Clinical results of anti-inflammatory therapy in Graves' ophthalmopathy and association with thyroidal autoantibodies . In: Clinical Endocrinology. Vol. 61, No. 5, November 2004, ISSN 0300-0664 , pp. 612-618, doi: 10.1111 / j.1365-2265.2004.02143.x , PMID 15521965 .
- ↑ a b A. K. Eckstein, KTM Johnson, M. Thanos, J. Esser, M. Ludgate: Current insights into the pathogenesis of Graves' orbitopathy. In: Hormone and Metabolic Research. Vol. 41, No. 6, 2009, ISSN 0018-5043 , pp. 456-464, doi: 10.1055 / s-0029-1220935 , PMID 19530272 .
- ↑ a b c d e f Franz Grehn: Ophthalmology. 30th, revised and updated edition. Springer, Heidelberg 2008, ISBN 978-3-540-75264-6 , pp. 324-325 .
- ↑ Hanns Kaiser , Hans K. Kley: Cortisontherapie. Corticoids in clinic and practice. 11th, revised edition. Georg Thieme, Stuttgart a. a. 2002, ISBN 3-13-357211-3 , pp. 267-268.
- ^ A b Kai Joachim Bühling, Julia Lepenies, Karsten Witt: Intensive course: General and special pathology. 3rd, updated and expanded edition. Elsevier, Urban & Fischer Verlag, Munich a. a. 2004, ISBN 3-437-42411-4 , p. 249.
- ↑ a b G. Kommerell: Endocrine orbitopathy. In: Herbert Kaufmann (Ed.): Strabismus. With the collaboration of Wilfried de Decker u. a. Enke, Stuttgart 1986, ISBN 3-432-95391-7 , pp. 395-397, here p. 396.
- ↑ Endocrine orbitopathy . In: Roche Lexicon Medicine. last seen on June 20, 2013.
- ^ I. Coulter, S. Frewin, GE Krassas, P. Perros: Psychological implications of Graves' orbitopathy. In: European Journal of Endocrinology. Vol. 157, No. 2, 2007, ISSN 0804-4643 , pp. 127-131, doi: 10.1530 / EJE-07-0205 .
- ↑ a b c Katharina A. Ponto, Susanne Pitz, Norbert Pfeiffer, Gerhard Hommel, Matthias M. Weber, George J. Kahaly: Endocrine orbitopathy: quality of life and occupational stress. In: Deutsches Ärzteblatt International. Vol. 106, No. 17, 2009, pp. 283–289, doi: 10.3238 / arztebl.2009.0283 .
- ↑ Peter Berlit (Ed.): Clinical Neurology. Springer, Berlin a. a. 1999, ISBN 3-540-65281-7 , pp. 376-378.
- ↑ a b c d e f Operative and non-operative treatment options at basedow.ch (interdisciplinary group of specialists from public hospitals and private clinics, Switzerland)
- ↑ Guideline No. 28 of the professional association of ophthalmologists in Germany, BVA, on orbital diseases / exophthalmos
- ↑ a b c d e f g Herbert Kaufmann (Ed.): Strabismus. 3rd, fundamentally revised and expanded edition. 2004, p. 428 ff.
- ↑ a b c d e f g h i j Theodor Axenfeld (first), Hans Pau (ed.): Textbook and atlas of ophthalmology. 12th, completely revised edition. 1980.
- ↑ a b E. Heufelder, D. Schworm, C. Hofbauer: The endocrine orbitopathy: current status on pathogenesis, diagnosis and therapy. In: Deutsches Ärzteblatt. Vol. 93, No. 20, 1996, pp. A-1336-A1342.
- ↑ Eberhard Kirsch, Beat Hammer, Georg von Arx: Graves' orbitopathy: current imaging procedures. In: Swiss Medical Weekly. Vol. 31, No. 43/44 = No. 139, October 2009, ISSN 1424-7860 , pp. 618-623, online (PDF; 526 KB) , PMID 19950023 .
- ^ Ward R. Bijlsma, Rachel Kalmann: Idiopathic Orbital Inflammation and Graves Ophthalmopathy. In: Archives of Ophthalmology. Vol. 128, No. 1, 2010, ISSN 0003-9950 , pp. 131-132, doi: 10.1001 / archophthalmol.2009.324 .
- ↑ KP Boergen, CR Pickardt: New classification of endocrine orbitopathy. In: The Medical World. Vol. 42, 1991, ISSN 0025-8512 , pp. 72-76.
- ↑ Navid Ardjomand, Gertrud Esche, Susanne Lindner, Manuela Panzitt, Reingard Aigner, Andrea Berghold, Andrea Langmann: The importance of octreotid scintigraphy in the diagnosis of active endocrine orbitopathy. In: Spectrum of Ophthalmology. Vol. 15, No. 3, 2001, ISSN 0930-4282 , pp. 113-116, doi: 10.1007 / BF03162928 .
- ↑ Georg J. Kahaly, Peter Bumb, Susanne Pitz, Christoph Scheurle, Katharina A. Ponto, Kathrin Lingl, Gerhard Hommel, Wibke Müller-Forell, Matthias M. Weber, Wolf J. Mann: Operative relief for endocrine orbitopathy. In: Medical Clinic. Vol. 102, No. 9, 2007, ISSN 0723-5003 , pp. 714-719, doi: 10.1007 / s00063-007-1097-1 .
- ↑ K.-P. Boergen: Ophthalmological diagnosis in autoimmune orbitopathy. In: Experimental and Clinical Endocrinology & Diabetes. Vol. 97, No. 2/3, 1991, ISSN 0947-7349 , pp. 235-242, doi: 10.1055 / s-0029-1211071 .
- ↑ a b c d e L. Bartalena: What to do for moderate-to-severe and active Graves' orbitopathy if glucocorticoids fail? . In: Clin Endocrinol. (Oxf). 2010 Feb 10, PMID 20148907
- ↑ Jack J. Kanski: Clinical Ophthalmology. Textbook and atlas. 6th, updated and expanded edition. Elsevier, Urban & Fischer, Munich a. a. 2008, ISBN 978-3-437-23471-2 , pp. 174-176.
- ↑ Kristian TM Johnson, Andrea Wittig, Christian Loesch, Joachim Esser, Werner Sauerwein, Anja K. Eckstein: A retrospective study on the efficacy of total absorbed orbital doses of 12, 16 and 20 Gy combined with systemic steroid treatment in patients with Graves' orbitopathy. In: Graefe's Archive for Clinical and Experimental Ophthalmology. Vol. 248, No. 1, 2010, ISSN 0721-832X , pp. 103-109, doi: 10.1007 / s00417-009-1214-3 , PMID 19865824 .
- ↑ Surgical rehabilitation for endocrine orbitopathy. on: Forum Thyroid e. V.